Tracheal Bronchus in Children
By Shi-Min YuanAffiliations
doi: 10.29271/jcpsp.2023.06.684ABSTRACT
Tracheal bronchus is an uncommon congenital anomaly. It is often of important significance during endotracheal intubation. In paediatrics with tracheal bronchus, stenosis of trachea and (or) bronchus and the management strategies remain to be further clarified. A comprehensive retrieval of literature since 2000 revealed 43 articles with 334 paediatric patients with tracheal bronchus. The delayed diagnosis rate is 4.1%. Paediatric patients with tracheal bronchus most often present with recurrent pneumonia and atelectasis. In less than one-third of the patients, there was an intrinsic or extrinsic stenosis of the trachea, which warrant a conservative or a surgical treatment. A surgical treatment was performed in 15.3% of the patients, in most of which the operations were for relieving the tracheal stenosis. The surgical outcomes were satisfactory. Paediatric patients with tracheal bronchus with tracheal stenosis and recurrent pneumonia and persistent atelectasis warrant active treatments, and surgical treatments are preferred. No treatment is needed in those with no tracheal stenosis or those with no or mild symptoms.
Key Words: Abnormality, Congenital, Thoracic surgery, Tracheal stenosis.
INTRODUCTION
Tracheal bronchus was defined as a bronchus originating directly from the trachea, either above or at the level of the carina.1 The frequency of tracheal bronchus was 0.31% in patients for multidetector computed tomography scans,2 and 1.9% in patients for flexible bronchoscopy.3 The incidence of tracheal bronchus detected in young children was 1.06%.4 The tracheal bronchus is usually located at the junction of the mid and distal thirds of the trachea, originating from the right lateral wall of the trachea 2cm proximal to the carina and supplying the upper lobe or its apical segment.5 Tracheal bronchus can be displaced or supernumerary.6 It may have different sizes and angles, and can be tiny, stenotic, or blind-ended.7 The angle between the tracheal bronchus and trachea varied from 22° to 108° with a mean of 73°.8
There are various classifications of tracheal bronchus reported in the literature. Moreno et al. elaborated the anatomical classification of tracheal bronchus into three types: Type I, arising from the junction of the middle and lower third of the trachea with a decrease in the distal tracheal diameter; type II, arising from the lower third without modification of the tracheal size; and type III, arising almost at the level of the carina and giving the appearance of a trifurcated carina.1
A mistaken cannulation of type I tracheal bronchus might obstruct the rest of respiratory system; type II tracheal bronchus might be obstructed by a normal tracheal tube; and type III might cause problems for one-lung ventilation.
At least half of the patients with pulmonary artery sling are associated with tracheal and bronchial stenosis and complete tracheal cartilage rings.6 When the distal trachea is severely compressed in the anterior and posterior directions, the right main bronchus is usually severely narrowed, or even leaving only one slit.6 Tracheal reconstruction and the left pulmonary artery re-implantation are the effective ways for relieving airway obstruction due to tracheal stenosis.6 Tracheal stenosis and airway obstruction are also a prominent problem in patients with tracheal bronchus with or without a pulmonary artery sling or other vascular rings. Patients with tracheal bronchus may have intrinsic or extrinsic stenosis of trachea and (or) bronchus, which may further lead to respiratory symptoms or recurrent respiratory infections. Morita et al.6 classified congenital tracheal stenosis in patients with tracheal bronchus into 3 types: Type 1, tracheal stenosis above the right-upper lobe bronchus; type 2, tracheal stenosis below the right upper lobe bronchus and type 3, tracheal stenosis above the right upper lobe bronchus to the carina. However, the diagnosis and treatment of tracheal stenosis in patients with tracheal bronchus have not been elucidated in detail. In fact, majority of reports on tracheal bronchus focus on that of the right side, as most of the instances were seen on the right. There are also tracheal bronchus originating from the left side or bilaterally. Moreover, in spite of constantly reported tracheal bronchus, the anatomical and clinical features of tracheal bronchus in paediatric patients have not been sufficiently evaluated so far. In paediatrics with tracheal bronchus, stenosis of trachea and (or) bronchus and the management strategies remain to be further clarified. The aim of this review was to give an overview of the tracheal bronchus in paediatric patients in terms of anatomical and clinical aspects of this anomaly.
METHODOLOGY
Comprehensive retrieval of pertinent literature in the PubMed, Google Scholar, and Baidu Scholar was done for English articles published between 2000 and 2022. The reference lists after the text of the recruited publications and conference abstracts were also carefully screened for a complete retrieval of the literature. It was tried to search randomised controlled trials, but retrospective studies, case series and case reports on tracheal bronchus of paediatric patients were also included. The retrieval terms included aberrant bronchus, tracheal bronchus, eparterial bronchus, pig bronchus, bronchus suis, tracheal trifurcation and tracheal quadrifurcation, with a filter of paediatrics. The inclusion criteria were the clinical prospective or retrospective researches, cohort studies, case series and case reports of tracheal bronchus. The primary exclusion criteria were publications with, no substantial information of tracheal bronchus patients (n=3), tracheal bronchus of adult patients (n=2), middle aberrant bronchus (n=1), congenital absence of the right upper lobe bronchus (n=1), airway anomaly with congenital diaphragmatic hernia (n=1), ectopic right lower lobe (n=1), anomalous tracheobronchial arborisation (n=1), congenital tracheal stenoses (n=1) and bridging bronchus (n=1). As a result, a total of 43 articles were included and 12 articles were excluded with 334 patients included. A flowchart of the retrieval policy was shown in Figure 1.
