Surgical Blowhole Incision - An Unconventional Approach to Subcutaneous Emphysema Management Following Blunt Neck Trauma
By Tooba Khanum, Mohammad Saad Jawaid, Sadaf Zia, Iqbal A.M. KhyaniAffiliations
doi: 10.29271/jcpsp.2022.05.665ABSTRACT
Subcutaneous emphysema is the fortuitous entry of air into subcutaneous tissue. Its occurrence in the head, neck, and mediastinum is a result of trauma or surgery. This case describes a 45-year male who presented with massive progressive subcutaneous emphysema, spreading from the peri-orbital area to the upper mediastinum, secondary to tracheal injury following blunt trauma sustained two days before presentation. We present this case to emphasize on simple management and observation of minor laryngo-tracheal trauma which can prevent further unexpected complications. In this case, we used an unconventional approach of making blowhole incision which is not in routine practice.
Key Words: Subcutaneous emphysema, Blowhole, Neck trauma.
INTRODUCTION
Subcutaneous emphysema (SE) as a sequela of head, neck, and chest trauma is well documented in the literature. According to Advanced Trauma Life Support (ATLS) protocols, it is identified during the secondary survey.1
Clinical symptoms depend upon the amount of gas and degree of extension. It can be identified clinically as swelling and palpable crepitus of subcutaneous tissue. There may also be dyspnea, chest pain, and dysphagia.2 Progression can be rapid with air build-up at multiple tissue levels causing severe discomfort, airway compromise, cardiac tamponed, and tension pneumomediastinum. Accumulation of air at the level of the thoracic inlet can compress the trachea and great vessels, thereby severely compromising the airway, venous return, and blood flow to the head and neck. Thorough clinical examination must be done whenever possible for prompt diagnosis and recognition of the site of injury.
Plain radiographs can identify the presence of air in the subcutaneous tissue and deep spaces of the neck and mediastinum. However, a CT scan is a better modality when a small amount of accumulated gas is present.3
We present a case of progressive facial and cervical SE and pneumo-mediastinum with compressive symptoms endangering the airway following blunt neck trauma. This case emphasizes the minimalistic approach to the management of such injuries and SE associated with it. The importance of this approach lies in it being conservative for blunt neck trauma and a minimalistic surgical approach for SE.
CASE REPORT
A 45-year male presented in our OPD, four days following accidental strangulation with complaints of the face and neck swelling and hoarseness. Managed initially at primary care centre elsewhere, he was referred to tertiary care setup due to progression of swelling. Vital parameters reveal blood pressure of 130/90 mmHg, pulse, 80/min, respiratory rate, 17 breaths/min, SpO2, 98% on room air with no features of airway compromise.
Clinical evaluation showed strangulation marks, subcutaneous tissue swelling, and crepitus extending from the mandible superiorly, downward to the second intercostal space. Neck circumference was 15 cm. Flexible fibreoptic direct laryngoscopy showed normal-looking glottis with intact mucosa. The rest of the systemic examination was non-contributory as was the past history. Baseline laboratory investigations and ECG were unremarkable. Neck and chest radiographs showed marked subcutaneous emphysema. He was admitted in a monitored setup with the plan of observation and localisation of air leak.
