Substance Abuse and Mental Health Issues Among HIV/AIDS Patients
By Khunsa Junaid, Saira Afzal, Muhammad Daood, Meha SiddiquiAffiliations
doi: 10.29271/jcpsp.2023.03.325ABSTRACT
Psychiatric morbidity commonly coexists with substance abuse and HIV/AIDS around the globe. This review study aimed to determine the available literature on the prevalence of common substance abuse/use and common mental health illnesses among HIV/AIDS patients worldwide to help policymakers design appropriate strategies to limit extensive substance use and prevent common mental and health illnesses. For the comprehensive literature review, Google Scholar, PubMed Central, Medline, and PakMediNet biomedical databases were searched for original and reviewed studies published in English, from January 2000 to September 2021. Selections of studies and extraction of data from the studies were performed based on quality and inclusion criteria. MedCalc Meta-analysis Software Package version 20.009 was used for data analysis. Out of 103,024 HIV/AIDS patients inspected in 30 studies, 6430 HIV/AIDS patients had pooled prevalence of depression 30.31% (95%CI: 26.028 to 34.786), and 6927 study participants reported the overall current pooled prevalence of any substance use was 25.13% (95%CI: 11.526 to 41.897), respectively. Current alcohol consumption and tobacco smoking are the most common substance abuse, and depression and anxiety are the most common mental health disorders among HIV/AIDS patients. There was no significant publication bias, but substantial heterogeneity was observed in the presented studies. The current systematic review and meta-analysis showed a greater prevalence of substance abuse and mental health illnesses among HIV/AIDS patients than the general population at the global level.
Key Words: Substances, Substance use, Substance abuse, Alcohol abuse, Tobacco smoking, HIV/AIDS, Depression, Anxiety, Mental health, HIV/AIDS, Worldwide.
INTRODUCTION
In 1980, the human immunodeficiency virus (HIV) epidemic was first recognised, and approximately 78 million people suffered from the HIV infection, and 39 million people died due to HIV causes. Globally, two-third of new HIV cases are reported in Sub-Saharan Africa.1,2 According to a recent UNAIDS survey in 2020, approximately 37.6 people had HIV/AIDS, and 690,000 [480,000–1 million] people died from AIDS-related illnesses in 2020.3 Various treatment modalities and policies have been designed, such as giving antiretroviral therapy (ART) to every HIV-positive patient regardless of their WHO HIV/AIDS stage and CD4 cell count.4
The World Health Organisation (WHO) describes substance use disorder as "the detrimental or dangerous consumption of any psychoactive substances comprising alcohol and other illegal drugs."
It has been found that more than half of the patients suffering from chronic medical conditions such as Diabetes Mellitus, Cancer, and HIV/AIDS are the cause of psychological disorders such as depression, anxiety, emotions, hallucination, and rage.5 Common mental disorder (CMD), occasionally termed as mental distress or psychological distress, is a gross name to describe various mental instabilities elucidated by the exhibition of depressive, anxiety, somatic, and rage symptoms. According to World Health Organization (WHO), depression contributed about 12% of disability-adjusted life years, and by 2030, depression and HIV/AIDS would be the foremost causes of disability globally.5,6 It has been noted that nearly 50 percent of HIV patients have reported past or current substance use or abuse. Substance abuse or use in HIV patients may show poor health outcomes and behaviour such as risky sexual practices, non-compliance of ART, and a greater burden on the health system.6,7
Psychiatric morbidity is commonly co-occurring with substance abuse and HIV/AIDS. The relationship is bi-directional, meaning individuals suffering from mental distress may drink or abuse substances more and vice versa.7,8 Besides increasing HIV transmission risk, these have also been responsible for rapid disease progression because of decreased CD4 cell count suppression, poor medication adherence, the greater threat of mortality and morbidity, and reduced efficiency. Globally, mental health disorders were more common among HIV patients than in general.9,10
The literature assessing the association between HIV outcomes and substance abuse has predominantly targeted the injection drug abuser. Still, there have been cumulative interest in smoking, alcohol, Khat, cocaine, and marijuana. Correspondingly, literature related to the psychological health problems has mostly focused on depression, with little notice on severe mental illness or anxiety. There is little literature assessing the comprehensive literature regarding triple diagnosis between substance abuse and mental illness concurring HIV/AIDS disease. Therefore, this review study evaluates the pooled prevalence of common psychiatric morbidity and common substance abuse among HIV/AIDS patients.
METHODOLOGY
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines 2020 were used for data reporting and analysis.11 MEDLINE, PubMed, PubMed Central, Google Scholar, PsycINFO, and PakMediNet were searched for publications, from January 2000 to September 2021. The authors also performed a literature search using direct websites of local journals. Relevant articles from databases were researched according to PICO: Patients/Problem = patients with a confirmed diagnosis of HIV/AIDS; Intervention = screening of mental health issues and substance abuse disorders by using validated screening tools; Comparison= no comparison group; Outcome= prevalence of mental health issues and substance abuse disorders among HIV/AIDS patients.
The following inclusion and exclusion criteria were developed to check the eligibility of the relevant primary studies to be included in the systematic review. The inclusion criteria defined as all observational studies (cross-sectional, case-control, and cohort studies) with the original data and review articles that evaluated the prevalence of substance abuse and psychological distress/mental health/mental distress among HIV/AIDS patients, studies published in English conducted on either male or female or both adults having age than 18 years or more, who abuse substances, specifically, any non medical use of prescription drugs, illicit drug (e.g., marijuana, heroin), or alcohol (liquor, wine) and use or tobacco, research papers that described a psychiatric finding established on the healthcare provider's diagnosis or used a validated scale with a well-defined cut-off (e.g., patient health questionnaire [PHQ-9] or the Beck Depression Inventory or Beck Anxiety Inventory). Articles on specific ethnic groups, pathophysiological conditions, dementia, organic mental disorders, and developmental delay among HIV/AIDS patients were not considered. Articles focused on neuropsychiatric or neurobiological aspects of the pathology among HIV/AIDS patients were not included. Moreover, studies of less educational implications, editorial articles, qualitative studies, commentaries, interventional studies, unpublished literature, and purely descriptive studies available in various scientific conferences without any quantitative and qualitative inferences were also excluded.
Mental health indicators include three areas; depression, anxiety, and psychological distress established on the diagnosis of healthcare provider or used a validated scale with a well-defined cut-off (e.g., patient health questionnaire [PHQ-9] or the Beck Depression Inventory or Beck Anxiety Inventory). Indicators of substance abuse include overall lifetime or current prevalence of any substance (alcohol, tobacco, cocaine, marijuana, methamphetamine, opioid, or any other substance). Two variables (alcohol and tobacco smoking) focused on capturing a range of substance-using behaviours among HIV/AIDS patients. Lifetime prevalence was described as the proportion of persons who have ever used any substance (alcohol, tobacco, cocaine, and marijuana, etc.), in his/her life. Current prevalence was described as the percentage of persons who have used any substance (alcohol, tobacco, cocaine, and marijuana, etc.); over the past three, six or twelve months in his/her life.
Various synonymic keywords in each database using Boolean operators, truncation, and a combination of Medical Subject Heading (MeSH) terms were utilised to include many relevant articles. Broad search keywords were: Substance use or substance use disorder, or alcohol drinking, or alcohol abuse, or tobacco abuse, or cocaine, or marijuana) and Prevalence of HIV, or human immune deficiency virus or AIDS or acquired immune deficiency syndrome) or (psychological distress or mental health disorder or depression or anxiety, and prevalence of HIV or human immune deficiency virus or AIDS or acquired immune deficiency syndrome). The eligibility of all research reports identified by the search strategy was assessed. Any doubts or disagreements were resolved by conferring the issue. The authors removed any duplicate studies manually. Initially, articles were assessed by studying their titles and abstracts, and afterwards, relevant studies were further assessed by reading their full text. Two authors independently selected the corresponding full-text article on final eligibility of reports. After the full-text assessment, thirty papers were eligible and included in this systematic review.
