Various Risk Factors of Overweight and Obesity among Children Aged 5-16 Years
By Ajea Rani Bekhwani, Mashal KhanAffiliations
doi: 10.29271/jcpsp.2022.06.763ABSTRACT
Objective: To determine the determinants of overweight and obesity among children aged 5-16 years.
Study Design: Descriptive study.
Place and Duration of Study: Emergency and Outpatient Department of National Institute of Child Health, from October 2020 till July 2021.
Methodology: All children of either gender ranged between 5 and 16 years were enrolled. Children with ≥85 and <95 percentile were labeled as overweight and ≥95 percentile as obese. Other determinants like physical factors, high screen time, and environmental factors were noted. Frequency and percentages were computed for gender, residence, overweight, obesity, and physical and environmental factors. Mann-Whitney U-test was applied to determine the median difference of quantitative variables between overweight/obese and healthy children. The comparison was done to see the association of the presence of overweight/obesity with respect to the baseline characteristics. Binary logistic regression analysis was also applied.
Results: Of 184 children, 99 (53.8%) were males and 85 (46.2%) females. The median age was 9 (7-12) years. There were 25 (13.6%) overweight and 80 (43.5%) obese children. In combination, the frequency of overweight/obesity was found to be 105 (57.1%). After adjusting for other covariates, the odds of overweight and obesity were significantly higher for children with age ≤9 years (adjusted OR: 3.40, 95% CI: 1.51-7.66) and male gender (adjusted OR: 3.95, 95% CI: 1.80-8.68). However, lower odds of overweight/obesity were observed among children with low physical activity at school (adjusted OR: 0.31, 95% CI: 0.14-0.66) and low screen time (≤4 hours) (adjusted OR: 0.24, 95% CI: 0.11-0.55).
Conclusion: Children aged 5 to 16 years had a much greater frequency of overweight and obesity. Factors such as younger age, male gender, lower physical activity, and high time screen have been demonstrated to contribute significantly.
Key Words: Children, Obese, Overweight, Risk factors, Pakistan.
INTRODUCTION
Childhood overweight and obesity is a rapidly growing public health problem.1 Similar issues are reported from Pakistan as well where abnormally increased weight in children is reported among children belonging to privileged even middle or upper middle-class socioeconomic status.2It is a well-known fact that overweight and obesity in children have various negative consequences that are not only limited to the physical health of the children but also largely affect their social, psychological, and personality development. In addition to this, childhood obesity and overweight significantly raise the risk of a variety of noncommunicable diseases.3
It is also reported in the literature that in infancy and adolescence, overweight and obesity have been associated with a higher risk of early death and morbidity in adulthood.4
Thus, to prevent childhood obesity, it is critical to identify associated risk factors. Numerous investigations worldwide have shown that obesity risk factors are of multiple aspects, such as dietary practices of children, activity level, screening time, family history of obesity, and parenting literacy.5,6
The rationale of this study was that low physical activity and sedentary lifestyles are remarkably increasing all over the world. Particularly, children are more vulnerable and need special attention to avoid health-related issues in the future. Furthermore, after the occurrence of the CoronaVirus Disease (COVID)-19 outbreak, the risk of being overweight and obese is doubled in children. Therefore, there is a dire need to understand the burden of the disease and associated risk factors in young children. Therefore, this study was conducted to investigate the determinants of overweight and obesity among children aged 5-16 years in a tertiary care hospital in metropolitan city Karachi.
METHODOLOGY
This descriptive study was carried out at the emergency and the outpatient department of the National Institute of Child Health, Karachi from October 2020 to July 2021. The Institutional Ethical Review Committee granted ethical approval. Furthermore, prior to enrollment in the study, permission from the guardian/parents was obtained.
All children of either gender aged 5-16 years, were consecutively enrolled. However, those children who were on steroids for any reason, as well as any other medicines that can cause obesity, and/or comorbidity that could lead to obesity, were excluded from the study.
