Vitamin D Replacement Effect on Platelet Counts
By Murat Bulent Kucukay, Recep AlanliAffiliations
doi: 10.29271/jcpsp.2021.09.1064ABSTRACT
Objective: To determine the effect of vitamin D treatment on platelet counts according to age groups in patients with vitamin D deficiency.
Study Design: An observational study.
Place and Duration of Study: Outpatient Clinics, Department of Internal Medicine, Faculty of Medicine, Lokman Hekim University Hospital, Ankara, Turkey from January 1st to December 31st, 2020.
Methodology: A total of 1,230 participants, who were treated for vitamin D deficiency after admission to hospital for various reasons, were enrolled. Patients under 18 years of age, having chronic diseases, using medicines affecting platelets and who had 25-hydroxyvitamin D levels above 74.88 nmol/L were excluded from study. Participants were divided into three groups according to ages: 18 to 30 (Group 1), 30 to 50 (Group 2), and greater than 50 years (Group 3). Complete blood count parameters and vitamin D level data before and after vitamin D replacement treatment were compared.
Results: Platelet counts and mean platelet volume levels were found to be significantly lower in participants after vitamin D treatment. Changes in hemoglobin and neutrophil counts were insignificant. Although there was no difference between mean platelet counts and age groups before treatment, significant differences were noted after vitamin D treatment (p=0.004). Correlation between vitamin D levels and changes in platelet levels compared to treatment beginning was found to be significant (r=-0.159, p<0.001).
Conclusion: Vitamin D treatment lowered platelet counts. This may be beneficial in medical conditions such as essential thrombocythemia in which platelet counts are higher than normal, and may help decrease platelet counts.
Key Words: Complete blood count, Blood platelet count, Vitamin D.
INTRODUCTION
Vitamin D deficiency is a worldwide health problem and affects approximately one billion people.1 Vitamin D has many different functions in the body and exerts its effects through intracellular vitamin D receptors. Active form of vitamin D; 1-alpha, 25-dihydroxyvitamin D, has steroid like hormone effects; it has roles in bone and calcium metabolism, cell growth and differentiation and immune system regulation.2
Mature megakaryocte grow in cytoplasm and nucleus, and produces platelets. Both platelets and megakaryocytes have been shown to express vitamin D receptors.3 Thus, it is proposed that vitamin D is necessary in maturation of platelets. Platelets do not have nuclei and they cannot produce vitamin D receptor proteins. Because of this, they obtain vitamin D receptor proteins, while maturating in megakaryocytes.3
Platelet counts may be affected by gender, ethnical origins and environmental factors. Platelet levels remain stable, if there is no affecting factors.4 There are few studies reporting effect of vitamin D levels on platelet counts. Inverse relationships between vitamin D levels and platelet counts were reported by these studies.5-7 The effect of vitamin D treatment on platelet counts is not clearly known; and previous studies could not enlighten this issue enough. Thus, this study was conducted to determine the effect of vitamin D treatment on platelet counts.
METHODOLOGY
This retrospective observational study was conducted with 1,230 participants meeting inclusion criteria, out of 1,925 patients who were treated for vitamin D deficiency, between January 1st and December 31st, 2020.
Patients who attended Outpatient Clinic of Lokman Hekim University Ankara Hospital with tiredness, fatigue, myalgia, back pain complaints were tested for vitamin D deficiency. Patients who were diagnosed to have vitamin D deficiency and who were given vitamin D replacement treatment; and patients who accepted to participate, were enrolled on the study.
Patients under 18 years of age, or having chronic pulmonary obstructive diseases, coronary artery disease, stroke history, chronic liver diseases, chronic renal failure, malignancies, acute infections, or those using agents such as non-steroid anti-inflammatory drugs, anti-coagulants, acetylsalicylic acid, and those who had 25-hydroxyvitamin D levels above 74.88 nmol/L were excluded from the study. Informed written consents were obtained from all of the patients who participated in the study. This study, approved by local ethics committee, was conducted in concordance with Declaration of Helsinki and good clinical practices directives.
