Two-point Fixation for Biological Mesh in Laparoscopic Inguinal Hernia Repair
By Guozhong Liu, Yiping Chen, Yuhai Hu, Jianbin Zhang, Shangeng WengAffiliations
doi: 10.29271/jcpsp.2022.12.1534ABSTRACT
Objective: To evaluate the clinical outcomes and safety of two-point fixation for biological mesh in laparoscopic totally extraperitoneal (TEP) inguinal hernia repair.
Study Design: Case series.
Place and Duration of Study: The first Affiliated Hospital of Fujian Medical University Hospital, Fuzhou, China, from January to December 2019.
Methodology: A total of 38 patients with a primary inguinal hernia who underwent laparoscopic TEP repair with a small intestine submucosal matrix biological mesh were included. A novel two-point fixation method was performed at the level of 2 cm above the upper margin of the hernia ring. The mesh was fixed at 3 cm medial and lateral to the inferior epigastric artery. The recurrence rate, surgical site infection rate, postoperative chronic pain, hematoma/seroma, and chronic pain were evaluated.
Results: There was no conversion to open procedure. The surgical time was 60.0 (range 35–72) min, and the time of mesh fixation was 4.00 (range 2.5–6.0) minutes. All patients were discharged on the first postoperative day and had similar pain scores (VAS score = 1). Hematoma/seroma was detected in only three (7.9%) patients. No infection or recurrence was observed.
Conclusion: The two-point fixation for biological mesh is reliable and easy to perform. Further study with a larger sample size may be needed to validate it.
Key Words: Inguinal hernia, Laparoscopy, Biological mesh, Surgical mesh, Herniorrhaphy, Two-point fixation.
INTRODUCTION
Inguinal hernia, is a common hernial defect, especially in older people.1 It is not usually considered dangerous, but physical activity and heavy lifting might provoke pain or even lead to life-threatening complications such as intestinal strangulation.1,2 Surgical repair via open or laparoscopic techniques is the most common approach. The laparoscopic repair offers many advantages over the open approach for a lower recurrence risk, less pain, and faster recovery.3 The laparoscopic repair with a mesh by trans-abdominal preperitoneal (TAPP) or totally extraperitoneal (TEP) approaches have started to be increasingly used as the most common treatment methods.4 Although these two techniques are similar in efficacy and complications, TEP may be more technically difficult than TAPP, however, the former has the advantage that it does not require an additional intervention for peritoneal closure.5
The clinical effectiveness of hernia repair is usually evaluated with regard to recurrence, groin pain, hospitalisation time, recovery time, and complications.6 The mesh fixation techniques and the mesh material can considerably affect the indicators above.7 The current options for mesh fixation in TEP include the use of sutures, tacks or staples, and tissue glues.8 The tensile strength of transabdominal sutures was reported to be greater than the tensile strength of tackers.9 Using a developed standardised two-point mesh anchoring was established to be safe and feasible for laparoscopic Sugarbaker parastomal hernia repair.10
Synthetic non-absorbable mesh has been widely accepted as the standard in routine hernia surgery. However, several studies found negative effects of permanent implants, and the application of biological or synthetic degradable meshes has been proposed.11 Porcine-derived small intestinal submucosa (SIS) mesh has been implanted in several animal species and humans, with no evidence reported of an adverse host immune response. An earlier investigation revealed that SIS elicited an immunologic recognition but did not prevent xenograft acceptance12 and was rapidly degraded after its in vivo implementation as a bioscaffold. Meanwhile, other reports showed that biological meshes usually softened when introduced into the groin area, shrank from the hernia position, or promoted recurrence.13
This study aimed to evaluate the clinical outcomes and safety of the novel two-point fixation method for small intestine submucosal matrix biological mesh in the laparoscopic TEP repair inguinal hernia. It was hypothesised that using a biologically degradable mesh will lower the rates of complications, such as site infection and postoperative chronic pain. Furthermore, the chosen fixation method would facilitate the prevention of shrinking and hernia recurrence.