The information extracted was the name of the first author, the year of publication, study setting, study design, sample size, region, gender, diagnostic tool, lifetime or current prevalence of any substance abuse, current or lifetime prevalence of alcohol and tobacco smoking, the prevalence of psychological distress, depression, and anxiety. Data were synthesised by categorising the mental health components and substance abuse outcomes of the study examined. Any discrepancies raised during data extraction were resolved. A modified version of the Newcastle-Ottawa Scale (NOS) for cross-sectional and cohort studies was used to check the studies quality. The assessment of multiple systematic reviews (AMSTAR) scale evaluated the included reviews as a methodological quality assessment tool. Articles fulfilling a minimum of 50% of the quality assessment criteria score were incorporated in this review, and Microsoft Excel was used for the data extraction.
MedCalc, a Meta-analysis Software Package version 20.009 was used for data analysis. The random-effect model for meta-analysis was used to quantify the overall pooled prevalence of mental distress and substance abuse disorders among HIV/AIDS-infected patients. Prevalence estimates were reported with a 95% confidence interval (95% CI). Pooling of prevalence was done with a single arcsine transformation using a random-effect meta-analysis model. In this analysis, the main outcome of interest was the current prevalence of any substance use and depression among HIV/AIDS patients. Using the Q and I2 statistics, the amount of statistical heterogeneity between the eligible articles was calculated. The 25%, 50%, and 75% represented low, medium, and high-quality heterogeneity, respectively. Sub-group analysis was executed to determine the potential source of heterogeneity. The funnel plot and Egger's regression tests assessed potential publication bias. In the case of significant heterogeneity, random-effect models were used to determine pooled prevalence. The CI of the observed data was set at 95%, and statistical significance was at a p-value ≤.05.
RESULTS
According to the literature search, 856 studies were identified through various databases (Figure 1). From a total of 856 studies, 198 were excluded due to duplication, and 658 records were further excluded after screening the title and abstract of the studies. A total of 388 reports were assessed for quality and eligibility, and from these, 30 studies were included in the final systematic review, as shown in Figure 1.7,12-29
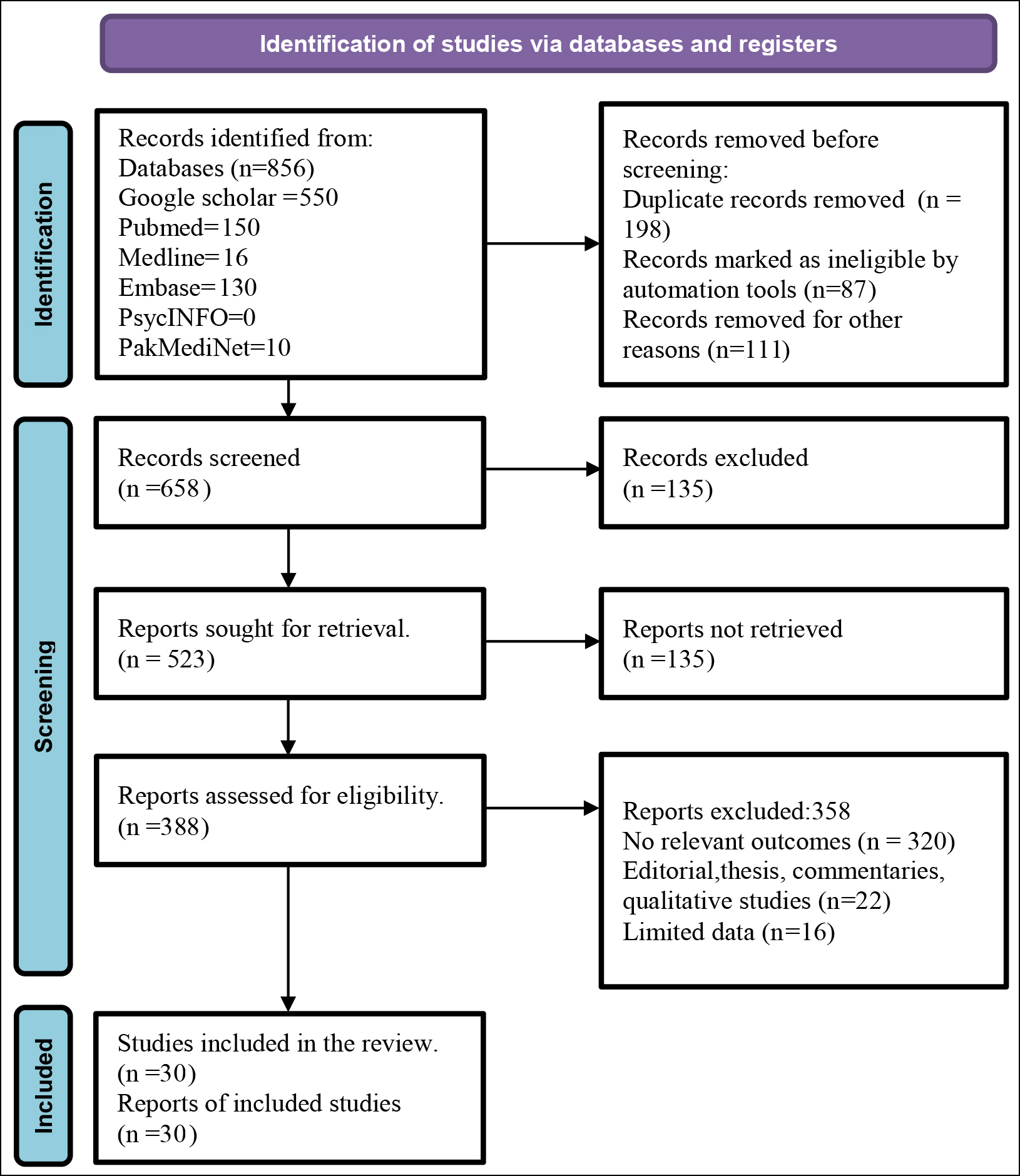 Figure 1: PRISMA Flowchart of the study selection procedure.
Figure 1: PRISMA Flowchart of the study selection procedure.
The detail of the key characteristics of included studies is mentioned in Table I.12-41 Fourteen of the presented studies were from the African regions. Nine studies were from the United States of America (USA), and a few studies were from China, India, Spain, Russia, and the Netherlands. Sixty-two is the minimum sample size range, and 45,783 is the maximum sample size range in the presented studies, as mentioned in Table I. Each of the included studies was varied in study designs and outcomes were measured. Sixteen studies reported depression. Various scales were used by studies such as beck depression inventory (BDI) (2 studies), Centre for Epidemiologic Studies Depression Scale (CES-D) (nine studies), structured clinical interview for DSM-III-R (SCID) (three studies), depression, anxiety and stress scale-21 Items (DASS-21) (one study), MINI (One study), patient health questionnaire (PHQ) (1 study), World Mental Health (WMH) (WHO) composite international diagnostic interview (CIDI) (two studies), hamilton depression rating scale (HDRS) (1 study). Six studies reported anxiety. State-trait anxiety inventory (STAI) (two studies, depression, anxiety, and stress scale-21 Items (DASS-21) (one study), Beck depression inventory (BDI) (one study), World Mental Health (WMH), (WHO) composite international diagnostic interview (CIDI) (one study). Seven studies reported psychological distress. Brief symptom inventory (BSI) (one study), Kessler psychological distress Scale (K10) (four studies), and self-report screening tool (SRQ-20) (1 study).