The Epi Info sample size calculator was used to estimate sample size, with confidence intervals of 97 percent, margins of error of 5 percent, and reported overweight in children of 10.5 percent. The estimated sample size was 177 children. The current study, however, enrolled 184 children.
Health status was defined on the basis of body mass index for age percentile based on z-score. Children with 5th percentile to less than 85th percentile were labelled as a normal or healthy weight. Whereas children with ≥85 and <95 percentile were labeled as overweight and ≥95 percentile as obese.
This information along with certain important determinants like physical factors, high screen time, and environmental factors was noted. Physical factors were measured on the basis of CDC guidelines.7 Sixty minutes or less energetic physical activity for at least 3 days per week was labelled as low physical activity whereas 60 minutes or more energetic physical activity for the minimum period of 3 days per week was labelled as high physical activity. Vigorous physical activity was defined as playing or exercise that makes children sweat and breathe hard.7 High screen time was assessed based on the number of hours of watching television / iPad / mobile phone / laptop / desktop. Watching ≥4 hours per day was labeled as high screen time.8 Environmental factors were assessed on the basis of following social and family characteristics; residence (rural/urban), total monthly household income, physical activity at school, availability of ground at or near home, mother feeding history, mother’s education status, and family structure.
Data analysis was performed via Statistical Package for Social Sciences (SPSS) version 24. Median along with the interquartile range (IQR) were computed for quantitative variables such as age, Body Mass Index (BMI), screen time duration, duration of outdoor games, and total monthly household income. Frequency and percentages were computed for gender, residence, overweight, obesity, and physical and environmental factors. Mann-Whitney U-test was applied to determine the median difference of quantitative variables between overweight/obese and healthy children. The comparison was done to see the association of the presence of overweight/obesity with respect to the baseline characteristics. Chi-square/Fisher-Exact test was applied, and p-value less than equal to 0.05 was labelled as statistically significant. Binary logistic regression analysis was also applied. All those variables found statistically significant at contingency table were selected in the binary logistic regression analysis. Both univariable and multivariable regression analysis was performed.
RESULTS
Of the 184 children, the median age was 9 (7-12) years. Gender distribution revealed 99 (53.8%) males and 85 (46.2%) females. The median weight, height, and BMI were found to be 32 (25-40) kg, 122 (107-130) cm, and 21 (17-27) kg/m2 respectively. Most of the children had a mother/breastfeed, i.e., 127 (69%). Educational status showed that 87 (47.3%) had matric or greater maternal education. Living characteristics showed that 138 (75%) of the children had urban residences whereas 78 (42.4%) had a combined family structure. Physical activity at school was reported by 93 (50.5%) of the children, availability of ground at or near home 57 (31%), vigorous physical activity 45 (24.5%), whereas high screening time by 86 (46.7%) children.
Health status as per age percentile based on z-score showed that 79 (42.9%) children were healthy, 25 (13.6%) were overweight, and 80 (43.5%) were obese. In combination, the frequency of overweight/obesity was found to be 105 (57.1%), (Figure 1).