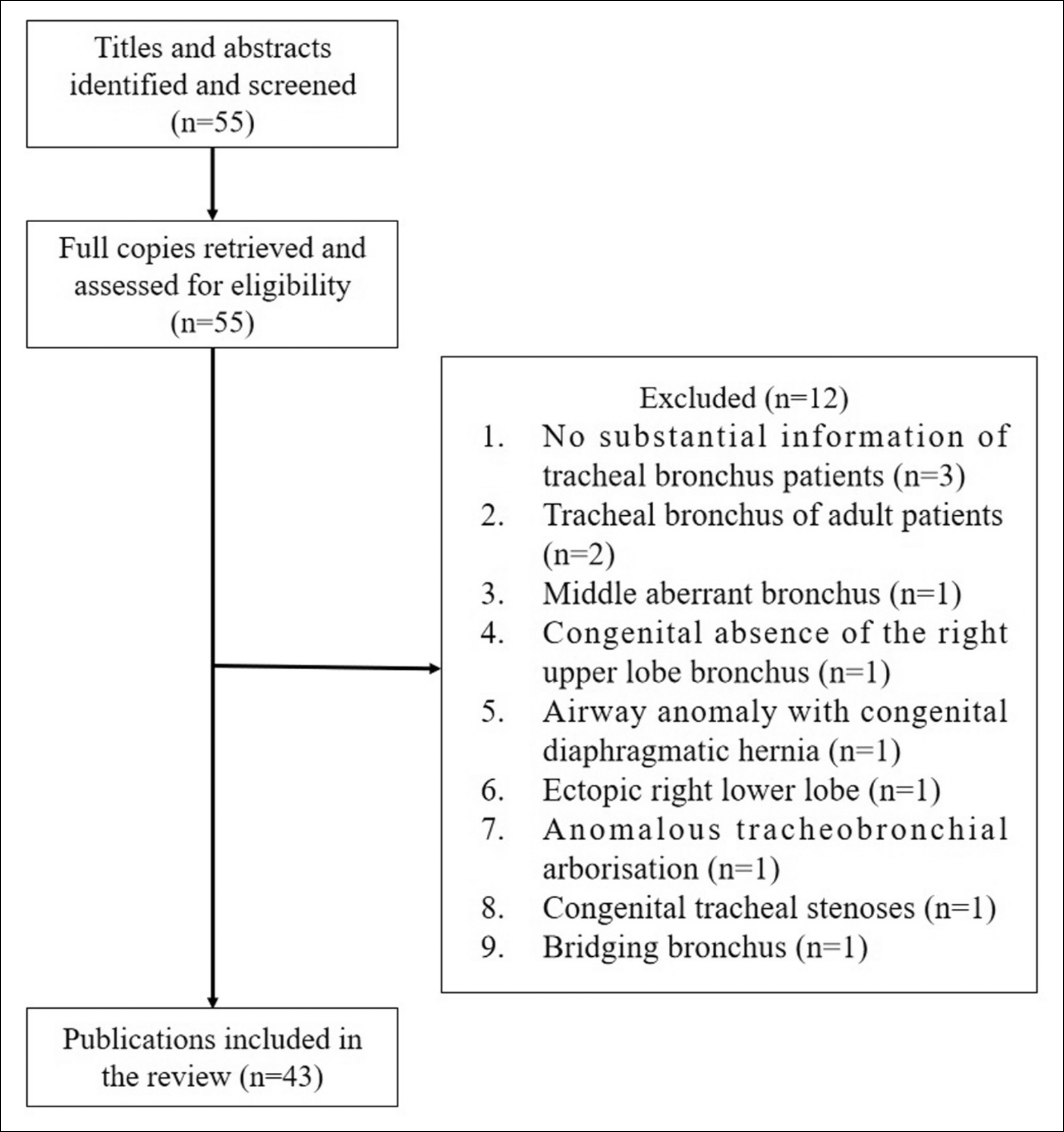 Figure 1: A flowchart of literature retrieval policy.
Figure 1: A flowchart of literature retrieval policy.
The data independently extracted from each study were the study population, demographics, clinical manifestations, classifications of tracheal bronchus, therapeutic strategies, procedures performed, effectiveness, and patient outcomes. Data extraction was taken by way of tabulating all the necessary information of each report. This process was replicated three times by three different reviewers to avoid omissions and ensured the integrity and credibility of the data. During the course, three reviewers independently reviewed titles, abstracts, and full texts as needed to determine whether studies met the inclusion criteria. In cases of conflict between the reviewers, additional review and analysis were undertaken to resolve the issue. In instances where heterogeneity existed, the effect of each study was examined on the overall effect by removing individual studies.
IBM SPSS statistics version 22 software was used for statistical analysis. The measurement data were expressed as mean ± standard deviation and median (range) while categorical data were given as numbers and percentages. The categorical variables were compared by Chi-square or Fisher exact test with continuity correction. Logistic regression analysis was performed to evaluate the determinants of treatment of choice for tracheal stenosis. The value of p<0.05 was considered as statistical significant. A P-P plot was used to estimate a normal distribution of patient age. MedCalc version 20.014 was used to draw a forest plot of OR (95%CL) of logistic regression analysis.
RESULTS
The 43 recruited articles included 33 (76.7%) case reports,8-16,18-30,34-42,44,45 3(7.0%) case series,17,31,43 and 7(16.3%) retrospective studies.1,3-5,7,32,33 There was no prospective study found in the literature.
There were a total of 334 patients, with 120 (52.9%) male and 107 (47.1%) female patients with a male-to-female ratio of 1.1:1, while gender was not given for the remaining 107 patients. Patients were at the age of 2.2±3.3 (range, 0–15; median, 0.7) years (n=61). The patients’ age was in a normal distribution.
The symptoms were not reported for 59 (17.7%) patients. Of the remaining 275 (82.3%) patients, 34 (12.4%) patients were asymptomatic,3,5,16,33,34,39,40 and 241 (87.6%) patients had a total of 309 common or severe/critical symptoms (Table I).
The diagnostic techniques were not stated at all or were not clearly indicated in 3 reports for a total of 194 patients,1,5,7 In the remaining 140 patients, the diagnostic techniques for reaching a definite diagnoses of tracheal bronchus were by bronchoscopy in most instances (Table II).
In 14(4.1%) patients, the tracheal bronchus had a delayed diagnosis.9,10,19,23-28,31,36 The delayed time was 7.9±8.3 (range, 0.3–24; median, 4) months (n=13).
