The Impact of Ureteral Wall Thickness on Spontaneous Passage and Development of Long-term Ureteral Stricture in Patients with Ureteral Stone
By Ozgur Ekici1, Abdullah Gul2, Salim Zengin2, Caglar Boyaci2, Metin Kilic2Affiliations
doi: 10.29271/jcpsp.2023.01.101ABSTRACT
Objective: To evaluate the association of ureteral wall thickness (UWT) with spontaneous passage (SP) of ureteral stones and formation of ureteral stricture (US) in patients who underwent ureterorenoscopy for ureteral stones.
Study Design: Cohort study.
Place and Duration of Study: Department of Urology, University of Health Sciences, Bursa Yuksek Ihtisas Training and Research Hospital, Turkey, between January 2019 and June 2021.
Methodology: One hundred and sixty-nine patients with ureteral stones were restrospetively reviewed for maximum stone diameter, stone density, degree of hydronephrosis, parenchymal thickness, and UWT measurement from CT images. The patients were divided into two groups; patients who had (group 1) and had not (group 2) undergone SP of ureteral stones. These two groups were compared for stone characteristics and UWT. Ureterorenoscopy was performed on 52 patients who did not experience SP. Data related to the passage of guide wire and radio-opaque material, drainage method, ureteral wall injury and patients who developed US were recorded. Ureterorenoscopy group were divided into two groups of patients who did and did not develop stricture. These two groups were compared for stone characteristics and perioperative findings.
Results: Of the 169 patients, 106 (62,7%) patients spontaneously passed stones. Ureterorenoscopy was performed on 52 patients. US developed in 9 (17%) patients. Maximum stone diameter, density, and antero-posterior (AP) diameter of the renal pelvis and UWT were statistically different between both groups. The degree of hydronephrosis, ureteral wall injury, density, AP diameter of the stones, parenchyma thickness, length of hospital stay, and UWT were found to be significantly increased in the stricture group.
Conclusion: UWT is a simple measurement that can be used to predict SP of ureteral stones. It can also predict the development of US after ureterorenoscopy in long-term.
Key Words: Ureteral calculi, Ureterorenoscopy, Ureteral wall thickness, Ureteral stricture.
INTRODUCTION
European Association of Urology Guidelines recommends medical expulsive therapy for uncomplicated ureteral stones if the patient is suitable for conservative treatment. The group expected most from this treatment method consists of patients with distal ureteral stones larger than 5 mm.1,2 Factors affecting the success of treatment include maximum stone diameter, ureteral density proximal and distal to the stone, degree of hydronephrosis, and hydration status of the patient.3-5
Inflammatory changes occur in the ureteral wall when the stone remains in the same localisation for a longer period. These changes reduce the possibility of SP of the stone. In addition, complication rates may increase as a result of interventions such as extracorporeal shock wave lithotripsy (ESWL) or ureterorenoscopy. In recent years, the idea of estimating the impact degree of the stone has emerged by measuring the UWT in the ureteral segment where the stone is located by non-invasive non-contrast computed tomography (CT). Based on this assumption, studies investigating the relationship between UWT and spontaneous passage of ureteral stone have been published.6 UWT is defined as the maximum wall thickness of the ureteral segment where the stone is located in the axial section.7
In impacted ureteral stones, oedema and inflammation of the ureteral wall are expected which may lead to bleeding, perforation or failure of procedures such as ureterorenoscopy, ESWL and insertion of Double j stent (DJS).8,9 They may also lead to the development of US in the long-term. Based on this idea, studies investigating the relationship between UWT and complications of ureterorenoscopy have also been published.7,10 However, there is no study in the literature investigating the relationship between UWT and US developed in the long-term.
In this study, the aim was to investigate whether UWT was associated with both SP and potential development US after ureterorenoscopy in the long-term.