Complete blood count parameters and 25-hydroxyvitamin D levels before treatment and three months after vitamin D treatment were recorded. Blood samples were obtained after 12 hours of fasting. Complete blood counts (neutrophil count, mean platelet volume (MPV) and hemoglobin level) were analysed using XN-1000 analyser (USA). 25-hydroxyvitamin D was measured by high pressure liquid chromatography on the Roche Hitachi Cobas 601 (Switzerland) analyser.
According to national treatment guide,8 provided by Turkish Society of Endocrinology and Metabolism, participants having 25-hydroxyvitamin D levels below 49.92 nmol/L were treated by loading dose of vitamin D, that is taken as 50,000 IU weekly for six weeks orally and then followed by 1800 IU/day vitamin D, as maintaining dose. Participants having 25-hydroxyvitamin D levels between 49.92 to 74.88 nmol/L were treated by 1800 IU/day vitamin D orally as maintaining dose for vitamin D deficiency.
Participants were divided into three groups according to ages: 18 to 30 (Group 1), 30 to 50 (Group 2), and greater than 50 years (Group 3). Complete blood count parameters of groups before and after vitamin D replacement treatment were compared between each other.
All data were evaluated using the statistical software SPSS for Windows (version 25, SPSS, Armonk, NY, USA). Data distributions were evaluated by Kolmogrov-Smirnov test. Quantitative data were presented as mean ± standard deviation for normally distributed variables. Categorical data were presented as frequency and percentage. Comparisons between groups were done by paired samples t-test and Independent samples t-tests. One-way ANOVA test was used to evaluate difference among groups greater than two. Pearson's correlation analysis was used to evaluate associations between two variables. A p value below 0.05 was considered significant.
RESULTS
After three months of vitamin D replacement treatment, platelet counts were found to be significantly lower in participants compared to the beginning of treatment. Increase in 25-hydroxyvitamin D levels and decrease in MPV levels were significant, but changes in hemoglobin and neutrophil counts were insignificant. Blood parameters before and after three months of vitamin D treatment were shown in Table I. The study was conducted with 1,230 patients; 282 (22.9%) patients were males and 948 (77.1%) patients were females. The mean age of patients was 41.47 ± 15.10 years (46 ± 14.39 for males, 40.13 ± 15.05 for females). Prior to vitamin D replacement treatment, mean vitamin D levels for males was 43.46 ± 17.59 nmol/L and 38.89 ± 19.37 nmol/L for females, which was statistically significant (p<0.001).
Platelet counts before and after vitamin D treatment, according to age groups, were shown in Table II. Although there was no difference between mean platelet counts and age groups before treatment, significant differences were noted after vitamin D treatment (p=0.004). Platelet changes with treatment, according to age groups, were shown in Figure 1.
Before treatment, 334 patients (27.2%) had serious vitamin D deficiency (below 24.96 nmol/L), 491 (39.9%) had vitamin D deficiency (24.96 to 49.92 nmol/L), and 405 (32.9%) had vitamin D insufficiency (49.92 to 74.88 nmol/L). After three months of vitamin D treatment, only 66 (5.4%) had serious vitamin D deficiency, 267 (21.7%) had vitamin D deficiency, 434 (35.3%) had vitamin D insufficiency, and 463 (37.6%) had sufficient vitamin D levels over 74.88 nmol/L. After vitamin D treatment in 161 patients (13.1%), vitamin D levels were found to be lower than beginning (treatment failure).
There was no correlation between vitamin D levels and platelet counts before treatment (r=-0.053, p=0.062). But correlation between vitamin D levels and changes in platelet levels compared to treatment beginning was found to be significant in Pearson correlation analysis (r=-0.159, p<0.001). There was a significant and inverse relationship between vitamin D levels and changes in platelet counts (Figure 2).
DISCUSSION
In this study, participants were treated for vitamin D deficiency for three months and changes in platelet counts before and after treatment were compared. Platelet counts and MPV levels were found to be lower after treatment. In addition, there was an inverse and significant relationship between vitamin D levels and changes in platelet counts.