Table I: The 309 clinical presentations of 241 patients.
|
Clinical presentation |
n (%) |
|
Common symptoms |
|
|
Stridor8,17,30–32,35,42 |
8 (3.3) |
|
Asthma32 |
6 (2.5) |
|
Wheeze3,18,31,36 |
5 (2.1) |
|
Acquired subglottic stenosis1 |
3 (1.2) |
|
Cough9,17,37 |
3 (1.2) |
|
Aspiration8,17 |
2 (0.8) |
|
Cyanosis41,44 |
2 (0.8) |
|
Cyanotic episode31,35 |
2 (0.8) |
|
Dysphagia8,31 |
2 (0.8) |
|
Failing to thrive22,31 |
2 (0.8) |
|
Feeding difficulties31 |
2 (0.8) |
|
Respiratory symptoms, unspecified5 |
23 (9.5) |
|
Severe/critical symptoms |
|
|
Recurrent pneumonia1,3,7,9-14,17,19,23-25,29-32,35,38,42-45 |
111 (46.1) |
|
Atalectasis1,3,10,17,21,32,41 |
67 (27.8) |
|
Difficult/failed intubation1,3,5,15,20 |
20 (8.3) |
|
Ventilation-dependent7,10,22,24,26,27,31,42,43 |
19 (7.9) |
|
Respiratory distress10,14,18,19,21-23,25-29,35,41,43 |
15 (6.2) |
|
Vascular compression3,21,23-25,28,32,41 |
13 (5.4) |
|
Respiratory arrest19,44 |
2 (0.8) |
|
Preintubation laryngospasm4 |
1 (0.4) |
|
Cardiopulmonary bypass-dependent7 |
1 (0.4) |
Table II: The diagnostic techniques for the definite diagnosis of tracheal bronchus in 140 patients.
|
Diagnostic technique |
n (%) |
|
Bronchoscopy/laryngoscopy |
122 (87.1) |
|
Bronchoscopy, flexible3,15,21,22,24-26,31,32,37 |
91 (74.6) |
|
Bronchoscopy, rigid4,10 |
12 (9.8) |
|
Bronchoscopy, unspecified8,11,12,14,17,18,33,36,42,43 |
15 (12.3) |
|
Laryngoscopy, direct8 |
1 (0.8) |
|
Laryngobronchoscopy, rigid31 |
3 (2.5) |
|
Bronchography18,22,27,31,38 |
5 (3.6) |
|
Computed tomography3,8,9,11-14,16,17,20,21,23,25,27,29,31,33,35,36,40,42-45 |
29 (20.7) |
|
Three-dimensional computed tomography24,30,40,42,44 |
5 (3.6) |
|
Computed tomographic angiography28,41 |
2 (1.4) |
|
X-ray film40 |
1 (0.7) |
|
Intubation39 |
1 (0.7) |
|
Operation34 |
1 (0.7) |
|
Autopsy19 |
1 (0.7) |
Table III: Tracheal stenosis.
|
Tracheal stenosis |
n (%) |
|
Intrinsic |
88 (26.3) |
|
Tracheal stenosis |
74 (84.1) |
|
Type 15,7 |
2 (2.7) |
|
Type 25,7,22,26-28,30,31,38,44 |
20 (27.0) |
|
Type 37,35 |
6 (8.1) |
|
Type unspecified1,3,5,32 |
46 (62.2) |
|
Bronchial stenosis |
13 (14.8) |
|
Right intermediate bronchus43 |
2 (15.4) |
|
Right tracheal bronchus + left lower bronchus13 |
1 (7.7) |
|
Ostium/orifice8,33 |
3 (23.1) |
|
Right tracheal bronchus5,33 |
3 (23.1) |
|
Right main bronchus17,28 |
2 (15.4) |
|
Bronchial stenosis, unspecified3 |
2 (15.4) |
|
Carina stenosis4 |
1 (0.3) |
|
Extrinsic vascular compression3,21,23-25,28,32,41 |
13 (3.9) |
|
No stenosis1,3,4,5,9-12,14-20,29,32,34,36,37,39,40,42,45 |
235 (70.4) |
|
* One patient had simultaneously intrinsic tracheal and bronchial stenoses and vascular compression.28 |
|
Table IV: A comparison of prognosis between patients receiving a conservative and a surgical treatment.