METHODOLOGY
After obtaining the ethics committee approval of the University of Health Sciences, Bursa Yüksek İhtisas Training and Research Hospital with reference number 2011-KAEK 25 2021/09-10, the data of patients who presented to the emergency department with renal colic between January 2019 and June 2021 were retrospectively reviewed. In this patient group, patients with 5-10 mm solitary ureteral stones who received daily doses of 0.4 mg tamsulosin as medical expulsive therapy were included in the study. Patients having kidney stones, bilateral and multiple ureteral stones, those with a previous history of ureterorenoscopy, congenital urinary system anomalies, cases requiring emergency drainage, and patients who could not receive medical expulsive therapy were excluded from the study. Gender, age, and medical treatments of the patients were recorded. Maximum stone diameter (mm), stone laterality (right/left), localisation (distal-mid-proximal), and density of the stone in Hounsfield unit (HU) value, degree of hydronephrosis (grade 0- 4),11 antero-posterior diameter of the renal pelvis (mm), renal parenchymal thickness (mm) and UWT (mm) estimated from the non-contrast CT images taken at the time of admission of all patients were recorded. UWT was measured by a single urologist as the maximum UWT in the axial section on CT (Figure 1). SP of the stones was evaluated one month later based on the assessments of radiography for opaque and non-contrast abdominal CT for non-opaque stones. The patients were divided into two groups based on whether SP of the stones had (group 1: SP ; n:106) and had not occurred (group 2: non – SP; n:63). The difference between the recorded data of both groups was evaluated.
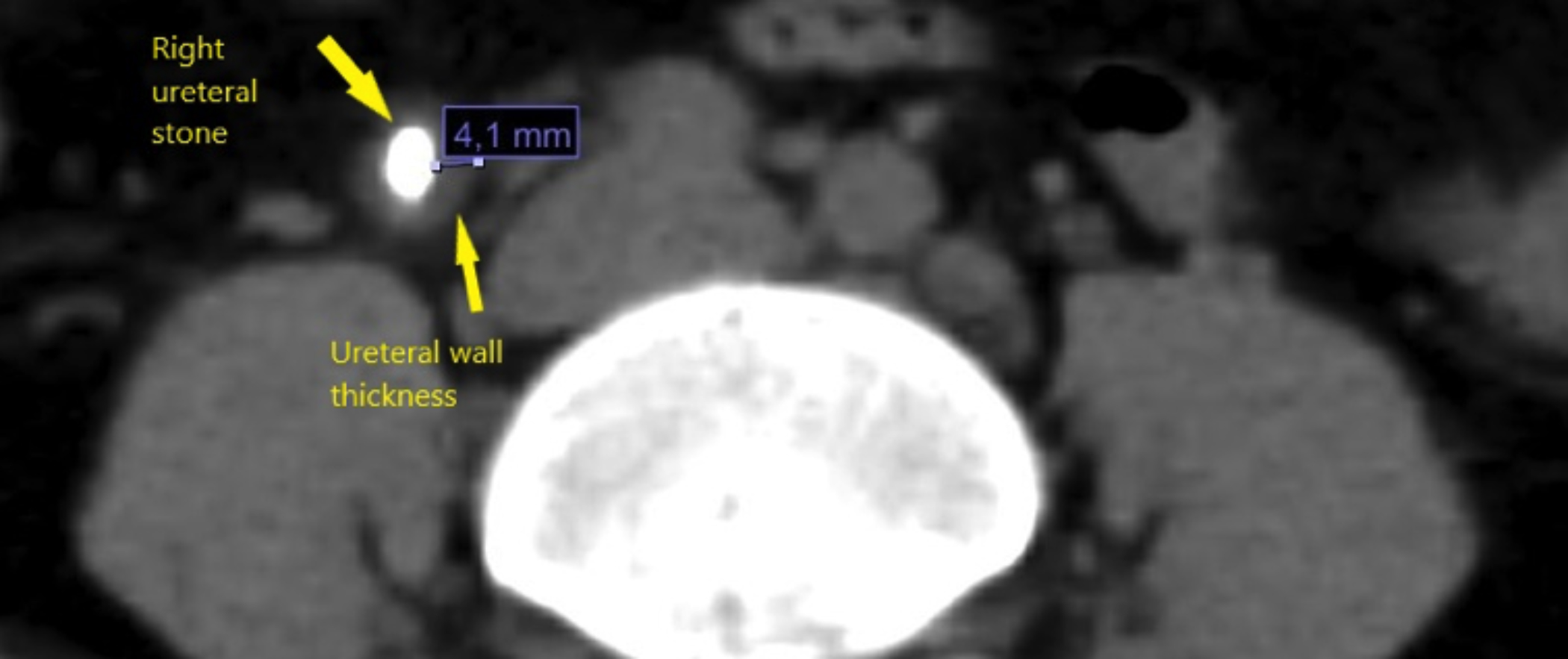 Figure 1: Non-contrast CT image of right ureteral stone and UWT.