There are studies reporting higher platelet counts in people who have vitamin D deficiency.5-7 Two of these studies inspected general population in adult ages and one inspected obese and overweight people. Vitamin D was reported to affect hematopoietic cell proliferation and differentiation.9 Patients with essential thrombocythemia had lower vitamin D levels compared to normal population.10 These studies inspected the relationship between vitamin D levels and platelet counts; but to the best knowledge of the authors of this article, changes in platelet counts with vitamin D replacement treatment was not inspected before in people who did not have any chronic diseases that might affect platelet counts. According to the results of this study, platelet counts were found to be decreased after vitamin D treatment.
Inverse relationship between vitamin D levels and platelet counts was explained by anti-thrombogenic, anti-inflammatory, anti-oxidant and anti-coagulant activity of vitamin D.5 Vitamin D has anti-oxidant activity as reported before11 and previously anti-oxidant supplementation was reported to decrease platelet counts.12
Table I: Blood parameters of participants before and after vitamin D treatment.|
Parameter |
Before |
Three months after |
p-value |
|
Hemoglobin (g/L) |
133.5±17.0 |
133.5±16.5 |
0.969 |
|
Neutrophil counts (x109/L) |
4.56±1.82 |
4.70±2.76 |
0.054 |
|
25-hydroxyvitamin D (nmol/L) |
39.94±19.06 |
72.52±40.26 |
<0.001 |
|
Platelet counts (x109/L) |
276.73±73.75 |
251.10±63.79 |
<0.001 |
|
Mean platelet volume (fL) |
10.38±0.94 |
10.32±0.91 |
0.002 |
Table II: Platelet counts before and after vitamin D treatment, according to age groups.
|
Age group and count (n) |