Concerning the methodological quality of observational studies, 17/25 (68%) studies had a low risk of bias, 7/25 (28%) had a moderate risk of bias, and 1/25 (4%) had a high risk of bias. Concerning the methodological quality of reviews studies, all five review studies had moderate quality studies.
Meta-analysis was done on eight studies for the prevalence of substance abuse among HIV/AIDS patients and ten studies for depression among HIV/AIDS patients due to the heterogeneity of outcome measures across chosen studies. Current prevalence of any substance use (cocaine, marijuana, alcohol, cigarette smoking, etc.), was reported in eight studies. All eight studies (n= 6927 study participants), who reported current prevalence of any substance abuse were included in the meta-analysis, and the overall pooled current prevalence of any substance use was 25.13% (95% CI: 11.526 to 41.897) (Figure 2A) according to random-effect methods. Among studies, the substantial heterogeneity with (I2 =99.39% Q=1150.3900, df=7, p <0.0001, 95% CI for I2: 99.24 to 99.51) were present and according to Egger’s test (p <0.3112) and Begg’s test (p <0.8046), revealed no significant publication bias (Figure 2B). Subgroup analysis was performed to determine the possible source of substantial heterogeneity. The detail of the subgroup analysis is mentioned in Table II.
All ten studies (n=6430 study participants) that reported the prevalence of depression among HIV/AIDS patients were included in the meta-analysis. According to the random-effect methods, the overall pooled prevalence of depression was 30.31% (95% CI: 26.028 to 34.786) (Table III). Among studies, the substantial heterogeneity with (I2=89.84%% Q=88.5435, df=9, p <0.0001, 95% CI for I2: 83.44 to 93.76) were present and according to Egger’s test p <0.5339 and Begg’s test p <0.5312, revealed no significant publication bias (Figure 3 A and B). The detail of sub-group analysis is mentioned in Table III. The higher pooled prevalence estimate of depression in HIV/AIDS patients were reported in studies from the non-African Region (30.52%). The studies used other depression screening instruments (PHQ-9, HADS, BDI, IDS, and DASS-21) 33.35%.
Table I: Characteristics of studies included in the systematic review.|
Author, Year |
Study Design
|
Country |
Patients (n)
|
Study setting |
Male, N (%) |
Female N (%) |
Outcome Mental Health |
Outcome Substance use |
Quality assessment |
|
|
|
|
|
|
|
|
Depression: N (%) Anxiety: N (%) Psychological distress: N (%) |
Any Substance abuse/use: N (%) Alcohol abuse/dependence: N (%) Cigarettes Smoking: N (%) |
|
|
1. Kalichman SC (2000)12 |
Cross-sectional study |
USA |
113 |
Institution-based |
85(75.2) |
28(24.7) |
Depression (mean±SD BDI score): 9.6±6.4 |
N/A |
NOS=5 |
|
2. Passik SD (2000)13 |
Cross-sectional study |
USA |
111 |
Institution-based |
N/A |
111 |
N/A |
Alcohol abuse/dependence: Lifetime: 70(64.2 %) Current: 26 (23.5%) |
NOS=6 |
|
3. Catz SL (2002)14 |
Cross-sectional study |
USA |
100 |
Institution-based |
N/A |
100 |
Depression (CES-D mean±SD): 24.9±12.5 Anxiety (STAI-state mean±SD): 43.0±14.0 |
N/A |
NOS=6 |
|
4. Gritz ER (2004)15 |
Cross-sectional study |
USA |
348 |
Institution-based |
272(78.1%) |
76(21.8) |
44(51.2%) current smokers were depressed; 16(18.6%) former smokers were depressed |
Smoking: Lifetime: 218 (62.8 %) Current: 162 (46.9%) |
NOS=6 |
|
5. Milam JE (2004)16 |
Cohort study |
USA |
835 |
Institution-based |
727 (87.1) |
108(12.9) |
Depression (CES-D mean±SD): 11.02± 9.70
|
Illicit drug use had significantly higher PTSD scores |
NOS=6 |
|
6. Krupitsky EM (2005)17 |
Cross-sectional study |
Russia |
201 |
Institution-based |
125(62.1) |
76 (38%) |
N/A |
Alcohol abuse/dependence: Lifetime: 19(9 %) Current: N/A |
NOS=6 |
|
7. Collins PY (2006)18 |
Systematic review |
Brazil, China, India, Kenya, Nepal, Russia, South Africa, Taiwan, Tanzania, Thailand Zaire, and Zimbabwe |
13 studies (n=3242) |
Istitutionbased:10 Community based:11 |
N/A |
N/A |
Depression rates among HIV-positive participants ranged from 0% to 63.3 per cent. |
N/A |
AMSTAR=6
|
|
8. Kalichman SC(2007)19 |
Systematic review |
Sub-Saharan Africa |
34 studies (n=45,783) |
N/A |
14860 (32.45) |
30923 (67.54) |
N/A |
Studies conducted in southern Africa confirm alcohol use and HIV sexual risks. |
AMSTAR=6
|
|
9. Brandt R (2009)20 |
Systematic review |
South Africa:12 Kenya:3 Senegal, Nigeria, Tanzania: Zambia, Angola, Zimbabwe, and Congo:1
|
23 studies |
Institution-based: 13 Community-based:10 |
N/A |
N/A |
Most studies find that approximately half of the HIV-infected adults sampled had psychiatric disorders, with depression being the most common individual problem. |
N/A |
AMSTAR=7
|
|
10. Sherr L (2011)21 |
Systematic review |
North America: 67(74.4%) Europe: 14 (15.5%) Africa, Asia, and South America: 9(10%) |
90 studies 2903 |
N/A |
N/A |
N/A |
Depression (only 18 studies): Four studies: (BDI: 12 to 71%) 3 studies: (BD1: 11 to 31.7%) Six studies: (CES-D: 35 to 42%) Three studies (DSM-III-R SCID: (30.6 to 80%) Two studies: (HAM-D: 8 to 56%) Prevalence rates of depression ranged from 0 to 80% |
N/A |
AMSTAR=6
|
|
11.Brown T (2013) 22 |
Cross-sectional |
Jamaica |
62 |
Institution-based |
27(43.5) |
35(56.5) |
Depression: (DASS21):39(63%) Anxiety: (DASS-21): 44(71%)
|
Alcohol abuse/dependence: Lifetime: 19(9 %) Current: N/A Smoking: Current: 7(11.4%) Lifetime: N/A |
NOS=7
|
|
12. Schadé A (2013)23
|
Prospective Cohort study |
Netherlands |
196 |
Institution based |
172(87.7) |
24(12.2) |
Depression: (MINI): 51(26%) Anxiety: (BAI): 42(21.4%) |
Any substance abuse/use: Lifetime: 20(10.2%) Current: N/A Alcohol abuse/dependence: Lifetime: N/A Current: 11(5.6%) |