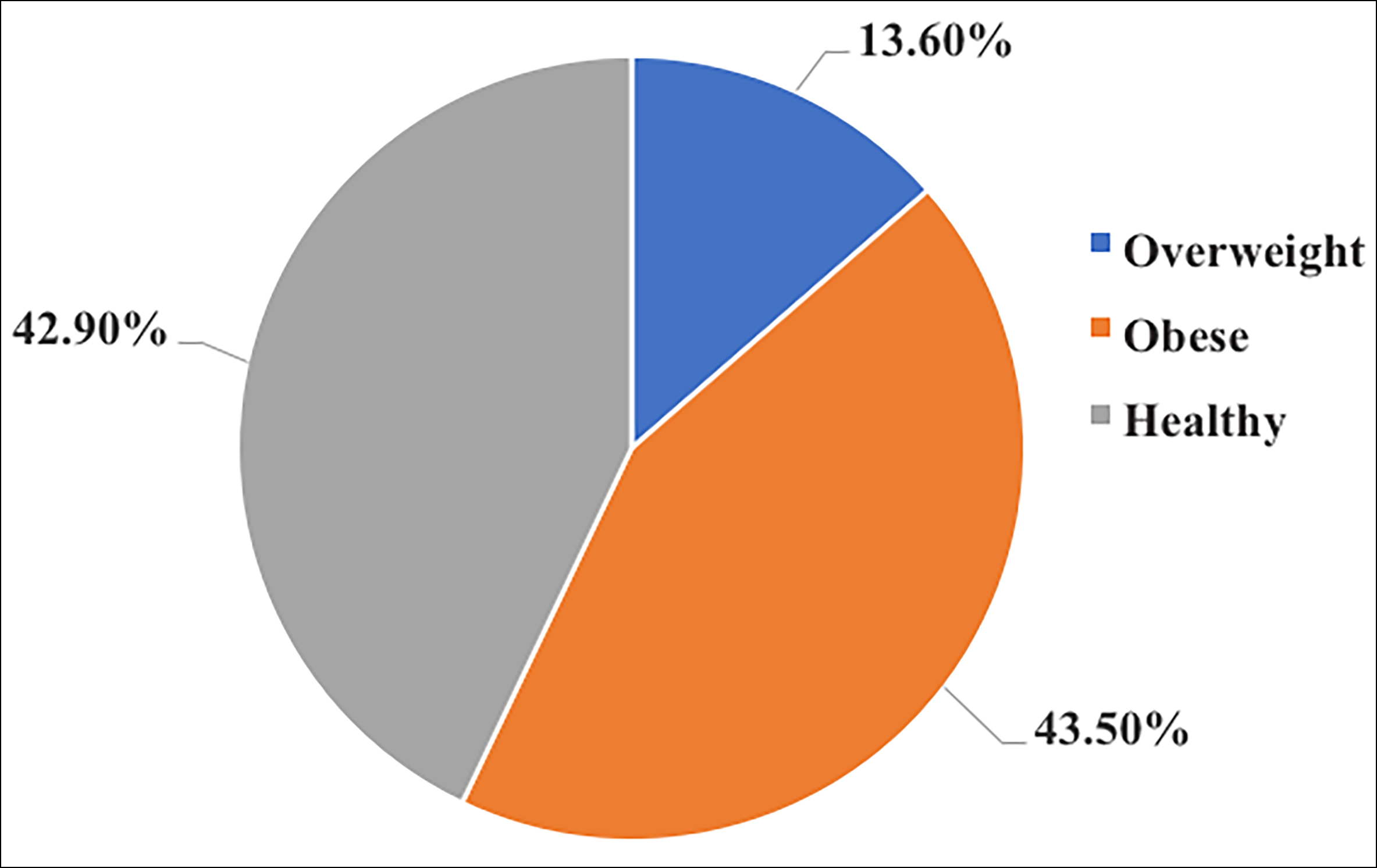 Figure 1: Health status of the children as per age percentile based on z-score (n=184).
Figure 1: Health status of the children as per age percentile based on z-score (n=184).
Overweight/obese patients had significant median difference with respect to age (p<0.001), weight (p<0.001), height (p=0.006), BMI (p<0.001), duration of screen time (p<0.001), and duration of outdoor games (p=0.012), (Table I). Similarly, overweight/obese were significantly associated with residence (p=0.032), family structure (p= 0.011), physical activity at school (p<0.001), availability of ground at or near home (p= 0.036), vigorous physical activity (p=0.008), and high screen time (p<0.001), (Table II).
The findings of the univariate analysis revealed that the odds of overweight/obesity were significantly higher for children with age ≤9 years (OR: 1.89, 95% CI: 1.03-3.45, p= 0.038), male gender (OR: 1.96, 95% CI: 1.08-3.55, p= 0.026), combined family structure (OR: 2.20, 95% CI: 1.19-4.05, p= 0.011), urban residence (OR: 2.08, 95% CI: 1.06-4.10, p= 0.033), and ≤60 minutes per week vigorous physical activity (OR: 2.51, 95% CI: 1.26-4.99, p= 0.009).