Initial mean platelet value (x109/L) |
p value |
Age group and count (n) |
Mean platelet value after treatment (x109/L) |
p value |
|
Group 1 (338) |
278.23±64.73 |
0.221 |
Group 1 (338) |
248.76±56.8 |
0.001*
|
|
Group 2 (555) |
279.39±76.25 |
Group 2 (555) |
258.01±67.38 |
||
|
Group 3 (337) |
270.83±77.81 |
Group 3 (337) |
242.09±63.22 |
||
|
p=0.035 between group 1 and 2, p=0.172 between group 1 and 3, and p<0.001 between group 2 and 3. |
|||||
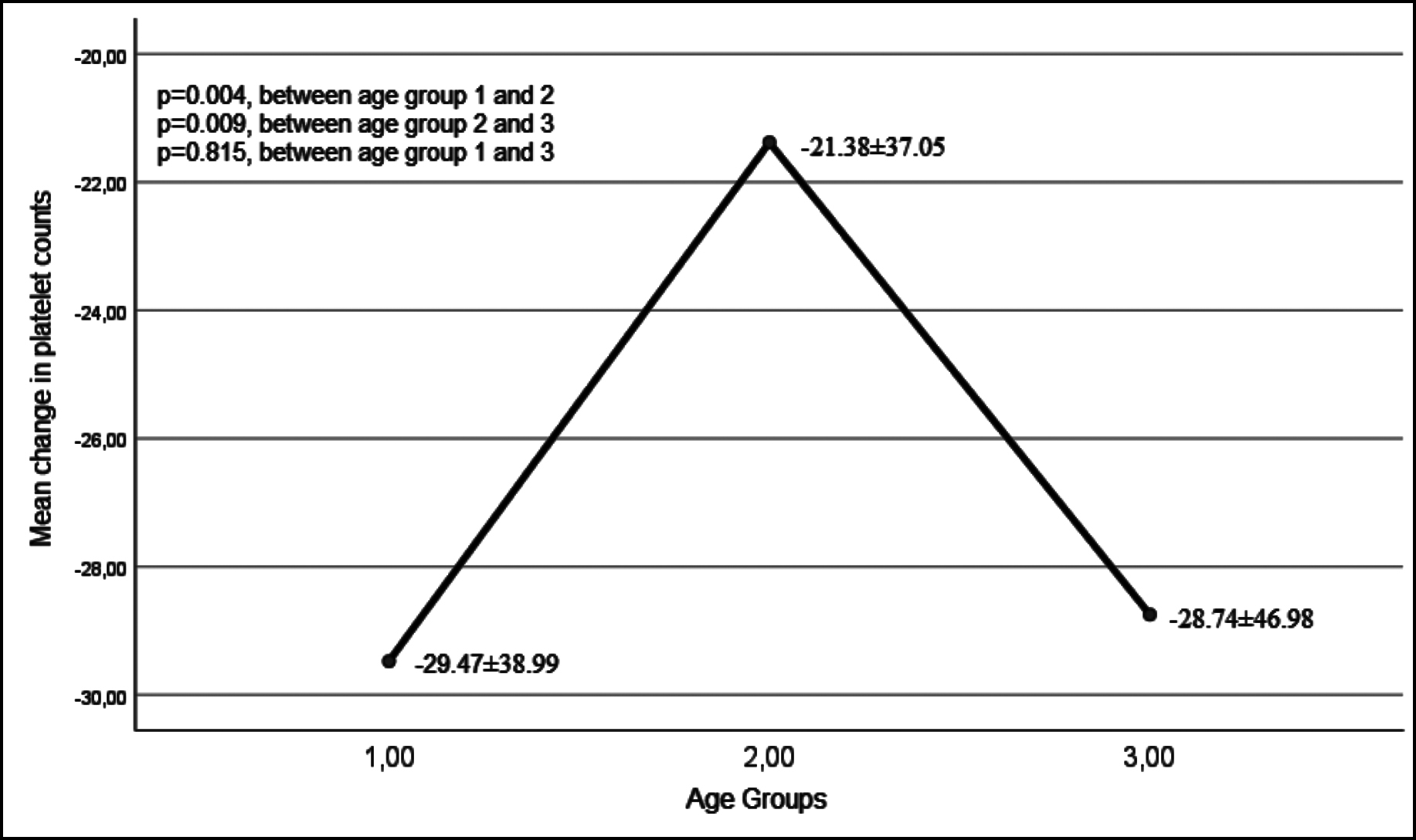 Figure 1: Platelet changes with treatment, according to age groups.
Figure 1: Platelet changes with treatment, according to age groups.
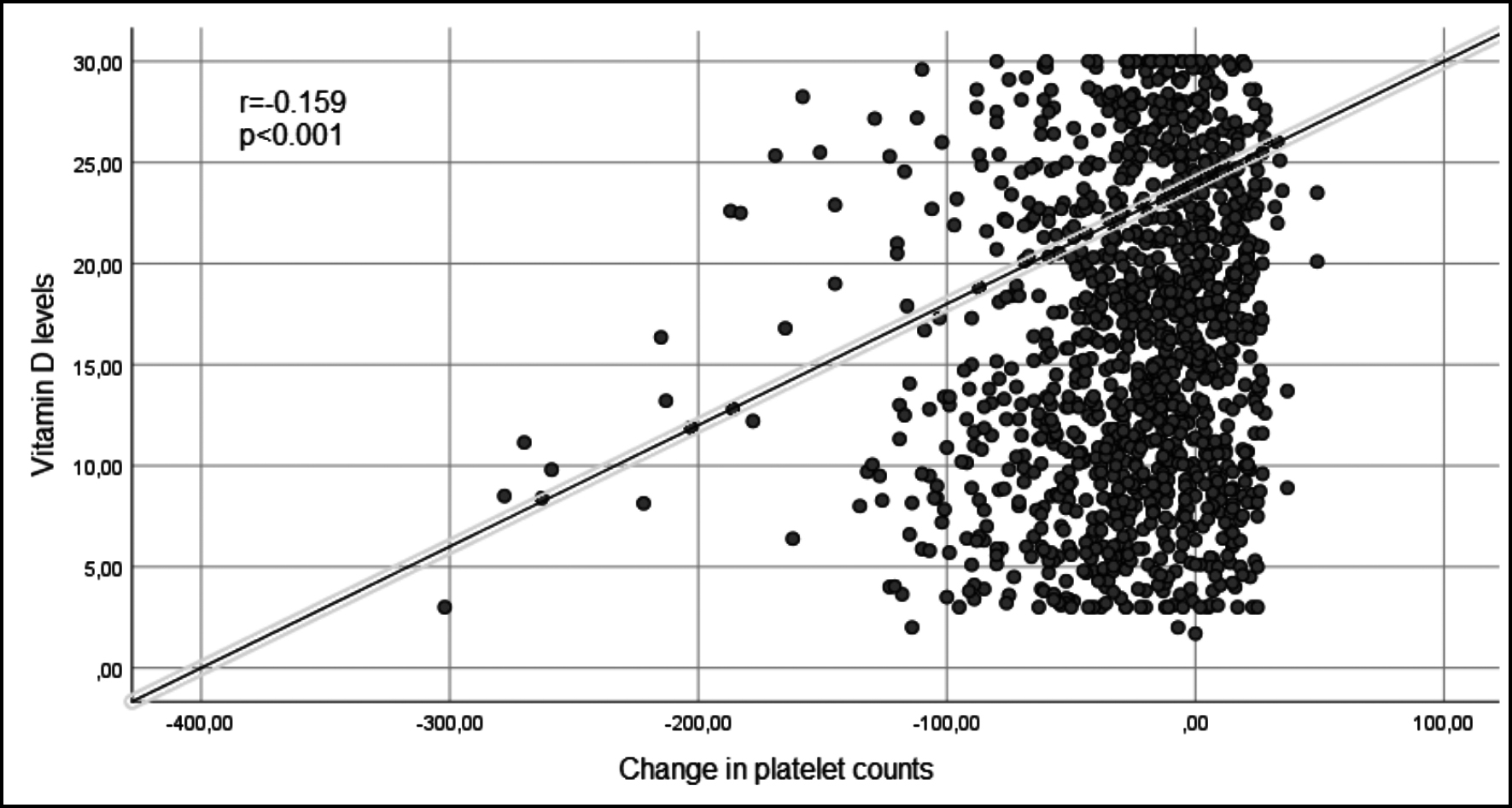 Figure 2: Vitamin D levels and changes in platelet counts.
Figure 2: Vitamin D levels and changes in platelet counts.
In a study including diabetics, an inverse relationship between platelet aggregation and vitamin D levels were documented.13 A study showed that, three months of vitamin D and calcium supplementations decreased levels of anti-inflammatory markers, such as CRP, interleukin 1 (IL-1), interleukin 6 (IL-6) and fibrinogen.14 Inflammation was reported to result in an increase in platelet activation and platelet counts.7 There was an inverse correlation between vitamin D and inflammatory markers in a study.15 Lower vitamin D levels were thought to be related with inflammation and elevated cytokine levels that will cause an increase in platelet counts. Endothelial dysfunction develops in vitamin D insufficiency; and this will result in increased platelet activation and thrombosis.16,17 As a result of aforementioned factors, increase in platelet production and platelet counts are expected. Vitamin D has also reported to