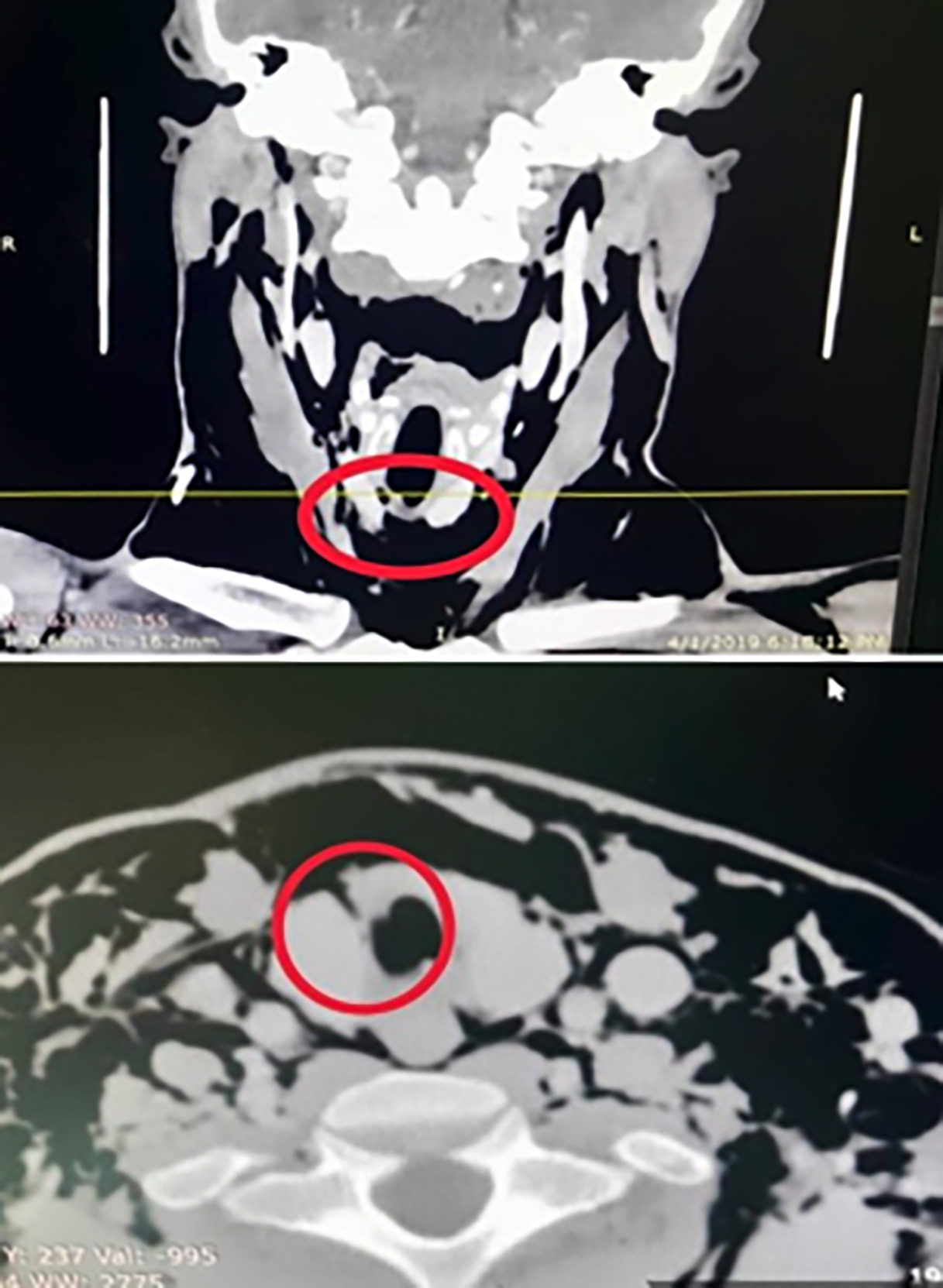 Figure 1: Site of air leak in CT scan of neck with contrast (demarcated with the red circle).
Figure 1: Site of air leak in CT scan of neck with contrast (demarcated with the red circle).
The patient was kept nill per oral (NPO), and broad-spectrum IV antibiotics were started. Progression was checked 4-hourly with neck girth measurements and a record of vertical extent. CT scan of the neck and chest with contrast showed a small breach just below the cricoid, intact pleura and lung parenchyma, and no features of mediastinitis (Figure 1). By the second day of admission, emphysema progressed with neck girth increasing to 18.6cm. Vertical extent progressed from zygoma up to upper abdomen i.e., grade 5 as described by Aghajanzadeh et al.4 However, this is not universally implemented.
Since the patient developed dyspnea, flexible tracheobronchoscopy was done which showed a fibrotic patch just below the cricoid but no frank tear up to the carina. Therefore, the airway was not intervened surgically allowing the defect to heal gradually. However, small sub-platysmal incisions were made in supraclavicular areas to facilitate the spontaneous expulsion of air from subcutaneous tissues. Emphysema slowly reduced and completely disappeared on the 5th post-procedure day. Hence, the patient was discharged and kept on follow-up. On 1 month follow-up, the patient had fully recovered (Figure 2).