Figure 1: Non-contrast CT image of right ureteral stone and UWT.
Procedures (ESWL- ureterorenoscopy) performed on patients, whose stones had not passed spontaneously, were reviewed retrospectively. All ureterorenoscopy procedures were performed using 8/9.5 Fr semi-rigid ureterorenoscopy and Holmium-YAG laser. Data about the passage of guide wire and opaque material proximal to the stone and the degree of ureteral wall injury were retrieved from the operation notes of the patient group who underwent ureterorenoscopy procedures. Data related to the passage of the guide wire and the opaque material were recorded at the beginning of surgery by the surgeon, before lithotripsy. A standard 0.035 inch hydrophilic guide was used in all cases. Before fragmentation the stone, it was recorded whether the guide and the opaque passed proximal to the stone. For the development of US, the data of the patients whose progressive ureteral dilatation continued in the control ultrasonography were analysed. US was diagnosed by CT urography, diagnostic ureterorenoscopy or scintigraphy. Stricture was diagnosed at 1 and 6 months after stent removal. Ureteral wall injury was graded as grade 0 at no evidence of mucosal damage, grade 1 included only mucosal erosion, grade 2 was injury to the mucosa and muscle tissue (periureteral adipose tissue is intact), grade 3 was an adventitial injury, and grade 4 was total ureteral avulsion.12 The surgeon graded ureteral wall injury according to the condition of the ureteral wall at the end of the operation. In addition, the length of hospital stay was also recorded.
Postoperatively, DJS was inserted in all patients and removed after 3 weeks as a routine procedure. In the ureterorenoscopy group, the patients were divided into two groups as those with and without US. The difference in per-operative and post-operative parameters between these two groups was analysed.
Statistical analysis was performed using IBM SPSS version 21 (IBM Corp., Armonk, NY, USA). Shapiro Wilk test was used to examine the normality of the distribution. Continuous variables with normal and non-normal distribution were compared between two groups using student's independent t-test and Mann-Whitney U-test, respectively. Continuous variables were expressed as mean and standard deviation or median and interquartile range based on the used statistical method used, respectively. Categorical variables were expressed as numerical values and percentages. Chi-square and Fisher’s Exact tests were used to compare non-parametric data. Correlation analysis was performed using the Spearman rho correlation analysis method. Two-tailed p <0.05 was considered statistically significant.
RESULTS
A total of 169 patients were included in the study. The median (IQR) age of the patients was 43(33-57) years. The female/male ratio was 46/123. The median (IQR) values for stone size and UWT were 5.9(5.5-7) mm and 3.5(2.27-4.76) mm, respectively. The baseline data are presented in Table I. While 106 patients spontaneously passed their stone, 63 patients did not. ESWL was performed on 5 of these 63 patients, DJS was inserted in 5 patients, and 1 patient was operated on in another hospital. In the remaining 52 patients, ureterorenoscopy was performed in this clinic and ureteroscopic laser lithotripsy was performed. US developed in 9 (17%) patients out of 52 patients who underwent ureterorenoscopy. Of these 9 patients, 5 patients were diagnosed with CT urography, diagnostic ureterorenoscopy and retrograde pyelography, and 4 patients were diagnosed with scintigraphy.