have anti-coagulant effects.18 In a study reported by Aihara et al., vitamin D receptor (VDR) knocked-out mice were used and lipopolysaccharide injections in different mice tissues provoked development of thromboses. Thus, VDRs were thought to produce anti-thrombotic effects.19 Active 1,25 dihydroxyvitamin D downregulates vitamin D receptors20 and vitamin D deficiency promotes megakaryocyte maturation and increases thrombocyte counts.3 All these mechanisms are thought to interact with changes in platelet counts. In this reported study, after vitamin D supplementation, decrease in platelet counts in age group above 50 years were found to be greater than 30 to 50 years age group. This may be caused by some reasons; people under 50 years are usually in a hard working lifestyle; and because of this, they may not get benefit of sunlight enough. Thus, endogenous vitamin D synthesis will not be sufficient. People with advanced ages tend to care diets and lifestyles and try to get benefit of sunbaths and open weather day walkings so that their endogenous vitamin D synthesis may be better. These factors may affect functional vitamin D status of people. A study reported the mean vitamin D levels of people above 45 years as greater than people under 45. This was explained by remarkable vitamin D supplementation in people who are above 45 years.21
Because of changes in exposure to sunlight, vitamin D levels of population may vary in different seasons of the year. Mostly in winter, vitamin D levels tend to drop to minimum and in summer tend to increase.22 Because of this variability in vitamin D levels, this reported study was planned to include participants, applying to hospital in a whole year.
