Takayasu Arteritis with Isolated Headache and Neck Pain
By Nazia Arain1, Shamsuddin Shaikh1, Jawad Ali2Affiliations
doi: 10.29271/jcpsp.2022.12.1617ABSTRACT
Takayasu Arteritis (TA), a chronic inflammatory condition of the aorta and its major branches, causes narrowing and ultimate occlusion of major vessels and may manifest as cerebrovascular insufficiency, organ ischemia, and systemic arterial hypertension (HTN). Herein, we report a case of a 35-year female with the pulseless disease but no other clinical signs except headache and neck pain on exertion despite the fact that three out of four vessels of the aortic arch were occluded. Diagnosis of TA was based on clinical findings, radiological imaging, and doppler studies. This case report highlights the clinical importance of unexplained headaches and absent peripheral pulses in the screening of TA.
Key Words: Takayasu arteritis, Unexplained headache, Neck pain.
INTRODUCTION
Takayasu Arteritis (TA) is a rare, idiopathic, vasculitis of large vessels, mainly involving the aorta and its main branches, leading to narrowing, stenosis, and aneurysmal dilatation of vessels.1 It predominantly affects young women, especially in the second and third decades, and is more prevalent among Asians.2 The worldwide incidence of TA is estimated at 2.6 cases/million/year.3 It has a heterogeneous clinical presentation due to vascular changes or ischemia of different organs or limbs, carotodynia, limb claudication, absent peripheral pulses, bruits, myocardial infarction, systemic arterial hypertension, headache, visual disturbance, and ischemic strokes.4 TA is associated with significant morbidity and mortality. About 20% of patients have self-limited disease, whereas 80% may progress to relapsing/remitting disease and need immunosuppressive treatment. Approximately 90% of patients with TA have survival rate of 10-years; this rate is reduced in the presence of major complications.5 Early diagnosis and treatment is vital for a better outcome. Herein, we present a case of a 35-year female with the pulseless phase of TA who presented with headache and neck pain.
CASE REPORT
A 35-year female presented with episodes of headache and neck pain for 6 months, more marked on exertion and physical activity.
There was no history of loss of consciousness, weakness, visual disturbances, fever, malaise, joint pains, and limb claudication. General physical examination revealed absent radial, brachial and carotid pulses on both sides, with normal palpable pulses in lower limbs. Blood pressure in both upper extremities was unrecordable, while it was 140/90 mmHg in lower limbs. Vascular bruit was audible over the right carotid area. The remaining cardiovascular, neuromuscular, respiratory, and abdominal examination was unremarkable. Risk factors of atherosclerosis like diabetes mellitus, smoking, dyslipidemia, and family history of vascular events were also assessed and excluded. The erythrocyte sedimentation rate was raised (35 mm/1st hr) and C-reactive protein was normal (0.05 mg/L). Complete blood count, renal function tests, blood sugar, fasting lipid profile, computed tomography (CT) scan of the brain, electrocardiography, echocardiography, and chest x-ray were normal.
Doppler ultrasound of carotids showed diffuse circumferential and mural thickening involving both the right and left common carotid arteries (Figure 1), causing severe luminal narrowing with sluggish flow on doppler. Multiple collateral vessels were noted on both sides of the neck. Subclavian arteries were not visualised. Magnetic resonance angiography (MRA) brain showed retrograde filling of anterior and middle cerebral artery through posterior circulation (Figure 2).
CT Angiogram (CTA) of the thoracic aorta showed mild mural thickening of the arch of aorta and ascending and descending the thoracic aorta. There was severe narrowing with complete obliteration of the left subclavian artery at its origin. Moderate to severe narrowing and filling defects were noted proximal to the origin of left common carotid artery, as were also narrowing and filling defects in the brachiocephalic trunk just proximal to its bifurcation, and the right common carotid artery (Figure 3). The coronary, abdominal and renal angiograms were normal.
With all above findings, the patient was diagnosed as a case of TA, type 2b. The patient was managed with a high dose of oral steroids, prednisolone 1 mg/kg in divided doses. The patient responded well. Headache and neck pain were improved and acute phase reactants returned to their normal limits. The patient started feeling better with start of routine activities.