|
Treatment |
Recovered |
Unchanged |
Worsened |
Complicated |
Died |
|
Conservative (n=126) |
98 (77.8) |
1 (0.8) |
22 (17.5) |
|
5 (4.0) |
|
Surgical (n=28) |
19 (67.9) |
|
1 (3.6) |
8 (28.6) |
|
|
χ2 |
1.2 |
0.2 |
5.2 |
38.0 |
1.1 |
|
p |
0.328 |
>0.990 |
0.025 |
<0.001 |
0.585 |
|
* Fisher exact test with continuity correction. |
|||||
The types of tracheal bronchus were unknown for 22 (6.6%) patients. Of the remaining 312 (93.4%) patients, tracheal bronchus was on the right in 304 (97.4%) (including 67 type I, 70 type II, 64 type III, and 103 cases of type I or II. One (0.3%) tracheal bronchus was on the left, which was type I.21 Seven (2.2%) patients had bilateral tracheal bronchi, which were types I,44 II 5,41,42 and III13 in 1, 5 and 1 patient, respectively (Figure 2).5-45
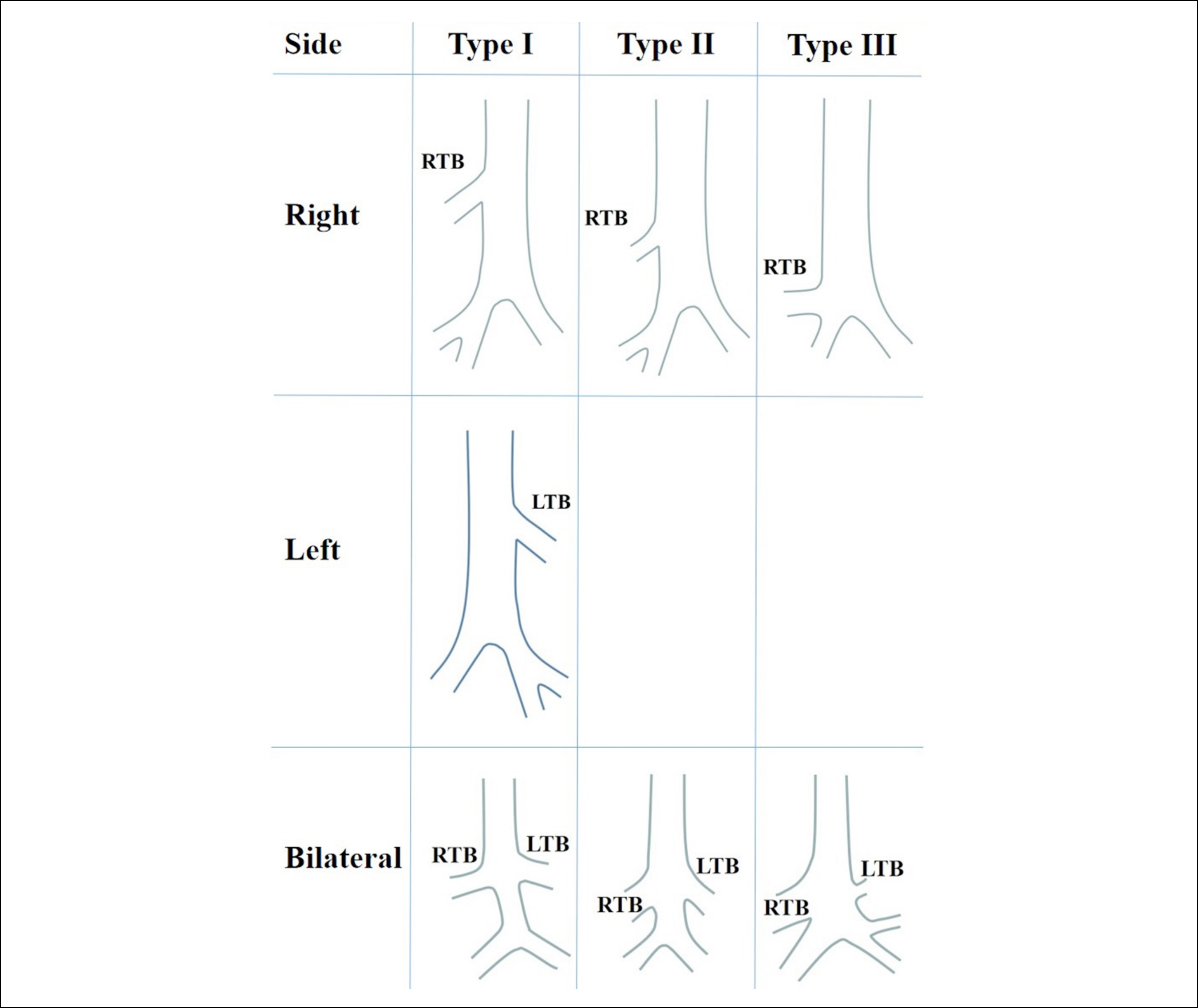 Figure 2: Classifications of displaced tracheal bronchi in paediatric patients: right tracheal bronchus (upper panel); left tracheal bronchus (middle panel); and bilateral tracheal bronchi (lower panel). LTB: left tracheal bronchus; RTB: right tracheal bronchus.
Figure 2: Classifications of displaced tracheal bronchi in paediatric patients: right tracheal bronchus (upper panel); left tracheal bronchus (middle panel); and bilateral tracheal bronchi (lower panel). LTB: left tracheal bronchus; RTB: right tracheal bronchus.
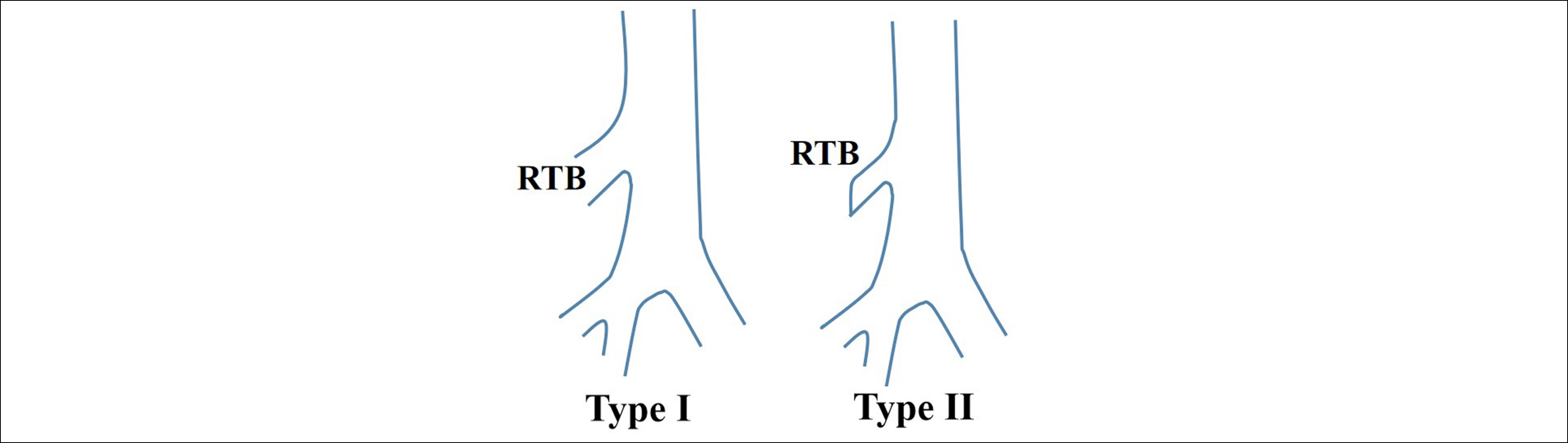 Figure 3: The supernumerary right tracheal bronchi: Type I, patent tracheal bronchus, and type II, tracheal bronchus with a blind end. RTB: Right tracheal bronchus.