Table I: Analysis of parameters affecting spontaneous passage of stones.|
Variables |
Spontaneous passage (n=106) |
Non-Spontaneous passage (n=63) |
p-values |
|
Age (median (IQR)) |
46.5(34-58) |
41(32-57) |
0.533 |
|
Gender n(%) Male Female |
72 (67.92%) 34 (32.07%) |
51 (80.95%) 12 (19.04%) |
0.066 |
|
Stone laterality n(%) Right Left |
50 (47.16%) 56 (52.83%) |
34 (53.96%) 29 (46.03%) |
0.393 |
|
Degree of hydronephrosis n(%) G0 G1 G2 G3 G4 |
7 (6.60%) 19 (17.92%) 53 (50%) 20 (18.88%) 7 (6.60%) |
0 (0%) 11 (17.46%) 26 (41.26%) 19 (30.15%) 7 (11.11%) |
0.085 |
|
Stone localization n(%) Lower Middle Upper |
53 (50%) 33 (31.13%) 20 (18.86%) |
14 (22.22%) 18 (28.57%) 31 (49.20%) |
<0.001 |
|
Maximum stone diameter (mm) (median (IQR)) |
5.69(5.35-6.28) |
6.9 (5.87-8.37) |
<0.001 |
|
Stone density (HU) (median (IQR)) |
330(219-510) |
600 (469-802) |
<0.001 |
|
AP Diameter (mm) (median (IQR)) |
18(14-22) |
19 (17-29) |
0.017 |
|
UWT (mm) (median (IQR)) |
2.79(2-4.1) |
4.71 (3.69-5.93) |
<0.001 |
|
Parenchymal thickness (mm) (median (IQR)) |
19(16-22) |
19 (16.4-22) |
0.864 |
|
Continuous variables were compared by Mann-Whitney U-test. Categorical variables were analysed by Chi-square and Fisher Exact Test for comparision of differences between 2 groups. |
|||
Table II: Parameters associated with the development of stricture.
|
Variables (n=52) |
Non- stricture group (n=43) |
Stricture group (n=9) |
p-value |
|
Age (mean± SD) |
41.72± 15.56 |
46 ± 11.76 |
0.441 |
|
Gender n (%) Male Female |
34 (79.06%) 9 (20.93%) |
8 (88.88%) 1 (11.11%) |
0.497 |
|
Stone Laterality n (%) Right Left |
25 (58.13%) 18 (41.86%) |
3 (33.33%) 6 (66.66%) |
0.175 |
|
Degree of hydronephrosis n (%) G0 G1 G2 G3 G4 |
0 (0%) 10 (23.25%) 20 (46.51%) 10 (23.25%) 3 (6.97%) |
0 (0%) 1 (11.11%) 1 (11.11%) 3 (33.33%) 4 (44.44%) |
0.011 |
|
Stone localisation n (%) Lower Middle Upper |
11 (25.58%) 9 (20.93%) 23 (53.48%) |
1 (11.11%) 6 (66.66%) 2 (22.22%) |
0.024 |
|
Ureteral wall injury n (%) G0 G1 G2 G3 G4 |
14 (32.55%) 11 (25.58%) 10 (23.25%) 8 (18.60%) 0 (0%) |
0 (0%) 1(11,12%) 4(44,44%) 4(44.44%) 0(0%) |
0.070 |
|
Guide passage n (%) Passed Not-passed |
31 (72.09%) 12 (27.90%) |
1 (11.11%) 8 (88.88%) |
0.001 |
|
Opaque passage n (%) Passes Not-passed |
33 (76.74%) 10 (23.25%) |
2 (22.22%) 7 (77.77%) |
0.003 |
|
Maximum stone diameter (mm) (median (IQR)) |
6.7(5.7-8.2) |
7.8(6.6-9.1) |
0.119 |
|
Stone density (HU) (mean ± SD) |
632.07 ± 291.29 |
887.22 ± 190.52 |
0.015 |
|
AP Diameter (mm) (mean ± SD) |
20.10 ± 7.19 |
26.88 ± 9.26 |
0.018 |
|
UWT (mm) (mean ± SD) |
4.35± 1.33 |
6.55± 0.37 |
<0.001 |
|
Parenchymal thickness (mm) (mean ± SD) |
19.49± 4.28 |
15.63 ± 3.94 |
0.016 |
|
Lenght of hospital stay (day) (median (IQR)) |
1(1-2) |
3(1-4) |
0.020 |
|
Continuous variables were compared by Student t-test and Mann-Whitney U-test according to normally distributed or undistributed, respectively. Categorical variables were analysed by Chi-square and Fisher Exact Test for comparision of differences between 2 groups. |
|||
There was no statistically significant difference between the SP and non-SP groups in terms of age, gender, stone laterality, degree of hydronephrosis, and parenchyma thickness. Localisation, size, density, antero-posterior diameter, and UWT were found to be statistically significantly associated with SP (p <0.001, <0.001, <0.001, 0.013, and <0.001, respectively, Table I).