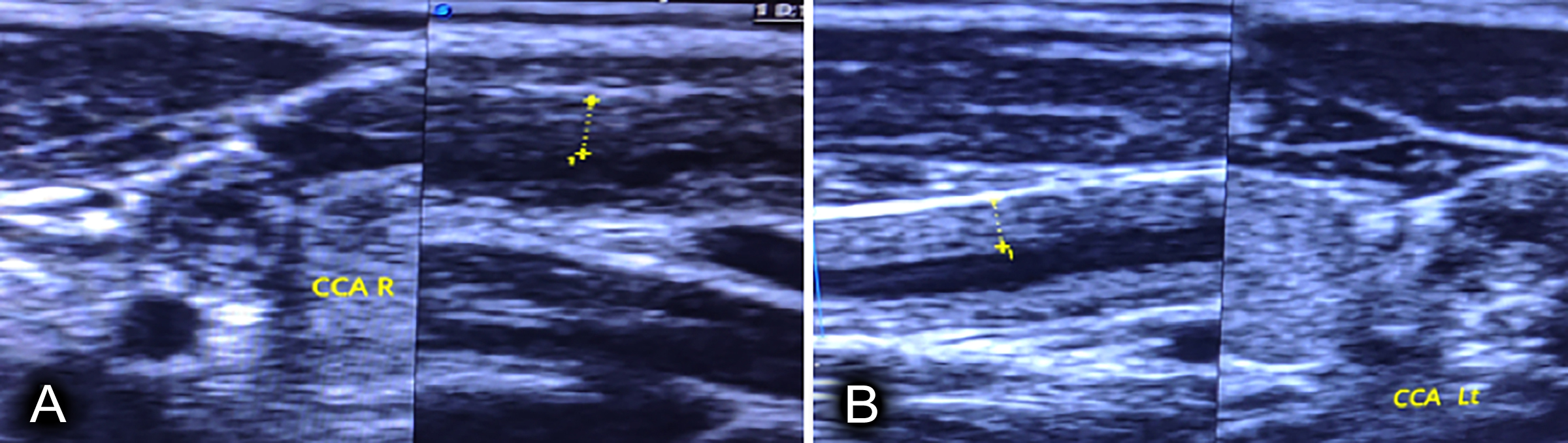 Figure 1: Doppler ultrasound (A) Diffuse mural thickening of RCCA (B) Diffuse mural thickening of LCCA.
Figure 1: Doppler ultrasound (A) Diffuse mural thickening of RCCA (B) Diffuse mural thickening of LCCA.
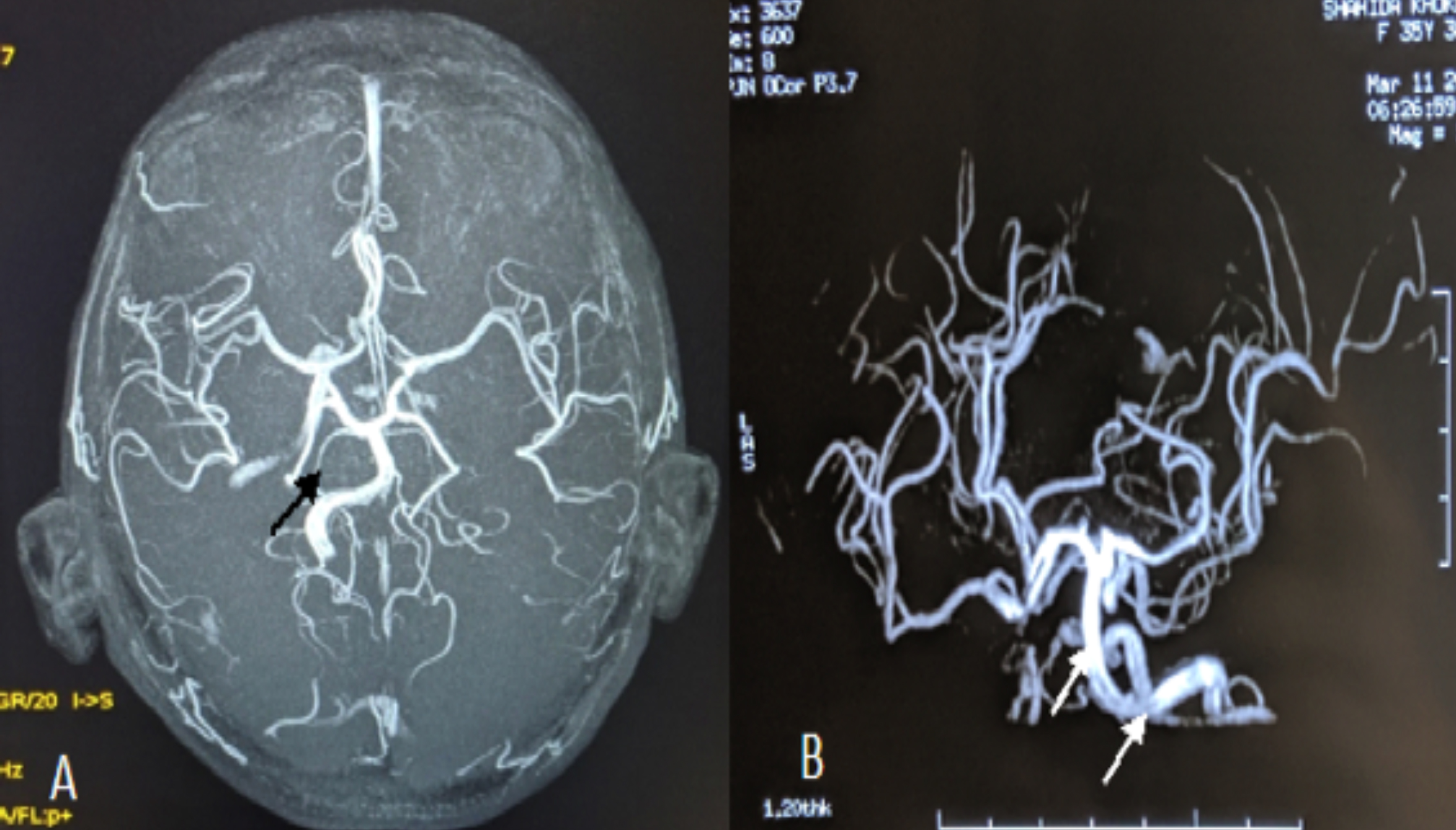 Figure 2 (A,B): MRA brain: Arrow shows retrograde filling of anterior and middle cerebral artery through posterior.
Figure 2 (A,B): MRA brain: Arrow shows retrograde filling of anterior and middle cerebral artery through posterior.
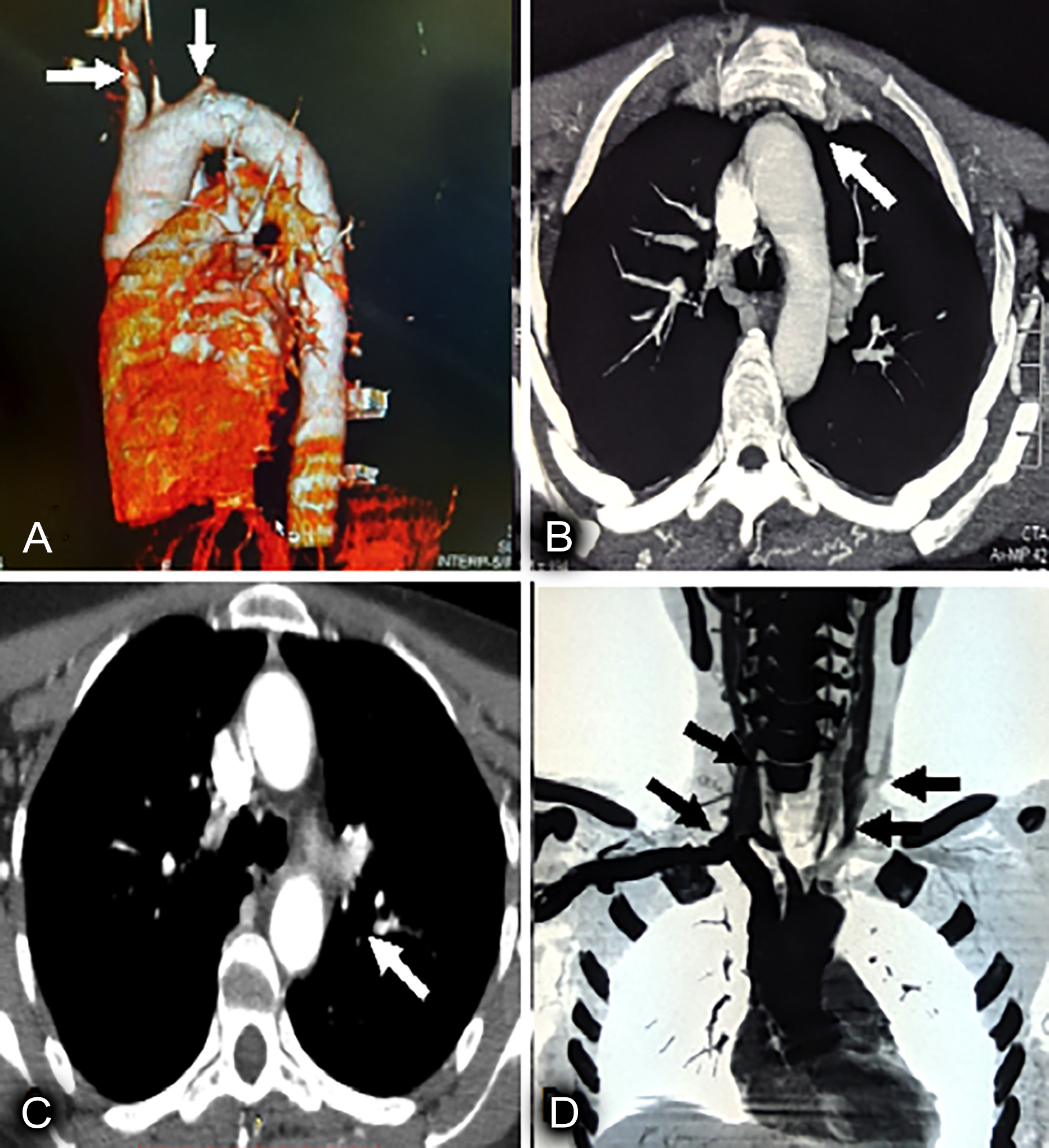 Figure 3: CT angiogram of thoracic aorta: (A) Mural thickening of arch of aorta (B) Ascending (C) Descending thoracic aorta (D) Left arrow shows severe narrowing and filling defect in subclavian, and LCCA at its origin, rt arrow shows narrowing of brachiocephatlic trunk and its bifurfaction also narrowing and filling defect in RCCA.