Table I: Median difference of baseline characteristics with respect to overweight/obesity status (n=184).
|
Variables |
Overweight/Obese |
p-value |
||
|
Total Median (IQR) |
Yes (n=105) Median (IQR) |
No (n=79) Median (IQR) |
||
|
Age, years |
9 (7-12) |
9 (6-12) |
10 (7-13) |
<0.001 |
|
Weight (kg) |
32 (25-40) |
36 (29-42) |
27 (21-33) |
<0.001 |
|
Height (cm) |
122 (107-130) |
121 (104-129) |
125 (112-136) |
0.006 |
|
BMI (kg/m2) |
21 (17-27) |
26 (21-28) |
17 (15-18) |
<0.001 |
|
Duration of screen times (hours) |
3.5 (1.6-5.5) |
5 (3-6) |
2 (1-4) |
<0.001 |
|
Duration of outdoor games (minutes) |
30 (20-60) |
30 (15-60) |
45 (30-60) |
0.012 |
|
Total monthly household income (Rs) |
18,000 (15,000-22,250) |
16,000 (15,000-22,000) |
19,000 (13,000-24,000) |
0.572 |
|
Mann-Whitney U-test applied, p-value <0.05 considered significant. |
||||
Table II: Comparison of overweight/obesity status with respect to baseline characteristics (n=184).
|
Total (n=184) |
Overweight / Obese |
p-value |
||
|
Yes (n=105) |
No (n=79) |
|||
|
Age (years) |
||||
|
≤9 |
79 (42.9) |
52 (65.8) |
27 (34.2) |
0.037 |
|
>9 |
105 (57.1) |
53 (50.5) |
52 (49.5) |
|
|
Gender |
||||
|
Male |
99 (53.8) |
64 (64.6) |
35 (35.4) |
0.025 |
|
Female |
85 (46.2) |
41 (48.2) |
44 (51.8) |
|
|
Feed |
||||
|
Mother / Breast feed |
127 (69.0) |
77 (60.6) |
50 (39.4) |
0.145 |
|
Top feed |
57 (30.9) |
28 (49.1) |
29 (50.9) |
|
|
Mothers' educational status |
||||
|
Illiterate |
61 (33.1) |
40 (65.6) |
21 (34.4) |
0.241 |
|
Secondary or less |
36 (19.6) |
20 (55.6) |
16 (44.4) |
|
|
Matriculation or more |
87 (47.3) |
45 (51.7) |
42 (48.3) |
|
|
Residence |
||||
|
Urban |
138 (75.0) |
85 (61.6) |
53 (38.4) |
0.032 |
|
Rural |
46 (25.0) |
20 (43.5) |
26 (56.5) |
|
|
Family structure |
||||
|
Combined |
78 (42.4) |
53 (67.9) |
25 (32.1) |
0.011 |
|
Nuclear |
106 (57.6) |
52 (49.1) |
54 (50.9) |
|
|
Physical activity at school |
||||
|
Yes |
93 (50.5) |
34 (36.6) |
59 (63.4) |
<0.001 |
|
No |
91 (49.5) |
71 (78.0) |
20 (22.0) |
|
|
Availability of ground at or near home |
||||
|
Yes |
57 (30.9) |
26 (45.6) |
31 (54.4) |
0.036 |
|
No |
127 (69.0) |
79 (62.2) |
48 (37.8) |
|
|
Vigorous physical activity |
||||
|
≤60 minutes per week |
139 (75.5) |
87 (62.6) |
52 (37.4) |
0.008 |
|
>60 minutes per week |
45 (24.5) |
18 (40.0) |
27 (60.0) |
|
|
Screen time, hours |
||||
|
≤4 |
98 (53.2) |
40 (40.8) |
58 (59.2) |
<0.001 |
|
>4 |
86 (46.7) |
65 (75.6) |
21 (24.4) |
|
|
All data presented as number (%). |
||||
However, lower odds of overweight/obesity were observed among children with physical activity at school (OR: 0.16, 95% CI: 0.08-0.31, p<0.001) and screen time of ≤4 hours (OR: 0.22, 95% CI: 0.12-0.42, p<0.001). The findings of the multivariable analysis revealed that after adjusting for other covariates, the odds of overweight/obesity were significantly higher for children with age ≤9 years (aOR: 3.40, 95% CI: 1.51-7.66, p=0.003) and male gender (aOR: 3.95, 95% CI: 1.80-8.68, p<0.001). However, lower odds of overweight/obesity were observed among children with low physical activity at school (aOR: 0.31, 95% CI: 0.14-0.66, p =0.002) and low screen time (≤4 hours) (OR: 0.24, 95% CI: 0.11-0.55, p<0.001).