METHODOLOGY
This retrospective case series included patients with primary inguinal hernia treated at Fujian Medical University Hospital Fuzhou, China, between January and December 2019. All patients were performed TEP mesh repair by VIDASIS® SIS. The research was approved by the Ethics Committee of the Hospital (approval number: MRCTA, ECFAH of FMU [2019]187). All participants provided written informed consent.
The inclusion criteria were age 18-50 years, reducible inguinal hernia, and American Society of Anesthesiologists (ASA) physical status I-III. The exclusion criteria were incarcerated hernia, other concurrent surgeries, or a history of surgery in the inguinal area of the affected side.
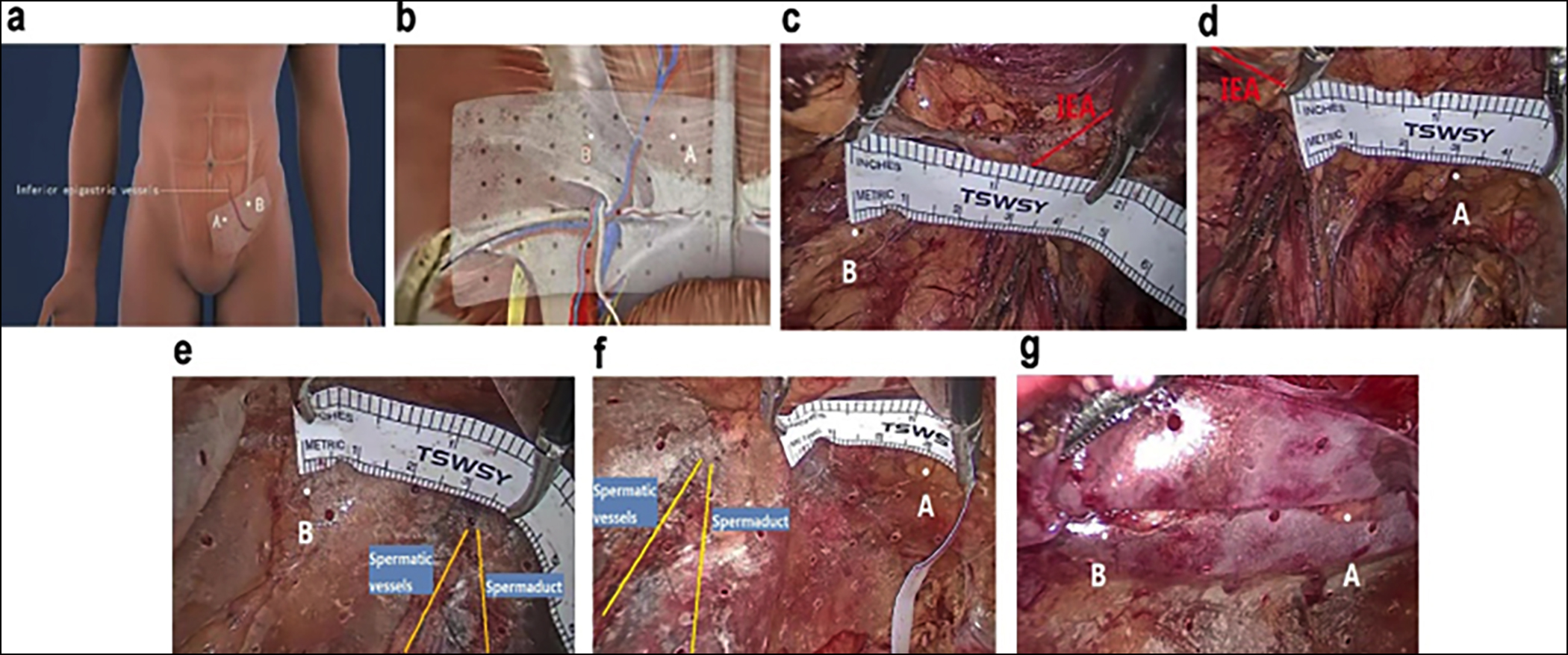 Figure 1: Projection and intraoperative photos of the two-points (A and B sites) fixation. Procedure adopted for SIS mesh fixation. (A) Projections of the fixation sites on the body surface; b, extraperitoneal projections of the fixation sites; (C,D) Intraoperative photo of a patient with left inguinal hernia. Before placing the biological mesh, the A site was 2-3 cm medial to the inferior epigastric artery (IEA) at the level above the iliopubic tract, and the B site was 2-3 cm lateral to the IEA at the level above the iliopubic tract; (E,F) The two points were confirmed again after placing the mesh, and then the fixation was performed; and (G) Post-fixation picture of the mesh.