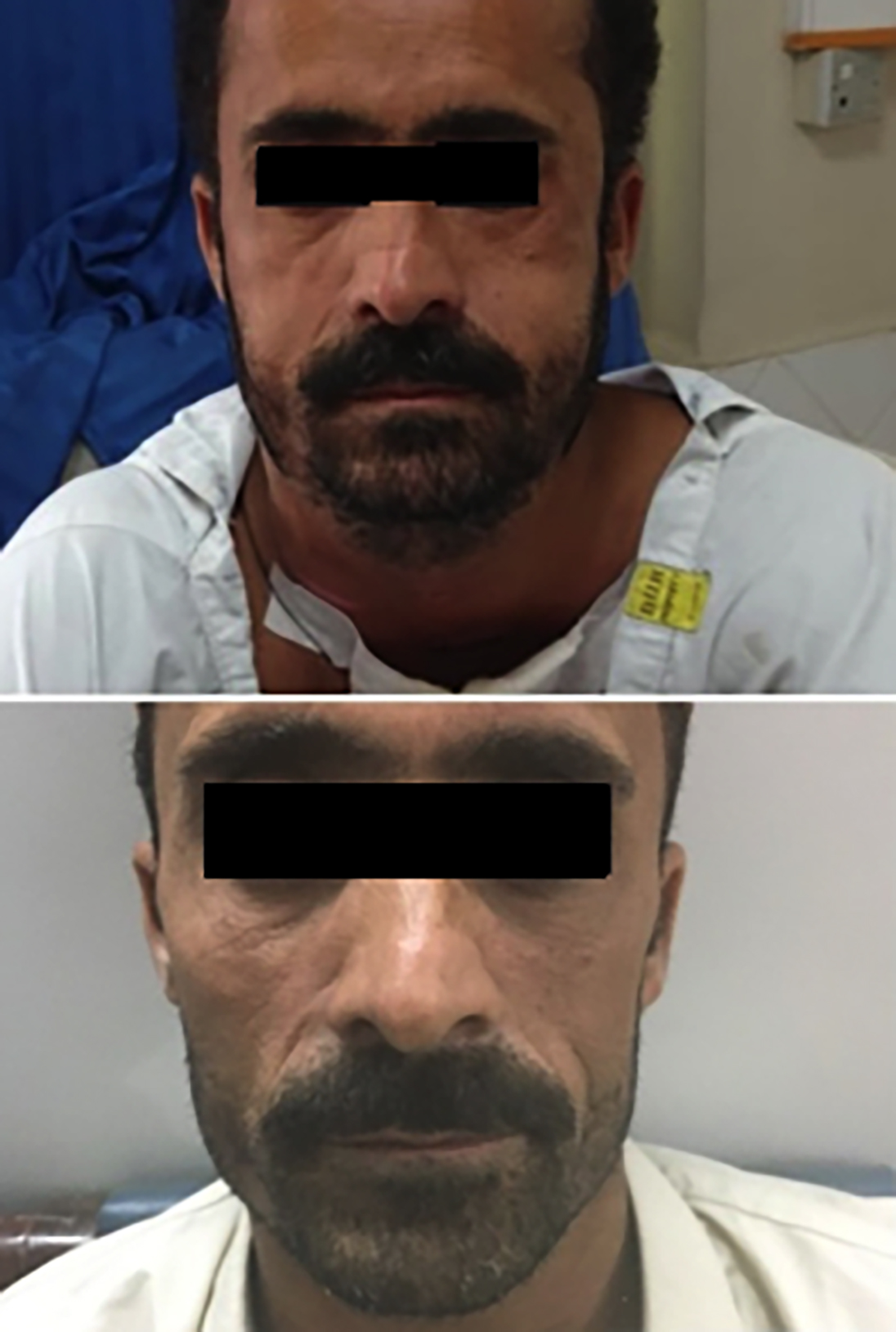 Figure 2: Patient’scondition A) Before the intervention, and, B) After resolution of subcutaneous emphysema.
Figure 2: Patient’scondition A) Before the intervention, and, B) After resolution of subcutaneous emphysema.