Figure 3: The supernumerary right tracheal bronchi: Type I, patent tracheal bronchus, and type II, tracheal bronchus with a blind end. RTB: Right tracheal bronchus.
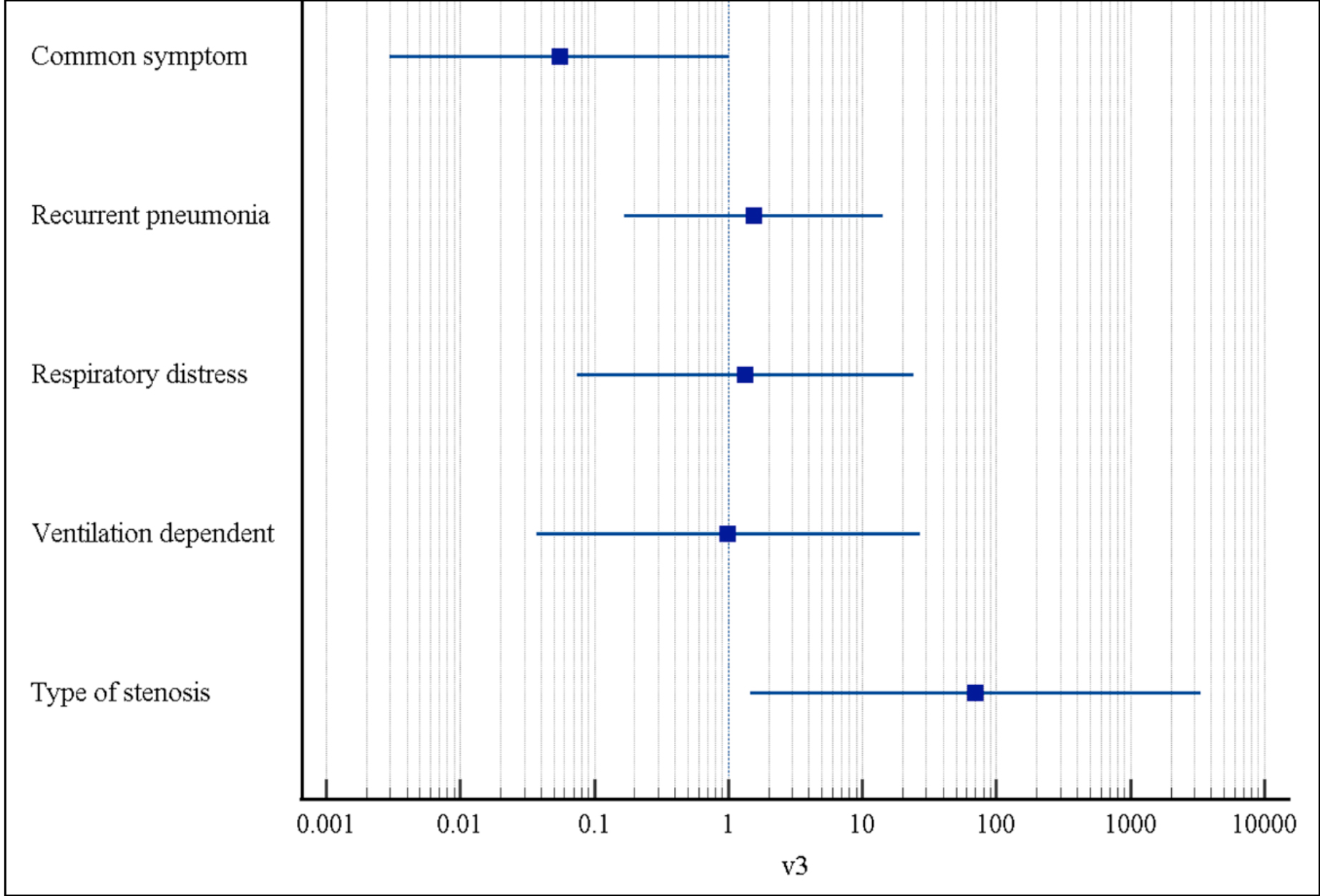 Figure 4: A forest plot of OR (95%CL) of logistic regression analysis.
Figure 4: A forest plot of OR (95%CL) of logistic regression analysis.
Of the left tracheal bronchus, a tracheal diverticulum was found in 2 cases.31,34 Of the left tracheal bronchus patients, a supernumerary tracheal bronchus was reported in 55 (55/304, 18.1%) patients (Figure 3), including 20 supernumerary lobar (20/55, 36.4%),1,3,17 14 supernumerary segmental (14/55, 25.5%),1,3 18 supernumerary unspecified (18/55, 32.7%),32 and 3 blind supernumerary tracheal bronchus (3/55, 5.5%) cases.17,32 Presumably all the remaining 249 (249/304, 81.9%) left tracheal bronchi were displaced.
The originating aspects from the trachea were only reported for 44 patients: It was from the right wall in 26 patients,3 from the right lateral wall in 15 patients,4,14,17,18,23 from the right posterolateral wall in 2 patients,20,25 and from the right posterior wall in 1 patient.24
In all 235 (70.4%) patients had no tracheal stenosis, whereas 99 (29.6%) patients had intrinsic and (or) extrinsic tracheal stenosis. Intrinsic tracheal stenosis was noted in 88 (88.9%) patients, and extrinsic vascular compression was present in 13 (13.1%) patients (Table III). One patient had simultaneously intrinsic tracheal and bronchial stenoses and vascular compression.28 Complete tracheal rings were present in 22 (6.6%) patients,3,7,22,26,27,31,33 and the absence of tracheal rings was found in 2 (0.6%) patients.35,38
A logistic regression analysis was performed between treatment strategy and symptoms and types of tracheobronchial stenosis. It was illustrated that the type of tracheobronchial stenosis was a determinant of treatment of choice (p=0.031), and common symptom was almost a determinant (p=0.057). A forest plot of the OR (95% CI) was shown in Figure 4.