Figure 1: Projection and intraoperative photos of the two-points (A and B sites) fixation. Procedure adopted for SIS mesh fixation. (A) Projections of the fixation sites on the body surface; b, extraperitoneal projections of the fixation sites; (C,D) Intraoperative photo of a patient with left inguinal hernia. Before placing the biological mesh, the A site was 2-3 cm medial to the inferior epigastric artery (IEA) at the level above the iliopubic tract, and the B site was 2-3 cm lateral to the IEA at the level above the iliopubic tract; (E,F) The two points were confirmed again after placing the mesh, and then the fixation was performed; and (G) Post-fixation picture of the mesh.
All surgeries were performed by the same group of surgeons. The two-point fixation technique is briefly described below: A 10 × 15 cm biological mesh was immersed in normal saline, placed into the abdominal cavity, and flattened, then it was fixed at the A and B sites at 2–3 cm from bilateral sides of the inferior epigastric artery at a level above the iliopubic tract. The projections of the A and B sites are depicted in Figure 1A,B. The A and B sites were measured before placing the mesh. The A site was at 3 cm medial to the inferior epigastric artery and at least 2 cm above the upper margin of the hernia ring. The B site was at 3 cm lateral to the inferior epigastric artery and at least 2 cm above the upper margin of the hernia ring (Figure 1C,D)., Figure 1E,F presents the projections of the fixation sites on the body surface after the mesh was placed. The puncture outfit (olecranoid anastomat for the abdominal wall) equipped with 4-0 Ethicon absorption thread was used to puncture the skin, the subcutaneous, muscular, and transversalis fascia layers, and then to puncture the corresponding fixation sites of the biological mesh. The thread was delivered, and the needle was withdrawn to the subcutaneous layer. Next, the needle was inserted at a different site again through the biological mesh, and the thread was pulled outward to the subcutaneous layer, which was then knotted with the other end of the thread to fix the mesh (Figure 1G).
The patients were followed up postoperatively for 1, 3, and 12 months by the outpatient department or by telephone calls. Information on the recurrence rate, surgical site infection rate, postoperative chronic pain, hematoma/seroma, the sense of the mesh as a foreign object, and chronic pain were collected. A visual analogve scale (VAS) was used to evaluate the patients’ postoperative pain.
R Foundation for Statistical Computing (4.0.2, Vienna, Austria) was employed for the statistical analysis. The Shapiro-Wilk test was used to verify the normality of the data. Quantitative data were expressed as medians (interquartile range, IQR). Qualitative data were presented as frequencies and percentages. A p-value <0.05 was considered to indicate statistically significant differences.