NOS=6
|
|
13.ScottSheldon LA (2013) 24 |
Nested cross-sectional study |
South Africa |
1,717 |
Community-based |
1125(65.5) |
592 (34) |
N/A |
Alcohol abuse/dependence: Current: 1255(73%) Lifetime: 1530 (89%) |
NOS=7
|
|
14. Chibanda D (2014)25 |
Systematic review |
Low- and middle-income countries |
21 studies (8757) |
N/A |
N/A |
N/A |
Depression is more prevalent among HIV/AIDS than in the general population, with an estimated 5%–20%. |
Alcohol is the most abused substance in Sub-Saharan Africa, corresponding to 70% of the world's HIV/AIDS. |
AMSTAR=6
|
|
15.Uebelacker LA (2015)26 |
Cross-sectional |
England
|
238 |
Institution-based |
149(62.6)
|
89(37.3)
|
Depression: (CESD): 41 (38%)
|
Any substance abuse/use: Lifetime: N/A Current: 9(8.4%) Alcohol abuse/dependence N (%): Lifetime: N/A Current: 10(9%) |
NOS=7
|
|
16. Secor AM (2015)27 |
Cross-sectional survey |
Coastal Kenya |
112 |
Institution-based |
112 (100) |
N/A |
Depression: (PHQ-9): 18(16.1%)
|
Any substance abuse/use: Current: 67(59.8) Lifetime: NA Alcohol abuse/dependence N (%): Current: 51(45%) Lifetime: NA |
NOS=7
|
|
17. Zhang C (2016)28 |
Cross-sectional study |
China |
2,987 |
Community-based |
N/A |
N/A |
N/A |
Any substance abuse/use: Current: 569(19.3%) Lifetime: NA Alcohol abuse/dependence n (%): Current: 1280(42.76%) Lifetime: NA Smoking: Current: 1545(51.57%) Lifetime: NA |
NOS=7
|
|
18. Quinn K (2017) 29 |
Nested cross-sectional study |
Chicago |
92 |
Institution-based |
92(100.0)
|
N/A |
Psychological distress: (BSI-18) 12(13.0%)
|
Any substance abuse/use: Current: NA Lifetime: 35(38%) Smoking: Current: 37(41.3%) Lifetime: NA |
NOS=7
|
|
19. Egbe CO et al. (2017)30 |
Cross-sectional study |
Nigeria |
1187 |
Institution-based |
789(66.5) |
398(33.5) |
Depression (WMH-CIDI) 339(28.2%) |
Alcohol abuse/dependence n (%): Current: 84(7.0%) Lifetime: N/A |
NOS=8
|
|
20. Cichowitz C (2017) 31 |
A prospective cohort study |
South Africa |
136 |
Institution-based |
69(50.7) |
67(49.3) |
N/A |
Alcohol abuse/dependence n (%): Current: 1280(42.76%) Lifetime: NA |
NOS=8
|
|
21. Mthembu JC (2017) 32 |
Cross-sectional study |
South Africa |
25,860
|
Community-based |
11,185(19.6) |
14675(27.8) |
Psychological distress (K-10): 6180(23.9%) |
Alcohol abuse/dependence n (%): Current: 15220(58.9%) Lifetime: NA |
NOS=7
|
|
22. Cook JA (2018)33 |
Nested study |
USA |
1027 |
Community-based |
N/A |
1027(100) |
Depression (WMH-CIDI): 337(32.4%) Anxiety (WMH-CIDI): 135(13.2%) |
Alcohol abuse/dependence n (%): Current: N/A Lifetime:58.3% Smoking: Current: 202(19.6%) Lifetime: NA |
NOS=7
|
| Continued... |
|
Author, Year |
Study Design
|
Country |
Patients (n)
|
Study setting |
Male, N (%) |
Female N (%) |
Outcome Mental Health |
Outcome Substance use |
Quality assessment |
|
|
|
|
|
|
|
|
Depression: N (%) Anxiety: N (%) Psychological distress: N (%) |
Any Substance abuse/use: N (%) Alcohol abuse/dependence: N (%) Cigarettes Smoking: N (%) |
|
|
23. Bassey RB (2018)34 |
Cross-sectional study |
USA |
282 |
Community-based |
152(54)
|
130(46) |
Depression (CIDI): 113(50%)
|
Any substance abuse/use: Current: 236 (86%) Lifetime: N/A |
NOS=7
|
|
24. Glynn TR (2019)35
|
Nested cross-sectional study |
USA |
240 |
Institution-based |
165(68.8)
|
75(31.25) |
N/A |
Any substance abuse/use: Current: 43(17.9% Lifetime: N/A |
NOS=7
|
|
25. Basha EA (2019)36 |
Cross-sectional survey |
Ethiopia |
422 |
Institution-based |
156 (37)
|
266 (63) |
Psychological distress (SRQ-20): 32(7.8%)
|
Alcohol abuse/dependence n (%): Current: 8(1.9%) Lifetime: NA Smoking: Current: 8(1.9%) Lifetime: NA |
NOS=8
|
|
26. Bitty Anderson AM (2019) 37 |
Cross-sectional |
Togo |
2115 |
Community-based |
641(30.3) |
1474(69.6) |
Psychological distress (K10): 136(6.4%)
|
Alcohol abuse/dependence n (%): Current: 1370(64.8%) Lifetime: NA Smoking: Current: 649(30.6%) Lifetime: NA |
NOS=7
|
|
27.SinghNK (2020)38 |
Retrospective chart review |
India |
2914 |
Institution-based |
2632(90.3) |
282(9.6) |
Depression: 792(27%) Anxiety: 659(23%) |
Any substance abuse/use: Current: 151(5.1%) Lifetime: NA Alcohol abuse/dependence n (%): Current: 2248(77%) Lifetime: NA |
NOS=7
|
|
28. Tchankoni MK (2020)39 |
Cross-sectional |
Togo |
280 |
Community-based |
78(27.8) |
202(72.1) |
Psychological distress (K10): 69 (24.6%) |
Smoking: Current: 175 (49.4%) Lifetime: NA |
NOS=6
|
|
29. Higueras CV (2020)40 |
Cross-sectional |
Spain |
75 |
Institution-based |
14(38.8) |
22(61.5) |
Depression (BDI): 12(33.3%) Anxiety: (STA) 5(13.9%) Psychological distress 25 (71.4%)
|
Alcohol abuse/dependence n (%): Current: 20 (58.8%) Lifetime: N/A Smoking: Current: 11 (31.4%) Lifetime: N/A |
NOS=7
|
|
30. Moges NA (2021)41 |
Cross-sectional |
Northwest Ethiopia |
689 |
Community-based |
291(42.0) |
398(57.8) |
Psychological distress (K10): 402(58.63)
|
Alcohol abuse/dependence n (%): Current: 150 (30.2%) Lifetime: 497(72.1%) |
NOS=7
|
|
Geographic location or country |
Observation (N) |
Prevalence (%) |
95% CI |
I2 |
Q |
df |
p-value |
|
Non-African Region |
7 |
20.889 |
8.177 - 37.528 |
99.42% |
1035.9936 |
6 |
p <0.0001 |
|
Sample size (n) |
|
|
|
|
|
|
|
|
<400 |
6 |
30.740 |
6.166- 63.72 |
99.14% |
578.2174 |
6 |
p <0.0001 |
|
>400 |
2 |
11.178 |
1.519 -28.058 |
99.66% |
290.3252 |
1 |
p <0.0001 |
|
Study setting |
|
|
|
|
|
|
|
|
Hospital/Institution |
6 |
17.435 |
6.582 - 32.072 |
97.87% |
235.0420 |
5 |
p <0.0001 |
|
Year of publication |
|
|
|
|
|
|
|
|
2010-2015 |
3 |
23.655 |
0.459 - 65.979 |
98.60% |
143.1480 |
2 |
p <0.0001 |
|
2016-2021 |
5 |
26.060 |
9.305 - 47.614 |
99.60% |
1004.6003 |
4 |
p <0.0001 |
Table III: Prevalence of depression in people with HIV globally: Subgroup meta-analysis and heterogeneity analysis.