In the correlation analysis of the parameters related to SP, there was a weak and significant correlation between SP and stone localisation (upper-middle-lower) and AP diameter (r coefficients and p values +0.336 p:0.001, and -0.185 p:0.016 respectively), while a weak-moderate correlation was found between SP and stone size, stone density and UWT (r coefficients and p values = 0.440 p:0.001, and -0.445 p:0.001, -0.471 p:0.001 respectively, Table III).
Table III: Correlation analysis of the parameters associated with spontaneous passage of the ureteral stone.
|
Parameters |
Spearman r |
p-value |
|
Stone localisation (upper-middle-lower ureteral segments)* |
0.336 |
0.001 |
|
Maximum stone diaeter (mm) |
-0.440 |
0.01 |
|
Stone density (HU) |
-0.445 |
0.001 |
|
AP diameter (mm) |
-0.185 |
0.016 |
|
UWT (mm) |
-0.471 |
0.001 |
|
* SP increases as the stone localisation descends to the lower ureter. |
||
Table IV: Correlation analysis of the parameters associated with ureteral stricture secondary to endoscopic surgical treatment of the ureteral stones.
|
Parameters |
Spearman r |
p-value |
|
Degree of hydronephrosis |
+0.365 |
0.008 |
|
Passage of guide wire* |
+ 0.474 |
0.001 |
|
Passage of opaque material |
+ 0.440 |
0.01 |
|
Stone density |
+ 0.381 |
0.006 |
|
AP iameter |
+ 0.300 |
0.031 |
|
UWT |
+ 0.635 |
0.001 |
|
Parenchymal thickness ** |
-0.331 |
0.016 |
|
* There is a positive significant correlation between the failed guide wire passage and the development of a stricture. ** There is a negative correlation between parenchymal thickness and development of a stricture. |
||
In the ureterorenoscopy group, 14 (26.9%) patients did not develop ureteral wall injury, while the remaining patients had G1 (n:12; 23.1%), G2 (n:14; 26.9%), and G3 (n:12; 23.1%) ureteral wall injuries. G4 injury did not develop in any of the patients. At the beginning of the operation, guide wire could not be advanced in 20 (38.4%) and passage of opaque material could not occur in 17 (32.6%) patients. Factors associated with the development of US were analysed in 52 patients who underwent ureterorenoscopy and endoscopic lithotripsy. According to this analysis, the degree of hydronephrosis, stone localisation, passage of the guide passage and opaque material, stone density, parenchyma thickness, length of hospital stay, and UWT were found to be statistically significantly associated with the development of stricture (Table II).
In the correlation analysis parenchyma thickness, stone density, AP diameter, and degree of hydronephrosis demonstrated weakly significant (respective r coefficients and p values = 0.331 p:0.016; +0.381 p:0.006; +0.300 p:0.031; and + 0.365 p:0.008), passage of the guide and opaque material revealed weakly-moderately significant (respective r coefficients and p values = +0.474 p:0.001; and +0.440 p:0.01), and UWT exhibited moderately significantly correlations (r coefficient and p-value+0.635 p:0.001) with the development of stricture after ureterorenoscopy (Table IV).
DISCUSSION
Oedema and fibrosis formed in the ureteral segment where the ureteral stone is localised are observed as an increase in periureteral thickness in CT images. This observation suggests to clinicians that the stone may be impacted with lower probability of SP. Studies supporting this hypothesis have been published in the literature.6,13 In addition, US may develop in impacted stones after development of oedema and the sequelae formed subsequent to the healing of micro-level damage caused by ureterorenoscopy. The results of this study support that UWT affects SP, but also provide new information to the literature by showing that increased UWT enhances the risk of US after ureterorenoscopy.