Table I: Baseline characteristics of the patients.
|
Variable |
Value (N = 38) |
|
Age (years) |
23.5 (18.0–31.8) |
|
Gender |
|
|
Male |
31 (81.6%) |
|
Female |
7 (18.4%) |
|
BMI (kg/m2) |
21.97 (20.31–23.72) |
|
Type of hernia |
|
|
Femoral hernia |
4 (10.5%) |
|
Indirect hernia |
35 (92.1%) |
|
Direct hernia |
1 (2.6%) |
|
Unilateral/bilateral hernia |
|
|
Unilateral hernia |
36 (94.7%) |
|
Bilateral hernia |
2 (5.3%) |
|
Inguinal Hernia Classification |
|
|
I |
5 (13.2%) |
|
II |
32 (84.2%) |
|
III |
3 (7.9%) |
|
IV |
0 (0.0%) |
|
Data are presented as medians (IQR) or frequencies (percentages). |
|
Table II: Perioperative data and postoperative complications of the patients with a primary inguinal hernia who underwent hernia repair with a SIS mesh.
|
Variable |
Value (n = 38) |
|
Surgical time (min) |
60.0 (48.0–62.2) |
|
Suture time (min) |
4.00 (3.00–4.00) |
|
Estimated blood loss (mL) |
10.0 (5.00–10.0) |
|
Defect area (cm2) |
3.00 (2.25–4.00) |
|
Length of hospital stay (day) |
1 (1.00–1.00) |
|
Postoperative activity time (hour) |
6.00 (5.00–7.00) |
|
Pain score |
1.00 (1.00–1.00) |
|
Intraoperative complications |
0 (0%) |
|
Wound-related complications |
3 (7.9%) |
|
Hematoma/seroma |
3 (7.9%) |
|
Non-wound-related complications |
5 (13.2%) |
|
Fever |
5 (13.2%) |
|
Data are presented as medians (IQR) or frequencies (percentages). |
|
RESULTS
A total of 38 patients were included, of whom 31 (81.6%) were males, and 7 (18.4%) were females. Baseline characteristics of the patients are listed in Table I. The mean age was 23.5 (range 18–31.8) years. Thirty-six patients (94.7%) had a unilateral hernia, and the remaining 2 patients (5.3%) had a bilateral hernia. Indirect hernia was the most common defect, reported in 35 (92.1%) of the patients, whereas direct and femoral hernias were reported in 1 (2.63%) and 4 (10.5%) of the patients, respectively. Based on the classification criteria of inguinal hernia among 38 patients with 40 primary hernias, 5 (13.2%), 32 (84.2%), 3 (7.9%), and 0 of the hernia patients were type I, II, III, and IV respectively. No patient had a history of hypertension or diabetes mellitus.
Surgery was successfully performed in all 38 patients, with no conversion to open procedure. As can be seen in Table II, the mean surgical time was 60.0 (48.0–62.2) min, the suture time was 4.0 (3.0–4.0) min, and the estimated blood loss was 10.0 (5.0–10.0) mL. Postoperatively, the average activity time of the patients was 6.0 (5.0–7.0) h. All patients were discharged on the first postoperative day and had an equal pain score (VAS score = 1).
All 38 patients received postoperative follow-up. Five (13.2%) patients reported mild fever within one week postoperatively, which was relieved without any specific treatment. Hematoma/seroma was found in three (7.9%) patients at the one-month follow-up of physical examination. Those changes were confirmed by ultrasonography and were absorbed spontaneously at three months. None of the patients reported a mesh sensation as a foreign object during the postoperative follow-up, and no recurrence was observed (Table II).
DISCUSSION
Inguinal hernia is a common and frequently-occurring disease in clinical practice. The present study aimed to evaluate the clinical outcomes and safety of the adopted two-point fixation method for a small intestine submucosal matrix biological mesh placed via laparoscopic TEP repair of inguinal hernia.
This modified suturing procedure was performed with a 4-0 Ethicon absorption thread used for a two-point fixation of a biological mesh. In this procedure, the suturing was easy to perform and with a short duration, with a low risk of bleeding, while the fixation was reliable, avoiding the disadvantages of conventional suturing. This procedure was safe and reliable as the 2-dimensional material in the extraperitoneal space required only two points for fixation. In addition, the mesh was fixed at the bilateral sides of the inferior epigastric artery at the level above the iliopubic tract, which prevented interference with major nerves and blood vessels. The proper selection of the suturing sites avoided contact with nerves as the thread loop was maintained slightly loose during the knotting. Therefore, even if nerves or muscles had been captured in the loop, they would not have been entrapped.