|
Geographic location or country |
Observation (N) |
Prevalence (%) |
95% CI |
I2 |
Q |
df |
p-value |
|
African Region |
3 |
26.12 |
18.581 to 34.446 |
81.73% |
10.9439 |
2 |
p<0.0042 |
|
Non-African Region |
8 |
30.52 |
24.805 to 36.566 |
92.43 |
92.5294 |
7 |
p<0.0001 |
|
Sample size |
|
|
|
|
|
|
|
|
<400 |
8 |
29.712 |
20.947 to 39.305 |
92.32 |
91.1398 |
7 |
p <0.0001 |
|
>400 |
3 |
29.365 |
26.205 to 32.627 |
82.68% |
11.5494 |
2 |
p <0.0031 |
|
Study setting |
|
|
|
|
|
|
|
|
Hospital/Institution |
9 |
27.275 |
22.695 to 32.109 |
88.68% |
70.6698 |
8 |
p <0.0001 |
|
Diagnostic tool |
|
|
|
|
|
|
|
|
ICD-10 |
2 |
33.217 |
21.309 to 46.331 |
94.86% |
19.4502 |
1 |
p <0.0001 |
|
WHO-CIDI |
2 |
30.651 |
26.568 to 34.892 |
78.68% |
4.6909 |
1 |
p <0.0303 |
|
CES-D |
2 |
17.707 |
14.425 to 21.246 |
0.00% |
0.03874 |
1 |
p <0.8440 |
|
Others |
5 |
33.358 |
20.729 to 47.339 |
90.59% |
42.5155 |
4 |
p <0.0001 |
|
Year of publication |
|
|
|
|
|
|
|
|
2010-2015 |
4 |
28.931 |
14.922 to 45.390 |
94.20% |
51.7429 |
3 |
p <0.0001 |
|
2016-2021 |
7 |
28.817 |
27.657 to 29.999 |
86.71% |
45.1419 |
6 |
p <0.0001 |
DISCUSSION
According to the meta-analysis results, the current prevalence of substance use and depression among HIV/AIDS patients was 25.13% and 30.31%, respectively. According to one study, 10-28% of HIV/AIDS patients have co-occurring psychiatric and substance abuse disorders.26,37,40,42 Depression, mood disorders, anxiety disorders, sleep disorders, and other somatic complaints were the most prevalent psychiatric disorders affecting more than 50% of HIV/AIDS patients. An institution-based cross-sectional study conducted in Ethiopia reported a 20% prevalence of depression among HIV and AIDS patients.43 Another study conducted in Kenya, also reported undetected psychiatric morbidity was 71.4%, and the most common were major depressive disorder (MDD) (32.2%), posttraumatic stress disorder (PTSD) (18.4%), dysthymia (17.6%), and obsessive-compulsive disorder (OCD) (17.6%) respectively.44 A study conducted in United States showed that the prevalence rate of substance abuse disorders among HIV/AIDS patients was 48%.45 There are greater inconsistencies in the reported prevalence of substance abuse and mental health issues due to different sample features, diagnostic criteria, and investigated periods.
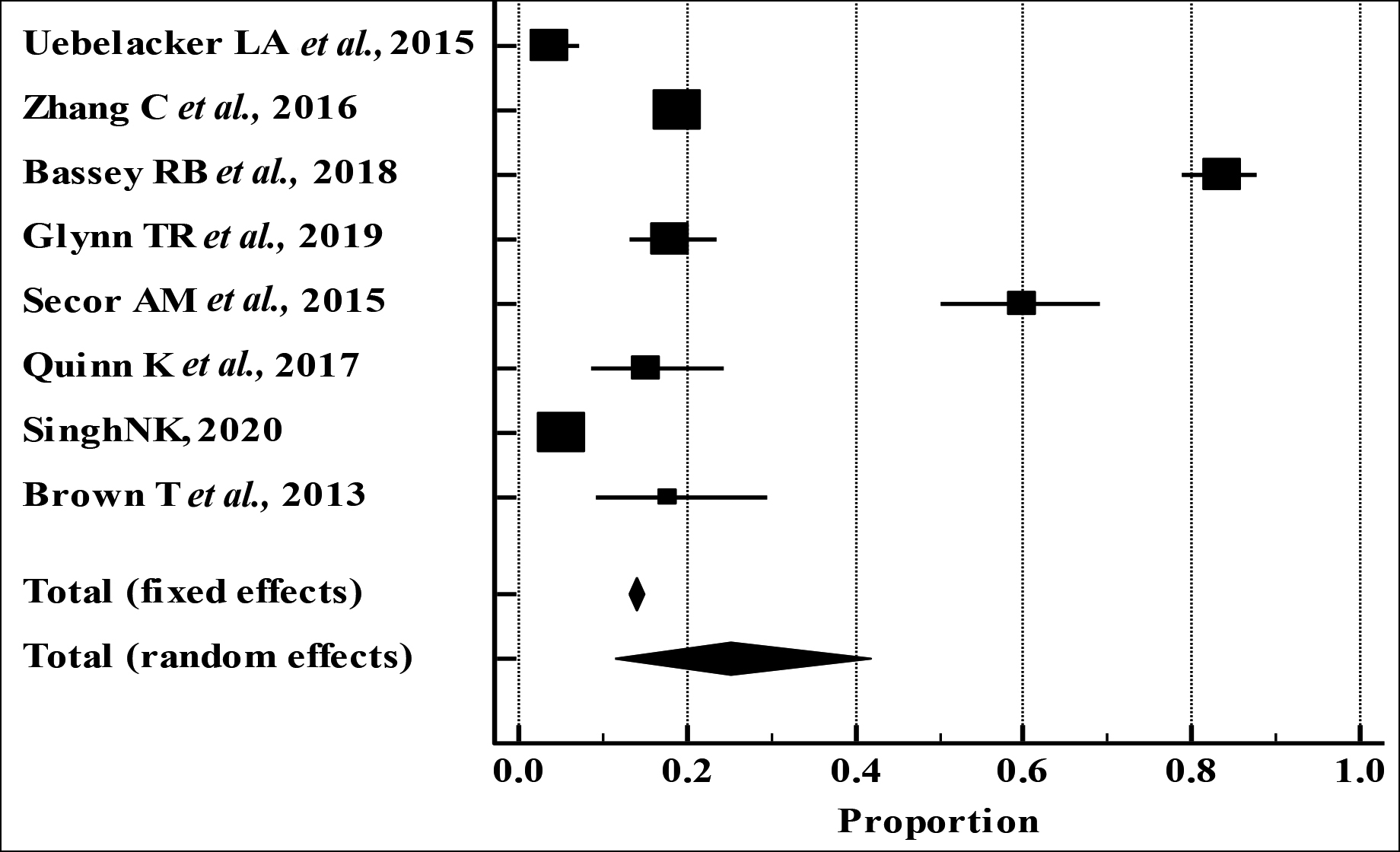 Figure 2(A): Forest plot of the prevalence of current substance use among HIV/AIDS patients: A meta-analysis.
Figure 2(A): Forest plot of the prevalence of current substance use among HIV/AIDS patients: A meta-analysis.