One hundred and fifty-six (46.7%) patients had associated congenital heart defects,1,3,5,10,13,14,16-18,21-28,31-33,36,40,41,43 and 87 (26.0%) patients had genetic, chromosomal, or other congenital anomalies.1,3, 4,8,10,13,15,17,19,20,22,31-34,38
Treatment was not mentioned for 151 patients. Of the remaining 183 patients, 15 (8.2%) patients were not treated due to no or mild respiratory symptoms, patient refusal, surgical planned but not yet performed, or sudden death.16-20,22,31,34-37,39,40
One hundred and thirty-nine (76.0%) patients were conservatively managed with adrenaline nebulisation, antibiotic, or intubation with oxygen supply,1,9,10,12,14,17,30 1 (0.5%) patient was treated interventionally (rigid broncholaryngoscopy with CO2 laser and balloon dilation of subglottic stenosis),31 and 28 (15.3%) patients were treated surgically,7,11,17,21,23-287,31,38,41,43-45 including slide tracheobronchial plasty (n=11),7,26,43,44 tracheal end-to-end anastomosis (n=7),7,38 right upper lobe diverticulum resection (n=1),31 lobectomy (n=3),17,25,45 right arteriopulmonary shunt operation (n=1),41 patent ductus arteriosus ligation, and the left-upper lobectomy with the resection of the tracheal bronchus (n=1),21 resection of the dysplastic tracheal segment and right upper lobe pulmonary artery transected and ligated (n=1),27 aortic and pulmonary arteriopexies (n=1),24 and pulmonary arteriopexy operation for pulmonary artery sling (n=2).23,28 Operations were performed under cardiopulmonary bypass in 7 (25%, 7/28) patients.26-28,38,43,44
The patients were on a follow-up of 45.1±57.5 (range, 0.3–240; median, 24) months (n=20). The prognoses were known for 174 patients: 138 (79.3%) patients recovered, 1 (0.6%) patient significantly improved, 1 (0.6%) patient unchanged, 23 (13.8%) patients had a poor or a worsened prognosis, 10 (5.7%) patients were complicated and 6 (3.4%) patients died (5 of them were with poor prognoses). The postoperative complications were stridor (n=1), delirium (n=1),4 dehiscence of the anastomosis (n=1), remaining tracheal stenosis (n=1), stenosis of the anastomotic site (n=1), severe tracheomalacia at the anastomotic site or a remaining complete tracheal ring (n=2),7 malacia (n=1)24 and granulation tissue formation in the trachea or at the carina (n=2).28,31
A comparison of prognosis between patients receiving a conservative and a surgical treatment revealed that the conservatively treated patients had more patients with a poor prognosis and a higher mortality (Table IV).
DISCUSSION
The diagnosis of tracheal bronchus can be made by rigid and flexible bronchoscopy or by computed tomography. The findings of intubation or surgery, bronchoscopy, or bronchography can be the gold standard for diagnosis of tracheal bronchus.5 Bronchoscopy can differ an undeveloped from a normally developed tracheal bronchus by a direct visualisation, and it can also judge whether the supply of the tracheal bronchus is lobar or segmental.17 It was proposed that the diagnostic sensitivity of tracheal bronchus was 100% by computed tomography, and was 16.7% by chest radiograph.5
Tracheal bronchus is usually asymptomatic and an incidental finding on bronchoscopy, but in paediatric patients it can be associated with recurrent infections, stridor, and thoracic masses.46
The aberrant course of the tracheal bronchus makes it vulnerable to obstruction. This can result in lobar collapse and infection due to retained secretions.9 Tracheomalacia is weakening and increased collapsibility of airway cartilages causing stridor, cough, impaired clearance of secretion, and recurrent respiratory infections.30 Recurrent atelectasis and infection in the affected pulmonary segments may contribute to increased mortality and pulmonary morbidity.10 During intubation, a tracheal tube can occlude the orifice of the tracheal bronchus, resulting in atelectasis of the supplied lobe or segment.5 A mistaken intubation into the tracheal bronchus may cause insufficient ventilation of the remaining lung.5 Early recognition of the anomaly allows for appropriate endotracheal tube positioning and respiratory management.10
Tracheal bronchus and tracheal stenosis association is rare, but the association between tracheal bronchus and stenosis of the right main bronchus to cause obstructive symptoms and recurrent pulmonary infections.24 Complete cartilaginous rings3 and absent tracheal rings have been taken as the causes of intrinsic stenosis of the trachea. Spontaneous resolution may occur within the first 2 years of life.35 Tracheostomy, stenting or surgery is required in severe and non-resolving cases.30 An arteriopexy is necessary for the relief of external vascular compression, and for eliminating the possible collapse of the distal trachea.24
The present study revealed paediatric patients with tracheal bronchus most often present with recurrent pneumonia and atelectasis. In less than one-third of the patients, there was an intrinsic or extrinsic stenosis of the trachea, which warrant a conservative or a surgical treatment. For patients with an intrinsic tracheal stenosis, a slide tracheobronchial plasty or tracheal end-to-end anastomosis can be practical, and for those with an extrinsic stenosis, arteriopexy operation should be performed. A lobectomy can be considered for patients with recurrent pneumonia and persistent atelectasis.
CONCLUSION
The diagnosis of tracheal bronchus sometimes poses challenges. The delayed diagnosis rate is 4.1%. Paediatric patients with tracheal bronchus with tracheal stenosis and recurrent pneumonia and persistent atelectasis warrant active treatments and surgical treatments are preferred. No treatment is needed in those with no tracheal stenosis or those with no or mild symptoms.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SMY: Substantial contribution to the conception and design of the work; and the acquisition, analysis, and interpretation of data for the work; drafting the work and revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved.