Studies investigating the effect of UWT on SP have been published recently. According to multivariate analysis, Yoshida et al. reported that stone size, stone localisation, and UWT were independent predictors of SP of a Stone impacted for 4-weeks after ureterorenoscopy.6 In their study, Kachroo et al. determined the maximum UWT as the most important predictor of SP.13 In their study, 212 patients subjected to multivariate analysis, Samir et al. showed that only UWT and degree of hydronephrosis were statistically significant predictors of SP in the patient group with 5-10 mm stones treated with silodosin.14
The impact of UWT on perioperative parameters in the patient group that underwent ureterorenoscopy has also been the subject of research. In a study investigating the relationship between the UWT and the DJS insertion, Sarica et al. concluded that UWT was increased in the group in which DJS did not pass.10 Sarica et al. indicated stone-free rates of 88.6%, and 63.2% one week after ureterorenoscopy in the groups with UWT < 5 mm and > 5 mm, respectively. In addition, the group with a UWT greater than 5 mm required DJS at a statistically significant higher rate (p= 0.025).15 In their publication, Yoshida et al. determined UWT as an independent predictor of the stone impaction based on ureterorenoscopy findings.7
The development of US during the follow-up period after ureterorenoscopy may lead to a silent obstruction if an effective follow-up process is not performed. Renal functions may be affected as a result of obstruction. The most important risk factor in the development of stricture is impaction of the stone.16 Other factors are related to the use of ureteral access sheath use, lithotripter, diameter of ureterorenoscopy, stone size, and surgeon's experience.17 During endoscopic intervention to the impacted stone, oedema and cystic changes developed in the working area restrict the surgical field. These changes cause micro-level perforations during lithotripsy. Fibrosis that will develop while these perforations are being repaired will lead to the development of stricture in the future. Perhaps it is necessary to extend the scope of the follow-up program in order to discern the development of stricture after endoscopic treatment of an impacted stone. Even in an asymptomatic patient, the developing scricture can silently impair kidney function.18 The development of US after ureterorenoscopy has been reported at different rates in the literature. Roberts et al. indicated that 24% of US may develop in impacted stones that have been present for more than 2 months.19 In the study of Geçit et al, which included 612 patients, US was detected in 8 (1.3%) patients.20 In this study, the rate of US was determined as 17 percent. The reasons for the differences in the incidence rates of US may be related to the size of the ureterorenoscopy used, the energy characteristics of the lithotripter, and the differences in the amount and characteristics of residual stone fragments.
In another study, the relationship of ureteral stone HU with SP and ureteral stricture has been demonstrated. Tran et al. did not observe a statistically significant difference in terms of HU between the impacted stone group and the control group, and they notices that the HU in the distal of the stone was significantly higher in the impacted group.3 Pareek et al. concluded that stone HU can predict the stone-free rate after ESWL.21 Sahin et al., investigated the patients with distal ureteral stones that received medical expulsive therapy and reported that the mean HU was statistically significantly lower in the group that could spontaneously pass their stones compared to the group that could not.22 The relationship between HU of the stone and the development of stricture can be explained by the increase in laser energy and time applied to the stone as the HU of the stone increases. In their study, Rana et al., found a positive correlation between the HU of the stone and the total laser energy applied and total duration of laser therapy.23
Other factors affecting the SP of ureteral stones have been investigated in the literature. In a study on 392 patients, Jendeberg et al. reported that only the size and location of the stone affected the rate of SP.24 Zorba et al. reported that not only the diameter of the stone in the axial or coronal section but also the volume of the stone significantly affects the SP.25 Yamashita et al. investigated the effect of UWT and ureteral wall volume on SP in ESWL patients. According to multivariate analysis, only ureteral wall volume was associated with ESWL failure.9 Being able to predict the SP of a ureteral stones can help surgeons in their decision-making process. First, earlier intervention may be offered to patients with a low probability of SP. Thus, nephron damage caused by obstructed stones can be prevented. Secondly, patients with increased UWT can be investigated in more detail before surgery in terms of ureteral wall injury and perforation, possibility of open surgical repair, and insertion of a nephrostomy tube. In short, the patient group with increased UWT should not be considered as a simple ureterorenoscopy patient. It is important to be prepared for complications that may develop in these patients.