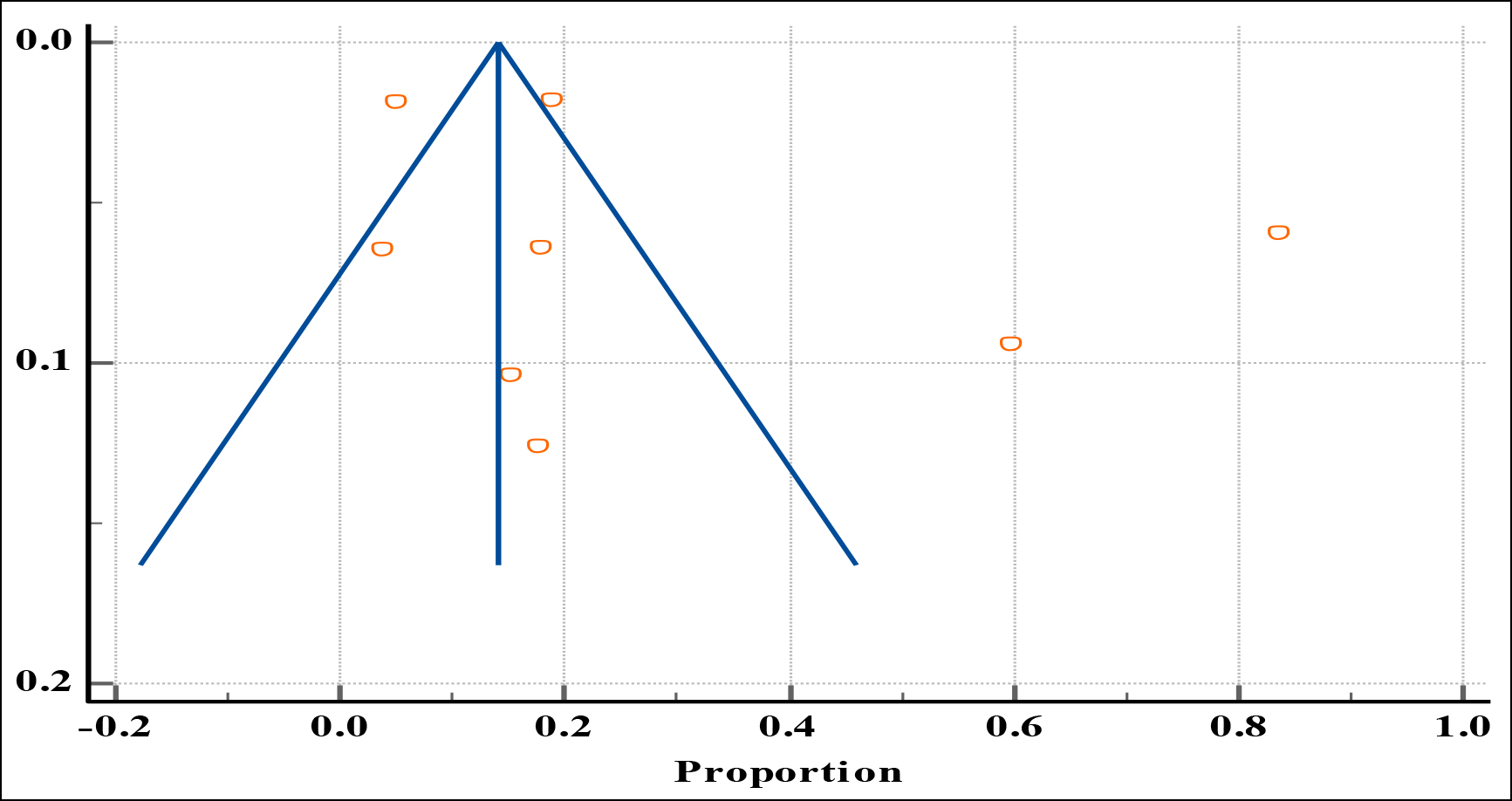 Figure 2(B): Funnel plot of the risk of publication bias for the prevalence of current substance use in HIV/AIDS patients
Figure 2(B): Funnel plot of the risk of publication bias for the prevalence of current substance use in HIV/AIDS patients
According to previous studies, consumption of alcohol, cigarette smoking, Khat abuse, and cocaine abuse among HIV/AIDS patients in the various parts of Ethiopia are most common and responsible for the greater hazard of developing mental health disorders and unsafe sexual and violent behaviour. The present results reported the current prevalence of tobacco smoking in seven studies. The prevalence ranged from 1.9% to 51.5%, and the lifetime prevalence of tobacco smoking was reported only in one study 16%. According to the data from the HIV cost services and utilisation survey (HCSUS), HIV-infected individuals, who currently abuse heavy alcohol, tobacco smoking, and the use of cocaine and heroin are more likely to experience psychiatric problems than general population. In a study conducted in Nepal, the prevalence of current tobacco smoking was 26.5%, and drinking of alcohol was 22.7%.46 According to the present results, the prevalence of current alcohol consumption was more reported in the fifteen studies ranging from 1.9% to 77% compared to current tobacco smoking prevalence ranging from 1.9% to 51.5%. This finding was consistent with previous studies on substance abuse disorders among HIV/AIDS patients, which indicates that alcohol consumption was greater among HIV-infected people than the general population.46,47 According to the findings of a review done on alcohol abuse disorders among HIV/AIDS patients by Duko et al.,47 the average global prevalence of alcohol abuse was 29.8%. Another meta-analysis on alcohol abuse disorders among HIV/AIDS patients indicates that the average one-year prevalence of alcohol abuse was 22.03%.46
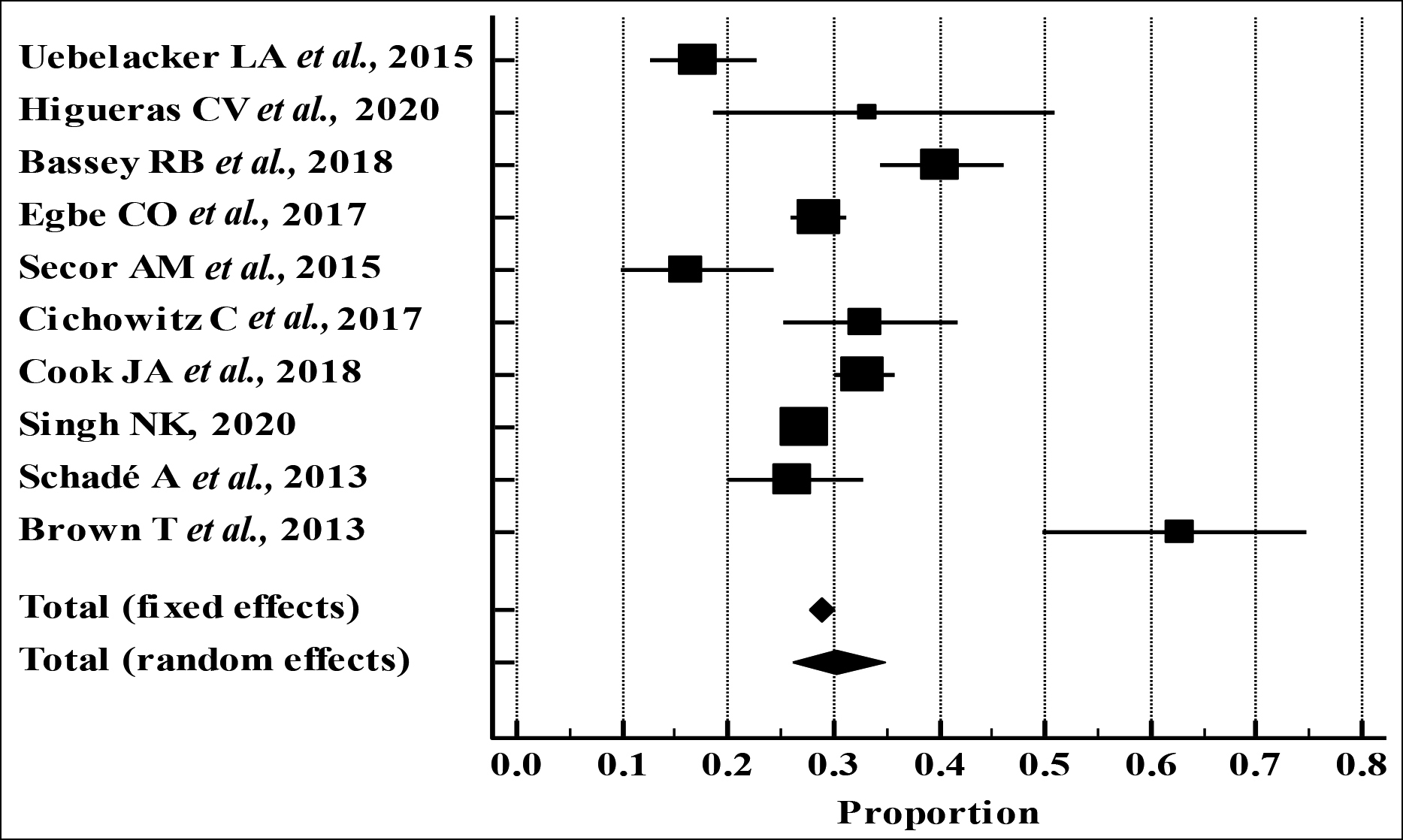 Figure 3 (A): Forest plot of the prevalence of depression among HIV/AIDS patients: A meta-analysis.