Vitamin D levels in females; were reported to be lower than males.23 This reported study also have similar results, vitamin D levels of female participants were lower. Interestingly, majority of participants in this study were females (77.1%). Whether male population apply to hospital rarely compared to females; or females are more willing to participate in the study compared to males, is not clear.
The study design was retrospective, and this may be a limitation for this study. Complete blood count parameters changes during vitamin D replacement treatment was under the scope of this study. Future studies in this subject could evaluate platelet level changes after vitamin D replacement treatment has been ceased.
CONCLUSION
According to results of this study, vitamin D replacement treatment results in lower platelet counts. This finding may be useful in some platelet disorders, such as essential thrombocythemia. Vitamin D treatment may be beneficial in medical conditions in which platelet counts are higher than normal, and may help decrease platelet counts. Vitamin D replacement, especially in patients who have vitamin D deficiency, may decrease platelet counts and risk for thrombotic events. Further studies are required on this subject.
ETHICAL APPROVAL:
This study, approved by local Ethics Committee of the Institute, was conducted in concordance with Declaration of Helsinki and good clinical practice directives.
PATIENTS’ CONSENT:
Informed written consents were obtained from all of the patients who participated in the study.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
MBK, RA: Conception, design, supervision, resources and materials, data collection and or processing, analysis and interpretation, literature search, writing manuscript, and critical review.
REFERENCES
- Holick MF. Vitamin D deficiency. N Engl J Med 2007; 357(3): 266-81. doi: 10.1056/NEJMra070553.
- Lemire JM. Immunomodulatory actions of 1,25-dihydroxyvitamin D3. J Steroid Biochem Mol Biol 1995; 53(1-6): 599-602. doi: 10.1016/0960-0760(95)00106-a.
- Silvagno F, De Vivo E, Attanasio A, Gallo V, Mazzucco G, Pescarmona G. Mitochondrial localisation of vitamin D receptor in human platelets and differentiated megakaryocytes. PLoS One 2010; 5(1):e8670. doi: 10.1371/journal.pone.0008670.
- Ittermann T, Feig MA, Petersmann A, Radke D, Greinacher A, Völzke H, et al. Mean platelet volume is more important than age for defining reference intervals of platelet counts. PLoS One 2019; 14(3):e0213658. doi: 10.1371/journal.pone.0213658.
- Park YC, Kim J, Seo MS, Hong SW, Cho ES, Kim JK. Inverse relationship between vitamin D levels and platelet indices in Korean adults. Hematology 2017; 22(10):623-9. doi: 10.1080/ 10245332.2017.1318334.
- Alanlı R, Küçükay MB, Yalçın KS. Relationship between vitamin D levels and platelet count: A retrospective study. Gulhane Med J 2020; 62:174-8. doi: 10.4274/gulhane.galenos.2020.762.
- Zupo R, Castellana F, Sardone R, Lampignano L, Di Noia C, Savastano S, et al. Hydroxyvitamin D serum levels are negatively associated with platelet number in a cohort of subjects affected by overweight and obesity. Nutrients 2020; 12(2):474. doi: 10.3390/nu12020474.
- Turkish society of endocrinology and metabolism. Guide to metabolic bone diseases. Available from: http://temd.org.tr/ admin/uploads/ tbl_kilavuz/METABOLIK_KH_BOOK_web_.pdf. [cited 2021 Mar 9].
- Medrano M, Carrillo-Cruz E, Montero I, Perez-Simon JA. Vitamin D: Effect on haematopoiesis and immune system and clinical applications. Int J Mol Sci 2018; 19(9):2663. doi: 10.3390/ijms19092663.