DISCUSSION
Childhood overweight and obesity have increased dramatically over the past few decades.9 The current study found that 13.6% of children were overweight, and 43.5% were obese. The combined prevalence of overweight/obesity was found to be 57.1%. Findings from different studies have shown large differences. For instance, obesity among children and adolescents residing in Brazil was found to be approximately 22%. Moreover, 42% in Mexico, 19% in Argentina, and 22% in India, which is a developing country like Pakistan.10 According to a recent Pakistani study, of total 1872 children, 10% of the children were overweight and 5% were obese.11 In another study, 65% children were of a healthy weight, 10% underweight, and 25% overweight or obese.12 In one study, it was found that watching TV for less than three hours had a 4.47 times increased risk of developing obesity, breastfeeding for six months had a 4.16 times increased risk, and maternal BMI >24.9 kg/m2 had a 2.70 times increased risk of developing obesity.13
As per the current study findings, the odds of overweight/obesity were significantly higher for children with ages less than equal to nine years. According to a recent study by Bont et al. the prevalence of overweight and obesity was highest among children aged six and seven years.14 Several studies have reported the highest incidence rates during mid-childhood, which shows a decline in older children, except for a study15, which reported similar incidence levels between the ages of two and six years.15-17
According to the results of the present study, males are more likely than females to be overweight or obese. Likewise, Bont et al. found that males were more likely to be overweight or obese.14 However, a previous study reported children with overweight had 4 times more risk of having obesity among both sexes.15
The findings of the current study also reported that low physical activity at school was also a significant factor associated with higher odds of overweight and obesity. In addition to this, physical activity increases children's energy expenditure and reduces their chances of being overweight or obese, however with steadily increasing screen time in school-aged children, there is a considerable drop in sporting events.18,19 It is well evident that low physical activity leads to sedentary behavior, which is linked to obesity.20
The findings of this study could be highlighted in light of the following limitations. First, this was a cross-sectional study and was conducted in a single centre on a limited sample size. Second, certain important predictor variables like type of food intake, junk food frequency, cola drinks, and chocolate intake were not observed in the current study. Further large-scale multicenter studies are recommended that not only investigate the burden of overweight and obesity and its associated risk factors but also some interventions to promote an increase in physical activity and healthy lifestyle behaviour among children.
CONCLUSION
A considerably higher frequency of overweight and obesity was found in our cohort of children aged 5-16 years. In particular, factors like younger age, male gender, less physical activity, and high screen time were found as significant contributing factors.
ETHICAL APPROVAL:
Ethical approvals were obtained from the Institutional Ethical Review Committee of the National Institute of Child Health prior to the initiation of the research work.
PATIENTS’ CONSENT:
Informed consent was obtained from parents/guardians to publish the data.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
MK: Conception and designing of the study, manuscript writing.
AR: Critically reviewed for important intellectual content.
Both authors agreed on the final version of the manuscript for publication.
REFERENCES
- Gill T. Epidemiology and causes of obesity in children and young adults. Eating disorders and obesity: A comprehensive handbook. 2017:393.
- Tanzil S, Jamali T. Obesity, an emerging epidemic in Pakistan-a review of evidence. J Ayub Med Coll Abbottabad 2016; 28(3):597.