DISCUSSION
SE denotes presence of free air in the subcutaneous tissues. First described by Louise Bourgeois in 1617 and later characterised by Laennec in 1819,5 its occurrence can follow an injury, surgery, mechanical ventilation, or infection. In a few cases, precipitating events could not be identified.6 Pathophysiologically, air enters beneath the facial spaces and the connective tissue gets dissected along the muscle plane. This can further involve adjacent cervical and thoracic spaces.7Blunt trauma to the neck can cause injuries to deep structures. It can be clinically depicted by redness, bruising, swelling, and tenderness in the neck. Laryngotracheal injury can be fatal. SE, pneumo-mediastinum, or laryngeal deformity can be present.8 Severe emphysema can also cause cutaneous tension, dysphagia, dysphonia, and airway compromise culminating in respiratory failure. Radiography and endoscopic evaluation are recommended to evaluate for the aerodigestive injuries in both adults and children.9 Computed tomography is superior to plain radiography, with a reported sensitivity of 100% and specificity of 99% in the management of neck trauma.10
In such cases, resolution of swelling is important to unmask the true nature of the pathology and relieve compressive symptoms. The laryngeal tear discussed above probably led to the clinical picture in this patient. Since SE and pneumo-mediastinum secondary to minor laryngeal trauma are considered benign conditions that resolve spontaneously, only expectant management was applied. What is remarkable in this case is the use of small portals for air escape in the form of stab incisions on the neck that limited the progression and hastened the release of trapped air, and aided in achieving rapid recovery.
In conclusion, aerodynamically stable patients with cervical SE and pneumo-mediastinum after blunt neck trauma can be observed alone without invasive testing or repeat imaging. The goals of such management should be targeted, ensuring that significant airway injuries are not missed. CT scan is of great value and can help in planning management. Blowhole incisions allow the escape of air from subcutaneous tissues relieving the compressive effects and providing symptomatic and visual relief to the patient.
PATIENT’S CONSENT:
Informed consent was obtained from the patient to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
TK: Analysis of data, its interpretation and drafting.
MSJ: Data collection.
SZ: Acquisition and supervision.
IAMK: Final approval of the draft sent for publication.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Galvagno SM, Nahmias JT, David A. Young, advanced trauma life support update 2019: Management and applications for adults and special populations. Anesthesiol Clinics 2019; 37(1):13-32. doi: 10.1016/j.anclin.2018. 09.009.
- Banki F, Estrera AL, Harrison RG, Miller CC, Leake SS, Mitchell KG, et al. Pneumomediastinum: Etiology and a guide to diagnosis and treatment. Am J Surg 2013; 206(6):1001-6. doi: 10.1016/j.amjsurg.2013.08.009.
- Fosi S, Giuricin V, Girardi V, Di Caprera E, Costanzo E, Di Trapano R, et al. Subcutaneous emphysema, pneumomediastinum, pneumoretroperitoneum, and pneumoscrotum: Unusual complications of acute perforated diverticulitis. Case Rep Radiol 2014; 2014: 461563. doi: 10.1155/2014/431563.
- Aghajanzadeh M, Dehnadi A, Ebrahimi H, Fallah KM, Khajeh JS, Amir MA, et al. Classification and management of subcutaneous emphysema: A 10 year experience. Indian J Surg 2015; 77(Suppl 2):673-7. doi: 10.1007/s12262-013- 0975-4.
- Mansella G, Bingisser R, Nickel CH. Pneumomediastinum in blunt chest trauma: A case report and review of the literature. Case Rep Emerg Med 2014; 2014:685381. doi: 10.1155/2014/685381.
- Sahni S, Verma S, Grullon J, Esquire A, Patel P, Talwar A. Spontaneous pneumomediastinum: Time for consensus. N Am J Med Sci 2013; 5(Issue 8):460- 4. doi: 10.4103/1947- 2714.117296.
- McKenzie Wm, Rosenberg M. Iatrogenic Subcutaneous Emphysema of Dental and Surgical Origin: A Literature Review. J Oral Maxillofac Surg 2009; 67(Issue 6):1265-8.
- Marathe US, Tran LP. Pediatric neck trauma causing massive subcutaneous emphysema. J Trauma Acute Care Surg 2006; 61(Issue 2):440-3. doi: 10.1097/01.ta.0000 229909.39338.ce.
- Losek J, Tecklenburg F, White D. Blunt laryngeal trauma in children: Case report and review of initial airway management. Paediatric Emergency Care 2008; 24(6): 370-3. doi: 10.1097/PEC.0b013e318177a78a.
- Chew BG, Swartz C, Quigley MR, Altman DT, Daffner RH, Wilberger JE. Cervical spine clearance in the traum: Is multidetector CT scanning sufficient alone? J Neurosurg Spine 2013; 19(5):576-81. doi: 10.3171/2013.8.SPINE 12925.