The present study shows that increased UWT negatively affects SP and is associated with US in the long-term. However, there are also limitations of the study. First, this study population consisted of a small number of patient groups and the data were analysed using a retrospective method. Second, since the duration of the obstruction caused by the stone was not known at the time of diagnosis, data related to the longevity of obstruction before establishment of diagnosis were not included in the analysis. Prolonged impaction of the stones might be expected to be associated with fewer SP of stones and the greater number of US. Third, operative and laser usage times were not included in the analysis. Longer use of laser may also affect stricture rates. There is a need for prospective studies investigating the relationship of UWT with US in patients groups followed up for longer periods of time.
CONCLUSION
UWT can be used both to predict SP of ureteral stone and the probability of US development after ureterorenoscopy. Early intervention is suggested to the patient with ureteral stones by measuring UWT which can also be helpful in informing the patient about the risk of US that may develop inc the patients who will be operated on.
ETHICAL APPROVAL:
The study was approved by the Ethics Committee of the University of Health Sciences Bursa Yüksek İhtisas Training and Research Hospital with reference number 2011-KAEK 25 2021/09-10.
PATIENTS’ CONSENT:
Written informed consent were taken from all the patients.
COMPETING INTEREST:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no competing interest to declare that is relevant to the content of this article.
AUTHORS’ CONTRIBUTION:
OE: Study conception and design, analysis and interpretation data, and manuscript.
AG: Study conception, design, and manuscript writing.
SZ: Acquisition of data, and critical revision.
CB: Critical revision, analysis, and data interpretation.
MK: Critical revision and manuscript writing.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Turk C, Knoll T, Seitz C, Skolarikos A, Chapple C, McClinton S, et al. Medical expulsive therapy for ureterolithiasis: the EAU recommendations in 2016. Eur Urol 2017; 71(4): 504-7. doi: 10.1016/j.eururo.2016.07.024.
- Urkmez A, Tokuc E, Topaktas R, Sahin A, Yuksel OH. Mirabegron: A novel and promising medical expulsive treatment for ureteral stones? J Coll Physicians Surg Pak 2019; 29(01):73-4. doi: 10.29271/jcpsp.2019.01.73.
- Tran TY, Bamberger JN, Blum KA, Parkhomenko E, Thai J, Chandhoke RA, et al. Predicting the impacted ureteral stone with computed tomography. Urology 2019; 130:43-7. doi: 10.1016/j.urology.2019.04.020.
- Arshad S, Mahmood K, Khalique A. Significance of hounsfıeld units on non-contrast computed tomography ın determınıng stone free rate after eswl. PJR 2018; 28(2).
- Khaliq DM, Faıq SM, Jesranı AK. Effect of ct scan hounsfıeld unıts (attenuatıon value of stones) ın predıctıng outcomes of eswl ın renal calculi, experıence at sıut. PJR 2021; 31(3).
- Yoshida T, Inoue T, Taguchi M, Omura N, Kinoshita H, Matsuda T. Ureteral wall thickness as a significant factor in predicting spontaneous passage of ureteral stones of≤ 10 mm: A preliminary report. World J Urol 2019; 37(5):913-9. doi: 10.1007/s00345-018-2461-x.
- Yoshida T, Inoue T, Omura N, Okada S, Hamamoto S, Kinoshita H, et al. Ureteral wall thickness as a preoperative indicator of impacted stones in patients with ureteral stones undergoing ureteroscopic lithotripsy. Urology 2017; 106:45-9. doi: 10.1016/j.urology.2017.04.047.
- Bulbul E, Ilki FY, Gultekin MH, Erozenci A, Tutar O, Citgez S, et al. Ureteral wall thickness is an independent parameter affecting the success of extracorporeal shock wave lithotripsy treatment in ureteral stones above the iliac crest. Int J Clin Pract 2021; 75(7):e14264. doi: 10.1111/ijcp.14264
- Yamashita S, Kohjimoto Y, Iguchi T, Nishizawa S, Kikkawa K, Hara I. Ureteral wall volume at ureteral stone site is a critical predictor for shock wave lithotripsy outcomes: Comparison with ureteral wall thickness and area. Urolithiasis 2020; 48(4):361-8. doi: 10.1007/s00240-019- 01154-w.