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumer R, Bhadotia AS. Childhood obesity: Causes and consequences. J Family Med Primary Care 2015; 4(2):187-92. doi: 10.4103/2249-4863.154628.
- Sommer A, Twig G. The impact of childhood and adolescent obesity on cardiovascular risk in adulthood: A systematic review. Current Diab Reports 2018; 18(10):91. doi: 10.1007/s11892-018-1062-9.
- Kumar S, Kelly AS. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc 2017; 92(2):251-65. doi: 10.1016/j.mayocp.2016.09.017.
- Albataineh SR, Badran EF, Tayyem RF. Overweight and obesity in childhood: Dietary, biochemical, inflammatory and lifestyle risk factors. Obesity Med 2019; 100112. doi: 10.1016/j.obmed.2019.100112
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for Americans. JAMA 2018; 320(19):2020-8. doi: 10.1001/jama.2018.14854.
- Engberg E, Figueiredo RA, Rounge TB, Weiderpass E, Viljakainen H. Heavy screen use on weekends in childhood predicts increased body mass index in adolescence: A three-year follow-up study. J Adolescent Health 2020; 66(5):559-66. doi: 10.1016/j.jadohealth.2019.09.002.
- de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clinical Nutr 2010; 92(5):1257-64. doi: 10.3945/ajcn.2010.29786.
- Gupta N, Shah P, Nayyar S and Misra A. Childhood obesity and metabolic syndrome in developing countries. Indian J Pediatr 2013; 80(1):28-37. doi: 10.1007/s12098-012- 0923-5.
- Khan S, Abbas A, Ali I, Arshad R, Tareen MB, Shah MI. Prevalence of overweight and obesity and lifestyle assessment among school–going children of Multan, Pakistan. Isra Med J 2019; 11(4):230-3.
- Mathew SM, Bell LK, Mauch C, Magarey AM. Weight status and diets of children aged 1–12 years attending a tertiary public paediatric outpatient clinic. J Paediatr Child Health 2020; 56(1):47-54. doi: 10.1111/jpc.14489.
- Hossain M, Zannat IA, Begum S, Rahman S. Risk factors for overweight and obesity among children and adolescents in Bangladesh: A hospital based study. Bangladesh J Child Health 2019; 43(1):9-14. doi: 10.3329/bjch.v43i1.41210.
- de Bont J, Díaz Y, Casas M, García-Gil M, Vrijheid M, Duarte-Salles T. Time trends and sociodemographic factors associated with overweight and obesity in children and adolescents in Spain. JAMA Network Open 2020; 3(3):e201171. doi: 10.1001/jamanetworkopen.2020.1171.
- Von Kries R, Beyerlein A, Müller MJ, Heinrich J, Landsberg B, Bolte G, et al. Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int J Obesity 2012; 36(4):505-10. doi: 10.1038/ijo.2011.251. doi: 10.1038/ijo.2011.251.
- Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med 2014; 370:403-11. doi: 10.1056/NEJMc1402397.
- Hughes AR, Sherriff A, Lawlor DA, Ness AR, Reilly JJ. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Preventive Med 2011; 52(5):300-4. doi: 10.1016/j.ypmed.2011.02.014.
- Whiting S, Buoncristiano M, Gelius P, Abu-Omar K, Pattison M, Hyska J, et al. Physical activity, screen time, and sleep duration of children aged 6-9 years in 25 countries: An analysis within the WHO European childhood obesity surveillance initiative (COSI) 2015-2017. Obesity Facts 2021; 14(1):32-44. doi: 10.1159/000511263.
- Friel CP, Duran AT, Shechter A, Diaz KM. US children meeting physical activity, screen time, and sleep guidelines. Am J Preventive Med 2020; 59(4):513-21. doi: 10.1016/j. amepre.2020.05.007.
- Yuksel HS, Şahin FN, Maksimovic N, Drid P, Bianco A. School-based intervention programs for preventing obesity and promoting physical activity and fitness: A systematic review. Int J Envir Res Public Health 2020; 17(1):347. doi: 10.3390/ijerph17010347.