Figure 3: CT angiogram of thoracic aorta: (A) Mural thickening of arch of aorta (B) Ascending (C) Descending thoracic aorta (D) Left arrow shows severe narrowing and filling defect in subclavian, and LCCA at its origin, rt arrow shows narrowing of brachiocephatlic trunk and its bifurfaction also narrowing and filling defect in RCCA.
DISCUSSION
TA has a worldwide distribution, with the greatest prevalence among Asian women of child-bearing age.6 The American College of Rheumatology criteria are used to classify TA, which include: (1) Age <40 years (2) Limb claudication (3) Decrease in brachial artery pulses in one or both arms (4) Blood pressure difference in both arms >10 mmHg (5) Presence of vascular bruit over the aorta or subclavian arteries, and (6) Angiographic evidence of narrowing and occlusion of the entire aorta or its major branches. It requires three out of six criteria and is 97.8% specific.4,7 This patient met five out of six criteria. Approximately 10% of patients with TA are asymptomatic, and the diagnosis is only suggested by abnormal vascular findings on examinations. The course of the disease is divided into early inflammatory phase with non-specific signs and symptoms of fever, arthralgia, malaise, night sweats, anorexia, and weight loss. Due to non-specific symptoms, the disease is often unrecognised in this phase, and the late chronic phase results in narrowing and occlusion of vessels, ischemia of organs, vascular tenderness, bruit, and aneurysmal dilatation. This patient presented with headache and neck pain and physical examination revealed pulse and blood pressure discrepancies in the upper and lower extremities. Cerebrovascular involvement has been reported in as many as 24% cases of aortoarteritis with occlusion, stenosis, aneurysm, and arterial thickening seen mostly in extracranial carotids and vertebral circulation. Furthermore, the literature review has shown that colour doppler studies and angiography are highly useful for detecting disease severity; 4,7,8 however, due to patient preference non-invasive findings of carotid doppler and CT angiogram were sufficient for diagnosis and classification of TA.