In a recent study, Aliyazicioglu et al. used a 3-dimensional synthetic mesh without fixation and achieved the shortest known so far surgery time of 55 minutes for bilateral hernia repair and 38 minutes for unilateral hernia repair.14 However, biological meshes are softer and with poorer adhesiveness than synthetic meshes, and, despite their advantage of degradability, they demand more preparation time.15 Another observational study reported applying the procedure of curtain closing to facilitate mesh flattening, which also reduced the required surgical time.16 In this study, the surgical time was 60 (48–62.2) minutes, during which certain difficulties and challenges were encountered, including the proper flattening and fixing of the biological mesh to avoid positional shifting and consequent postoperative recurrence.
Biological meshes could easily shift their position and wrinkle if not appropriately fixed, leading to hernia recurrence. Therefore, fixation is required, mainly done by suture, staple, and adhesion fixation.17 Based on the present experience and the results of published studies, the authors concluded that staple fixation involved an increased risk of postoperative pain and hematoma, whereas biogel fixation demanded the biological mesh to be water-immersed for hydration before delivery through the trocar into the surgical area, which may lead to dilution and a decrease in the concentration of the sprayed biogel, consequently causing adhesion failure and recurrence.18
In this study, the puncture outfit (olecranoid anastomat for the abdominal wall) was used to puncture the skin and underlying layers, and then the corresponding fixation sites of the biological mesh were punctured at 2–3 cm from the bilateral sides of the inferior epigastric artery at the level above the iliopubic tract. Suturing the two points generally took less than 5 min and contributed to reducing the total surgery time almost to the time of the procedure without fixation. To the best of authors’ knowledge, this study is the first to adopt this procedure for two-point fixation of a biological mesh using the described techniques, successfully reducing the surgery time.
CONCLUSION
Two-point fixation procedure is safe, reliable, rapid, easy to perform, and could potentially reduce postoperative complications. In addition, laparoscopic herniorrhaphy and the application of biological meshes could decrease the recovery time and postoperative pain and is thus worth being popularised in clinical practice.
FUNDING:
This study was supported by Wu Jieping Medical Foundation (Grant No. 320.6750.19091-15).
ETHICAL APPROVAL:
The research was approved by the Ethics Committee of the Hospital (Approval No. MRCTA, ECFAH of FMU [2019]187).
PATIENT’S CONSENT:
All participants provided written informed consent.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
GL, SW: Design topics, drafting, and editing of the manuscript.
YC, YH, JZ: Data collection and follow-up.
GL, YC: Data analysis.
REFERENCES
- Mehta A, Hutfless S, Blair AB, Dwarakanath A, Wyman CI, Adrales G, et al. Emergency department utilisation and predictors of mortality for inpatient inguinal hernia repairs. J Surg Res 2017; 212:270-7. doi: 10.1016/j.jss.2016. 12.012.
- Kudsi O, Bou-Ayash N, Gokcal F. Robotic transabdominal preperitoneal repair of complex inguinal hernias. Int J Abdominal Wall Hernia Surg 2021; 4(1):1-6.
- Carter J, Duh QY. Laparoscopic repair of inguinal hernias. World J Surg 2011; 35(7):1519-25. doi: 10.1007/s00268- 011-1030-x.
- Hirabayashi T, Kobayashi T, Saitoh T, Kimura T, Hakamada K. Surgical treatment of inguinal hernia in neonates and infants: Early surgery or elective surgery? Int J Abdominal Wall Hernia Surg 2020; 3(3):94-9.