- Sarica K, Eryildirim B, Akdere H, Karagoz MA, Karaca Y, Sahan A. Predictive value of ureteral wall thickness (UWT) assessment on the success of internal ureteral stent insertion in cases with obstructing ureteral calculi. Urolithiasis 2021; 49(4):395-65. doi: 10.1007/s00240-020- 01233-3.
- Fernbach S, Maizels M, Conway J. Ultrasound grading of hydronephrosis: Introduction to the system used by the society for fetal urology. Pediatr Radiol 1993; 23(6): 478-80. doi: 10.1007/BF02012459.
- Traxer O, Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal Surgery J Urol 2013; 189(2):580-4. doi: 10. 1016/j.juro.2012.08.197.
- Kachroo N, Jain R, Maskal S, Alshara L, Armanyous S, Milk J, et al. Can CT-based stone ımpaction markers augment the predictive ability of spontaneous stone passage? J Endourol 2021; 35(4):429-35. doi: 10.1089/end.2020.0645.
- Samir M, Elawady H, Hamid E, Tawfick A. Can ureteral wall thickness (UWT) be used as a potential parameter for decision-making in uncomplicated distal ureteral stones 5–10 mm in size? A prospective study. World J Urol 2021; 39(9):3555-61. doi: 10.1007/s00345-021-03608-6.
- Sarica K, Eryildirim B, Akdere H, Camur E, Sabuncu K, Elibol O. Could ureteral wall thickness have an impact on the operative and postoperative parameters in ureteroscopic management of proximal ureteral stones? Actas Urol Esp (English Edition) 2019; 43(9):474-9. doi: 10.1016/j.acuroe. 2018.10.007.
- Darwish AE, Gadelmoula MM, Abdelkawi IF, Abdellatif AM, Abdel-Moneim AM, Hammouda HM. Ureteral stricture after ureteroscopy for stones: A prospective study for the incidence and risk factors. Urol Ann 2019; 11(3):276. doi: 10.4103/UA.UA_110_18.
- Dong H, Peng Y, Li L, Gao X. Prevention strategies for ureteral stricture following ureteroscopic lithotripsy. Asian J Urol 2018; 5(2):94-100. doi: 10.1016/j.ajur.2017.09.002.
- Hernandez N, Mozafarpour S, Song Y, Eisner BH. Cessation of ureteral colic does not necessarily mean that a ureteral stone has been expelled. J Urol 2018; 199(4):1011-4. doi: 10.1016/j.juro.2017.10.032.
- Roberts WW, Cadeddu JA, Micali S, Kavoussi LR, Moore RG. Ureteral stricture formation after removal of impacted calculi. J Urol 1998; 159(3):723-6. doi: 10.1016/S0022- 5347(01)63711-X.
- Gecit I, Pirincci N, Taken K, Benli E, Ceylan K. Application of ureteroscopic pneumatic lithortripsy in patients with ureter calculi: Our five years experience. Pak J Med Sci 2012; 28(1).
- Pareek G, Armenakas NA, Fracchia JA. Hounsfield units on computerised tomography predict stone-free rates after extracorporeal shock wave lithotripsy. J Urol 2003; 169(5):1679-81. doi: 10.1097/01.ju.0000055608.92069.3a.
- Sahin MO, Sen V, Irer B, Ongun S, Yildiz G. Can the Hounsfield unit predict the success of medical expulsive therapy using silodosin in 4‐to 10‐mm distal ureteral stones? Int J Clin Pract 2021; 75(4):e13844. doi: 10. 1111/ijcp.13844.
- Rana RS, Ather MH. Hounsfield units-a significant predictor of lasering time and energy in the management of upper urinary tract stones using Holmium: Yttrium–Aluminum Garnet lasers. Int Urol Nephrol 2020; 52(9):1637-41. doi: 10.1007/s11255-020-02442-w.
- Jendeberg J, Geijer H, Alshamari M, Cierzniak B, Lidén M. Size matters: The width and location of a ureteral stone accurately predict the chance of spontaneous passage. Eur Radiol 2017; 27(11):4775-85. doi: 10.1007/s00330-017- 4852-6.
- Zorba OU, Ogullar S, Yazar S, Akca G. CT-based determination of ureteral stone volume: A predictor of spontaneous passage. J Endourol 2016; 30(1):32-6. doi: 10.1089/end. 2015.0481.