- Yikilmaz AŞ, Akinci S, Bakanay ŞM, Dilek İ. Vitamin D deficiency and Janus kinase 2 V617F mutation status in essential thrombocythemia and polycythemia vera. Malays J Med Sci 2020; 27(1):70-7. doi: 10.21315/mjms2020.27.1.7.
- Shaik-Dasthagirisaheb YB, Varvara G, Murmura G, Saggini A, Caraffa A, Antinolfi P, et al. Role of vitamins D, E and C in immunity and inflammation. J Biol Regul Homeost Agents 2013; 27(2):291-5.
- Bonaccio M, Di Castelnuovo A, De Curtis A, Costanzo S, Persichillo M, Donati MB, et al. Moli-sani project investigators. Adherence to the mediterranean diet is associated with lower platelet and leukocyte counts: results from the Moli-sani study. Blood 2014; 123(19):3037-44. doi: 10. 1182/blood-2013-12-541672.
- Sultan M, Twito O, Tohami T, Ramati E, Neumark E, Rashid G. Vitamin D diminishes the high platelet aggregation of type 2 diabetes mellitus patients. Platelets 2019; 30(1): 120-5. doi: 10.1080/09537104.2017.1386298.
- Neyestani TR, Nikooyeh B, Alavi-Majd H, Shariatzadeh N, Kalayi A, Tayebinejad N, et al. Improvement of vitamin D status via daily intake of fortified yogurt drink either with or without extra calcium ameliorates systemic inflammatory biomarkers, including adipokines, in the subjects with type 2 diabetes. J Clin Endocrinol Metab 2012; 97(6):2005-11. doi: 10.1210/jc.2011-3465.
- Erkus E, Aktas G, Atak BM, Kocak MZ, Duman TT, Savli H. Haemogram Parameters in Vitamin D Deficiency. J Coll Physicians Surg Pak 2018; 28(10):779-82.
- Di Rosa M, Malaguarnera G, De Gregorio C, Palumbo M, Nunnari G, Malaguarnera L. Immuno-modulatory effects of vitamin D3 in human monocyte and macrophages. Cell Immunol 2012; 280(1):36-43. doi: 10.1016/j.cellimm.2012.10.009.
- Fuentes QE, Fuentes QF, Andrés V, Pello OM, Font de Mora J, Palomo GI. Role of platelets as mediators that link inflammation and thrombosis in atherosclerosis. Platelets 2013; 24(4):255-62. doi: 10.3109/09537104.2012.690113.
- Koyama T, Hirosawa S. Anticoagulant effects of synthetic retinoids and activated vitamin D3. Semin Thromb Hemost 1998; 24(3):217-26. doi: 10.1055/s-2007-995845.
- Aihara K, Azuma H, Matsumoto T. Vitamin D-vitamin D receptor system regulates antithrombogenicity in vivo. Clin Calcium 2006; 16(7):1173-79. Japanese.
- Song LN. Demonstration of vitamin D receptor expression in a human megakaryoblastic leukemia cell line: regulation of vitamin D receptor mRNA expression and responsiveness by forskolin. J Steroid Biochem Mol Biol 1996; 57(5-6):265-74. doi: 10.1016/0960-0760(95)00266-9.
- Cigerli O, Parildar H, Unal AD, Tarcin O, Erdal R, Guvener Demirag N. Vitamin D deficiency is a problem for adult out-patients? A university hospital sample in Istanbul, Turkey. Public Health Nutr 2013; 16(7):1306-13. doi: 10.1017/ S1368980012003588.
- Kayacan AG, Sürmeli N, Ünlü Söğüt M, Yılmaz E. Evaluation of obesity with Vitamin D Levels and related parameters. Erciyes Med J 2019; 41(2):180-5 doi: 10.14744/etd.2019. 92609.
- Lips P. Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem Mol Biol 2007; 103(3-5):620-5. doi: 10. 1016/j.jsbmb.2006.12.076.