REFERENCES
- Moreno M, Castillo-Corullón S, Pérez-Ruiz E, Luna MC, Antón-Pacheco JL, Mondejar-Lopez P, et al. Spanish multicentre study on morbidity and pathogenicity of tracheal bronchus in children. Pediatr Pulmonol 2019; 54(10): 1610-6. doi: 10.1002/ppul.24435.
- Suzuki M, Matsui O, Kawashima H, Takemura A, Matsubara K, Hayashi N, et al. Radioanatomical study of a true tracheal bronchus using multidetector computed tomography. Jpn J Radiol 2010; 28(3):188-92. doi: 10.1007/s11604-009- 0405-5.
- Pérez Ruiz E, Caro Aguilera P, Valdivielso AI, Sanchís Cárdenas S, Martínez García Y, Pérez Frías J. Tracheal bronchus diagnosed in children undergoing flexible bronchoscopy. Paediatr Respir Rev 2018; 28:26–30. doi: 10. 1016/j.prrv.2018.03.009.
- Dave MH, Gerber A, Bailey M, Gysin C, Hoeve H, Hammer J, et al. The prevalence of tracheal bronchus in paediatric patients undergoing rigid bronchoscopy. J Bronchology Interv Pulmonol 2014; 21(1):26-31. doi: 10.1097/LBR.000 0000000000029.
- Ming Z, Hong S, Biao J. Images in cardiovascular medicine. Asplenia syndrome with bilateral tracheal bronchi. Circulation 2008; 118(2):196-7. doi: 10.1161/CIRCULATIONAHA.107.763458.
- Yuan SM, Shang H. Pulmonary artery sling. Mod Diagn Treat 1996; 7(5):287-8.
- Morita K, Yokoi A, Fukuzawa H, Hisamatsu C, Endo K, Okata Y, et al. Surgical intervention strategies for congenital tracheal stenosis associated with a tracheal bronchus based on the location of stenosis. Pediatr Surg Int 2016; 32(9):915-9. doi: 10.1007/s00383-016-3928-8.
- Adetayo OA, Suskind DL. Radiology quiz case: Tracheal bronchus. Arch Otolaryngol Head Neck Surg 2006; 132(4):453-4. doi: 10.1001/archotol.132.4.453.
- Alqahtani SA, Alghamdi AM, Babader RA, Aljehani DA, Alsultan RK, Mushari RY, et al. Tracheal bronchus: A rare etiology of recurrent pneumonia in children. Cureus 2021; 13(12):e20378. doi: 10.7759/cureus.20378.
- Ashmeade T, Carver JD. Right tracheal bronchus in an infant with congenital diaphragmatic hernia. Am J Perinatol 2009; 26(9):621-3. doi: 10.1055/s-0029-1220779.
- Bakir B, Terzibasioglu E. Images in clinical medicine. Tracheal bronchus. N Engl J Med 2007; 357(17):1744. doi: 10.1056/NEJMicm064503.
- Barros D, Rio G, Mendes V. Tracheal trifurcation: An uncommon cause of recurrent pneumonia. Arch Bronconeumol (Engl Ed) 2021; 57(3):229. doi: 10.1016/j.arbres. 2020.03.007.
- Bhat V, Gadabanahalli K, Ahmad O. Tracheal quadrifurcation associated with congenital heart disease. Pediatr Radiol 2015; 45(8):1236-8. doi: 10.1007/s00247-015-3309-9.
- Chau KW, Ng DK, Chong AS, Lau A. Tracheal bronchus. Hong Kong Med J 2003; 9(1):71-2.
- Delpizzo KR, Joffe DC, Finkel JC. Tracheal bronchus in 10-month-old patient for thoracoscopic resection of congenital cystic adenomatoid malformation. Paediatr Anaesth 2006; 16(9):997-8. doi: 10.1111/j.1460-9592.2006.01900.x.
- Doğan V, Ertuğrul İ, Taşcı Yıldız Y, Örün UA, Karademir S. A case of tracheal bronchus associated with right aortic arch and partial anomalous pulmonary venous connection. Turk Kardiyol Dern Ars 2016; 44(8):703-5. doi: 10.5543/tkda. 2016.83903.
- Doolittle AM, Mair EA. Tracheal bronchus: classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 2002; 126(3):240-3. doi: 10.1067/mhn.2002.122703.
- Elmaci TT, Güler N, Aydoğan U, Onursal E. Infantile lobar emphysema and tracheal bronchus in a patient with congenital heart disease. J Pediatr Surg 2001; 36(10): 1596-8. doi: 10.1053/jpsu.2001.27067.
- Hansen-Welches L, Slabach R, Landrum JE, Prahlow JA. Death of a 6-month-old due to a tracheal bronchus. Am J Forensic Med Pathol 2011; 32(3):219-22. doi: 10.1097/PAF.0b013e31822a62b7.
- Jain D, Bhardwaj N, Pareek A, Parikh B. Tracheal bronchus: An unusual cause of difficult ventilation. Can J Anaesth 2017; 64(9):979–80. doi: 10.1007/s12630-017-0919-8.
- Joseph L, Cytter Kuint R, Goldberg S, Picard E. Congenital left upper lobe emphysema due to vascular pressure on a left tracheal bronchus. Pediatr Int 2020; 62(3):407–8. doi: 10.1111/ped.14081.
- Kairamkonda V, Thorburn K, Sarginson R. Tracheal bronchus associated with VACTERL. Eur J Pediatr 2003; 162(3):165-7. doi: 10.1007/s00431-002-1109-3.
- Kocabaş A, Kardelen F, Akçurin G, Ertuğ H. Pulmonary artery sling and tracheal bronchus in an infant with severe respiratory distress. Anadolu Kardiyol Derg 2013; 13(6):E37. doi: 10.5152/akd.2013.222.