Adequate therapy in TA is important to prevent further progression and complications. Corticosteroids are still the mainstay of treatment. In addition, other immunosuppressive agents such as methotrexate, azathioprine, and cyclophosphamide are used in steroid-refractory cases.9 Symptoms of TA are dramatically improved with anti-inflammatory therapy. Five-year survival in adults is 94%.10 Mortality is related to hypertension, renal involvement, and respiratory and cardiac failure. In the presence of symptomatic stenotic lesions, bypass graft, patch angioplasty, endarterectomy, or stent placement should be considered.4,7 In this patient, even though three out of four major vessels were occluded, the patient was not much symptomatic. Early treatment with a high dose steroids was started. This improved patient’s symptoms and normalised acute phase reactants. During follow-up, this patient may need azathioprine and other immunosuppressives as steroid-sparing alternatives to avoid side effects.
In conclusion, patients with unexplained headache, neck pain, and absent peripheral pulses should be screened for Takayasu arteritis. No laboratory investigation is specific. General physical examination, carotid doppler and CT angiogram are useful for diagnosis. Early diagnosis and treatment are important to improve the outcome.
PATIENT’S CONSENT:
Informed consent has been obtained from the patient and her husband to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
NA: Principal investigation such as introduction, discussion and reference writing.
SUS: Review and revision.
JA: Radiological reporting.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Bond KM, Nasr D, Lehman V, Lanzino G, Cloft HJ, Brinjikji W, Intracranial and extracranial neurovascular manifestations of Takayasu arteritis. AJNR Am J Neuroradiol 2017; 38(4); 766-72. doi: 10.3174/ajnr.A5095.
- Hedna VS, Patel A, Bidari S, Elder M, Hoh BL, Yahnis A, et al. Takayasu’s Arteritis: Is it a reversible disease? Case report and literature review. Surg Neurol Int 2012; 3: 132-10. doi: 10.4103/2152-7806.102947.
- Numano F, Kobayashi Y. Takayasu arterit is beyond pulselessness. Intern Med 1999; 38(3):226-32. doi: 10. 2169/internalmedicine.38.226.
- Lalhmachhuani PC, Daimei SL, Ralte RL. A case of Takayasu arteritis in elderly male patient. Indian J Medical Research Pharmaceutical Sciences 2017; 4(12).
- Phillip R, Luqmani R, Mortality in systemic vasculitis: A systematic review. Clin Exp Rheumatol 2008; 26(5 Suppl 51):S94-104.
- James William D, Berger Timothy G. Andrew’ Diseade of the skin: Clinical dermatology. Saunders Elsevier ISBN 978- 0-7216-2921-6.
- Khan MAM, Banoo H: A case report of takayasu arteritis. Med Today 2012; 24(2):79-81.
- Nazzal MD, Agko M, Zingale K, Hamdan M, Higgins JA, Clark P. A unique presentation of Takayasu arteritis in a 39-year old male with chest pain, vertigo, and blindness. J Vasc Surg 2011; 54(2):529-32. doi: 10.1016/j.jvs.2010.12.059.
- Nascif AK, Lemos MD, Oliveria NS, Perim PC, Corderio AC, Quinintinon M. Takayasu arteritis in children and adolescents; Report of three cases. Rev Bras Reumatol 2011; 51:527-30.
- Hotchi M, Pathological studies on Takayasu arteritis. Heart Vessels 1992; 7:S11-7. doi: 10.1007/BF01744538.