- Techapongsatorn S, Tansawet A, Kasetsermwiriya W, McEvoy M, Attia J, Wilasrusmee C, et al. Mesh fixation technique in totally extraperitoneal inguinal hernia repair - A network meta-analysis. Surgeon 2019; 17(4):215-24. doi: 10.1016/j.surge.2018.09.002.
- Bhangu A, Singh P, Pinkney T, Blazeby JM. A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia 2015; 19(1):65-75. doi: 10.1007/s10029-014-1299-4.
- Molegraaf M, Kaufmann R, Lange J. Comparison of self-gripping mesh and sutured mesh in open inguinal hernia repair: A meta-analysis of long-term results. Surgery 2018; 163(2):351-60. doi: 10.1016/j.surg.2017.08.003.
- Rausa E, Asti E, Kelly ME, Aiolfi A, Lovece A, Bonitta G, et al. Open inguinal hernia repair: A network meta-analysis comparing self-gripping mesh, suture fixation, and glue fixation. World J Surg 2019; 43(2):447-56. doi: 10.1007/ s00268-018-4807-3.
- van’t Riet M, de Vos van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ. Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surgical Endosc 2002; 16(12):1713-6. doi: 10.1007/s00464-001- 9202-7.
- Suwa K, Nakajima S, Uno Y, Suzuki T, Sasaki S, Ushigome T, et al. Laparoscopic modified Sugarbaker parastomal hernia repair with 2-point anchoring and zigzag tacking of Parietex™ Parastomal Mesh technique. Surgical Endosc 2016; 30(12):5628-34. doi: 10.1007/s00464-016-4927-5.
- Ruiz-Jasbon F, Ticehurst K, Ahonen J, Norrby J, Falk P, Ivarsson ML Results at 3-year follow-up of totally extraperitoneal (TEP) hernia surgery with long-term resorbable mesh. Hernia 2020; 24(3):669-76. doi: 10. 1007/s10029-019-02116-2.
- Vărcuş F, Duţă C, Dobrescu A, Lazăr F, Papurica M, Tarta C. Laparoscopic repair of inguinal hernia TEP versus TAPP. Chirurgia Bucharest Romania 1990 2016; 111(4):308-12.
- Zhang Y, Chen Y, Zhao B, Gao J, Xia L, Xing F, et al. Detection of Type I and III collagen in porcine acellular matrix using HPLC-MS. Regen Biomater 2020; 7(6):577-82. doi: 10.1093/rb/rbaa032.
- Aliyazicioglu T, Yalti T, Kabaoglu B. Laparoscopic Total Extraperitoneal (TEP) Inguinal Hernia Repair Using 3-dimensional Mesh Without Mesh Fixation. Surg Laparosc Endos Percutan Tech 2017; 27(4):282-4. doi: 10.1097/SLE. 0000000000000423.
- Seefeldt CS, Meyer JS, Knievel J, Rieger A, Geißen R, Lefering R, et al. BIOLAP: Biological versus synthetic mesh in laparo-endoscopic inguinal hernia repair: Study protocol for a randomised, multicenter, self-controlled clinical trial. Trials 2019; 20(1):55. doi: 10.1186/s13063-018-3122-5.
- Gutlic N, Rogmark P, Nordin P, Petersson U, Montgomery A. Impact of mesh fixation on chronic pain in total extra-peritoneal inguinal hernia repair (TEP): A nationwide register-based study. Ann Surg 2016; 263(6):1199-206. doi: 10.1097/SLA.0000000000001306.
- Weng H, Ye L, Lu P, Sun H. Application of shaft method assisted biological mesh in laparoscopic inguinal hernia repair. Medicine 2018; 97(46):e12923. doi: 10.1097/MD. 0000000000012923.
- Agresta F, Bedin N. Transabdominal laparoscopic inguinal hernia repair: Is there a place for biological mesh? Hernia 2008; 12(6):609-12.