- Kuo SM, Yang ML, Li YC, Tsao TF, Liu SC, Chen FL. Balloon dilatation in management of postoperative airway obstruction due to tracheal bronchus associated with right main bronchial stenosis: Emphasizing the role of three-dimensional computed tomography on preoperative evaluation. Pediatr Pulmonol 2010; 45(7):730-3. doi: 10.1002/ppul. 21241.
- Kuriakose N, Al-Ismaili M, Raniga S, Date R, Al-Abady A, Al-Balushi Z. Airway and anaesthetic challenges in a child with bronchus suis and superimposed double aortic arch: A case report. Sultan Qaboos Univ Med J 2021; 21(1):e132-6. doi: 10.18295/squmj.2021.21.01.020.
- Le Bret E, Teissier N, Belli E, Sigal-Cinqualbre A, Couloignier V, Narcy P, et al. Slide tracheoplasty in the presence of tracheal bronchus in an infant. J Thorac Cardiovasc Surg 2006; 132(1):e15-6. doi: 10.1016/j.jtcvs.2006.03.033.
- Loukanov T, Sebening C, Springer W, Hagl S. A case of pulmonary artery sling associated with long-segment funnel trachea and bronchus suis. Ann Thorac Surg 2004; 78(5):1839-42. doi: 10.1016/j.athoracsur.2003.07.023.
- Lovett M, Entrikin D, Ungerleider R, Ootaki Y. Pulmonary artery sling and tracheal bronchus presenting in a 2-year-old child. Ann Thorac Cardiovasc Surg 2013; 19(4):302-4. doi: 10.5761/atcs.cr.12.01971.
- Manjunatha YC, Gupta AK. Tracheal bronchus (pig bronchus). Indian J Pediatr 2010; 77(9):1037-8. doi: 10.1007/s12098-010-0162-6.
- Mohakud S, Priyadarshini L. Tracheomalacia with tracheal bronchus. Natl Med J India 2018; 31(1):57. doi: 10.4103/ 0970-258X.243426.
- Rahmanian R, Zheng J, Chadha NK, Kozak FK, Campbell AI, Ludemann JP. False carina: A distinct variant of tracheal bronchus. Int J Pediatr Otorhinolaryngol 2015; 79(4):623-8. doi: 10.1016/j.ijporl.2015.01.023.
- Ruchonnet-Metrailler I, Abou Taam R, de Blic J. Presence of tracheal bronchus in children undergoing flexible bronchoscopy. Respir Med 2015; 109(7):846-50. doi: 10.1016/j. rmed.2015.04.005.
- Santangelo TP, Ottavianelli A, Curione D, Casazza I, Viglietti D, Agati S, et al. Tracheal trifurcation: New cases and review of the literature. Pediatr Radiol 2021; 51(10): 1848-55. doi: 10.1007/s00247-021-05075-y.
- Sarin YK. Tracheal trifurcation associated with esophageal atresia. APSP J Case Rep 2010; 1(2):14.
- Schwartz IE, Utz ER, Gaudreau PA. Congenital complete absence of tracheal rings with trifurcate carina: Case report of a rare clinical and endoscopic presentation. Int J Pediatr Otorhinolaryngol 2018; 111:1–6. doi: 10.1016/j.ijporl.2018. 05.009.
- Sprecher R, Josephson G. Tracheal bronchus in an 11-month-old infant. Ear Nose Throat J 2013; 92(10–11):505, 512.
- Srinivasan S, Mathew JL, Vaidya PC, Singh M. Tracheal bronchus and disseminated tuberculosis in a 9-year-old girl: Incidental finding or association? BMJ Case Rep 2020; 13(1):e231988. doi: 10.1136/bcr-2019-231988.
- Torre M, Speggiorin S, Roebuck DJ, McLaren CA, Elliott MJ. Congenital absence of cartilaginous tracheal rings associated with esophageal atresia and trifurcated carina: A novel anomaly? J Pediatr Surg 2012; 47(5):1008-11. doi: 10.1016/j. jpedsurg.2012.01.077.
- Tsukamoto M, Hirokawa J, Hitosugi T, Yokoyama T. Airway management for a paediatric patient with a tracheal bronchus. Anesth Prog 2018; 65(1):50-1. doi: 10.2344/anpr-64-04-02.
- Wang KL, Fu YC, Chan SC, Lin MC, Jan SL. "Uneven-sized eyes" sign on echocardiography in a young girl with pulmonary artery sling and tracheal bronchus. Acta Cardiol 2017; 72(1):81-2. doi: 10.1080/00015385.2017.1281532.
- Watabnabe K, Uese K, Higuchi O, Futatani T, Yoshimura N, Nakamura T, Ichida F. Three-dimensional computed tomographic findings of bilateral tracheal bronchus. Pediatr Cardiol 2009; 30(1):87-8. doi: 10.1007/s00246-008-9298-9.
- Wooten C, Doros C, Miclaus GD, Matusz P, Loukas M. A case of bilateral tracheal bronchus: Report of a rare association in multidetector computed tomography bronchoscopy. Surg Radiol Anat 2015; 37(6):693-6. doi: 10.1007/s00276- 014-1383-6.
- Wu ET, Yang MC, Wang CC, Lin MT, Chen SJ, Huang CH, et al. Congenital right intermediate bronchial stenosis with carina trifurcation: Successful management with slide tracheobronchial plasty. Ann Thorac Surg 2014; 98(1): 357-9. doi: 10.1016/j.athoracsur.2013.11.073.
- Yamoto M, Fukumoto K, Urushihara N. Tracheoplasty for congenital tracheal stenosis with bilateral tracheal bronchus. Ann Thorac Cardiovasc Surg 2022; 28(2):159-62. doi: 10.5761/atcs.cr.19-00198.
- Zhang Y, Qin M, Wang X, Yan Q. A rare anaesthetic challenge in a one-lung ventilated paediatric patient with right upper lobe tracheal bronchus. J Int Med Res 2020; 48(10):300060520967609. doi: 10.1177/0300060520 967609.
- Aoun NY, Velez E, Kenney LA, Trayner EE. Tracheal bronchus. Respir Care 2004; 49(9):1056-8.