Figure 3 (A): Forest plot of the prevalence of depression among HIV/AIDS patients: A meta-analysis.
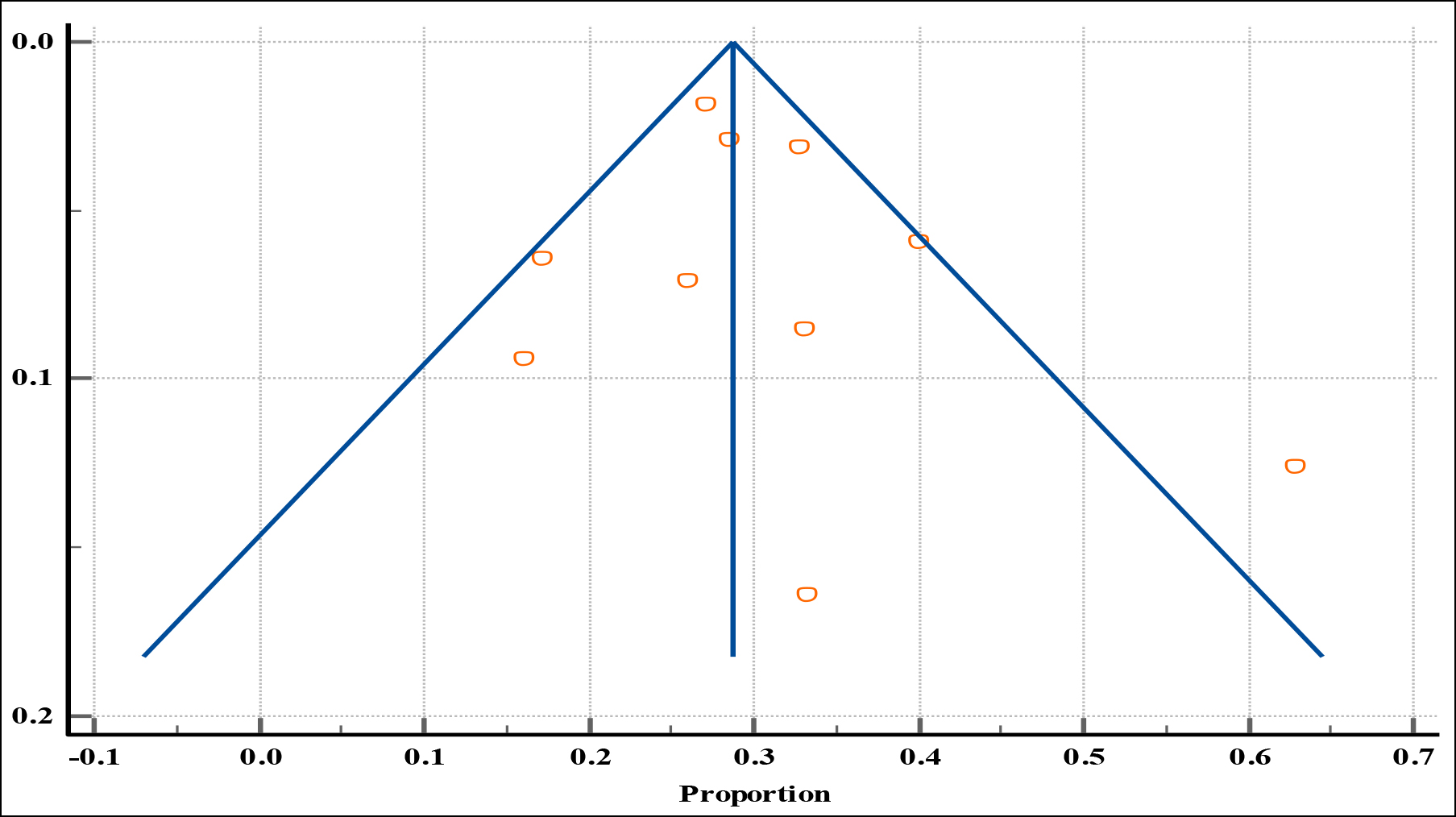 Figure 3 (B): Funnel plot of the risk of publication bias for the prevalence of depression in HIV/AIDS patients.
Figure 3 (B): Funnel plot of the risk of publication bias for the prevalence of depression in HIV/AIDS patients.
Less reporting of tobacco smoking in the included studies in this review might be due to dissimilarity in sample features, diagnostic, different investigated periods, and under-reporting of tobacco smoking, especially among the female study participants, which may not reproduce the exact prevalence.
Among psychiatric morbidity, depression was more reported in the studies than anxiety and psychological distress among HIV/AIDS patients in the current systematic review. This finding was consistent with the previous study's findings, which indicate that psychiatric depression (36.4%) was the most common mental health disorder among HIV/AIDS patients’ apart from suicidal thoughts, alcohol abuse-associated problems, and anxiety disorders.47,48 This may be due to the predominantly increase in the expansion of research on the depression among HIV/AIDS patients concerning the magnitude and current importance and hence, the production of the greater scientific volume.49
As mentioned in this review, drug abuse and mental health problems are most common globally but their prevalence is high among HIV/AIDS patients as compared to the general population. Significantly, various studies have studied the effects of drugs, including cocaine, amphetamines, and marijuana and found that alcohol and tobacco smoking was the most common substance abuse among HIV and AIDS patients.42 This systematic review mainly documented the current prevalence of substance abuse, alcohol consumption, and tobacco smoking. The results did not show a pooled prevalence of lifetime substance abuse because of the limited data available in the studies. This finding was consistent with the most large studies and various systematic reviews showed that many substance abusers were the current abusers in the studies.46,47
Subgroup analysis based on the region showed the pooled prevalence estimates of current substance abuse in HIV/AIDS patients in the non-African Region were 20.88%. The majority of representative data on the current prevalence of substance abuse among HIV/AIDS patients were identified from developed countries such as England, China, the USA, and Jamaica. This finding was consistent with the results of previous studies, which showed that the prevalence of substance use in developed countries was significantly higher than the developing countries.46,47 Based on the sample size, the pooled prevalence estimates of current substance abuse in HIV/AIDS patients for studies using sample size (n <400) was significantly higher, 30.74%. The majority of representative data on the current prevalence of substance abuse among HIV/AIDS patients were identified from studies using less than 400.22,26-30 This difference in sample size might be responsible for the difference in the prevalence. Subgroup analysis by study setting where studies were carried out was also performed. The pooled prevalence estimates of current substance abuse in HIV/AIDS patients for studies conducted in an institution was 17.435%. These findings are lesser than the un-pooled results of current substance abuse among HIV/AIDS patients in a community setting, which stated that the prevalence of substance abuse was 19.3% and 86%, respectively.28,34 This difference in prevalence maybe because all institution-based studies included in this systematic review mostly used screening tools to evaluate substance use disorders. In contrast, the community-based studies mostly relied on the self-reporting of substance abuse.
Moreover, in subgroup analysis based on the region, the pooled prevalence estimates of depression in HIV/AIDS patients in the non-African Region was 30.52% which was significantly higher than the pooled prevalence estimates of depression in HIV/AIDS patients in the African Region was 26.12%. This disparity may be due to the most representative data on the prevalence of depression among HIV/AIDS patients identified from non-African countries such as England, China, the USA, and Jamaica. In the present review subgroup analysis, the prevalence of depression revealed substantial disparities based on the measurement used to define depression in HIV/AIDS patients. The prevalence estimates of depression in HIV/AIDS patients for studies using ICD-10 were 33.21%, WHO-CIDI 30.65%, CES-D 17.07%, and others (PHQ-9, HADS, BDI, IDS, and DASS-21) 33.358%, respectively. According to another systematic review and meta-analysis, the pooled prevalence was seemingly greater in studies conducted using screening instruments than diagnostic instruments.50 For example, the pooled prevalence of depression in HIV/AIDS for studies using CES-D was 66.14%, HADS (51.30%), DSM or ICD (12.40%), PHQ-9 (32.15%), and HSC-D (30.50%), respectively.50 This apparent difference might be due to the fact that screening instrument used to assess depression provides more weight towards high sensitivity in contrast to a diagnostic instrument which provides more weight towards high specificity and variation in the sensitivity and specificity of the tools used to screen depression among HIV/AIDS patients.
The current meta-analysis showed that most of the studies have a moderate and low-risk of bias according to the Newcastle-Ottawa Scale (NOS) version. The results of the current meta-analysis revealed a substantial level of heterogeneity in the analysis due to disparities between the various studies. The possible disparity in the prevalence rate of depression and substance abuse among HIV/AIDS patients might be described by variation in the study population, study setting, sample size, variation in the sensitivity, and specificity of the tools used to screen depression, culture, and socioeconomic status of the countries, and availability of various substances in the countries.
The current meta-analysis revealed a substantial number of HIV/AIDS infected patients exposed to substance abuse and mental health disorders. Co-occurring substance abuse and mental health disorders have a detrimental effect on the health of HIV/AIDS patients. For example, various studies revealed that HIV/AIDS patients suffering from mental health and substance abuse disorders resulted in poor compliance of (ART), a decrease of CD4 cell count, higher viral load, speedy progression of various co-infections, and risky erotic activities which further enhanced the danger of HIV/AIDS transmission.31,33
Due to the strict PRISMA guidelines, the current systematic review reported the representative estimates. To ease the accessibility of evidence for concerned policymakers, the prevalence of common mental health disorders and substance abuse among HIV/ AIDS patients was comprehensively reported. Furthermore, two authors independently extracted data to lessen the probable risks.
The majority of the studies identified in this study were conducted in English and in countries in Africa and Sub-Saharan Africa, increasing the likelihood that the prevalence of mental health and substance abuse disorders in patients with AIDS/HIV would not be reported from other regions and continents. So, caution should be used when generalising the findings of this systematic review globally. It might be a good idea for future research and study. The current meta-analysis has few restrictions to consider in using its results findings. The current systematic review and meta-analysis were under the effect of substantial heterogeneity. Few studies were in the meta-analysis, affecting the estimate's precision. Furthermore, this meta-analysis mainly reports the current pooled prevalence of substance abuse. The results did not show the pooled prevalence of lifetime substance abuse because of limited data or insufficient data on lifetime prevalence of substance abuse in the studies. A large number of substance abusers were the current abusers in the studies.
CONCLUSION
This meta-analysis indicated that the overall pooled prevalence of any current substance use was 25.13%. The prevalence of depression among HIV/AIDS patients was 30.31% compared to the general population. Therefore, policymakers should designed strict strategies to limit the extensive utilisation of substance abuse. There should be an incorporation of psycho-social provision and mental health services with curative services for HIV/AIDS.
COMPETING INTEREST:
The authors have no competing interest.
AUTHORS’ CONTRIBUTION:
KJ: Conception and analysis of the study data and performed the statistical analysis.
SA: Critically revising work for important intellectual content.
MD: Substantial contribution to the conception and design of the work.
MS: Acquisition and interpretation of the data for the work.
All authors reviewed the draft critically for final publication.
REFERENCES
- Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PloS One 2017; 12(8):e0181960. doi: 10.1371/journal.pone.018 1960.
- Tesfay A, Gebremariam A, Gerbaba M, Abrha H. Gender differences in health-related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle Town, Northern Ethiopia. BioMed Res Int 2015; 2015:1-9. doi: 10.1155/2015/516369.
- Global HIV & AIDS statistics — Fact sheet [Internet]. Unaids.org. 2021 [cited 11 June 2021]. Available from: https:// www.unaids.org/en/resources/fact-sheet.
- Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention Atlanta, GA: Centers for Disease Control and Prevention. Available from: http://www. cdc.gov/hiv/prevention/research/compendium/rr/complete.html.
- Obadeji A, Ogunlesi AO, Adebowale TO. Prevalence and predictors of depression in people living with HIV/AIDS attending an outpatient clinic in Nigeria. Iran J Psychiatry Behav Sci 2014; 8(1):26-31.
- Hanass-Hancock J, Myezwa H, Carpenter B. Disability and living with HIV: baseline from a cohort of people on long term ART in South Africa. PloS One 2015; 10(12): e0143936. doi:10.1371/journal.pone.0143936.
- Felker-Kantor EA, Wallace ME, Madkour AS, Duncan DT, Andrinopoulos K, Theall K. HIV stigma, mental health, and alcohol use disorders among people living with HIV/AIDS in New Orleans. J Urban Health 2019; 96(6):878-88. doi: 10. 1007/s11524-019-00390-0.
- Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. A systematic review is the impact of alcohol use and related disorders on the HIV continuum of care. Curr HIV/AIDS Rep 2015; 12(4):421-36. doi: 10.1007/ s11904-015-0285-5.
- Hochstatter KR, Akhtar WZ, Dietz S, Pe-Romashko K, Gustafson DH, Shah DV, et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: Experience from a pilot mHealth intervention. AIDS Behav 2021; 25(2):354-9. doi: 10.1007/s10461-020-02976-1.
- Prado G, Pantin H. Reducing substance use and HIV health disparities among Hispanic youth in the USA: The Familias Unidas research program. Psychosoc Interv 2011; 20(1): 63-73. doi: 10.5093/in2011v20n1a6.
- Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst rev 2021; 10(1):1-9. doi:10.1186/s13643- 020-01542-z.
- Kalichman SC, Heckman T, Kochman A, Sikkema K, Bergholte J. Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psych Serv 2000; 51(7):903-7. doi : 10.1176/appi.ps.51.7.903.
- Passik SD, Kirsh KL, McDonald MV, Ahn S, Russak SM, Martin L, et al. A pilot survey of aberrant drug-taking attitudes and behaviours in cancer and AIDS patients samples. J Pain Symptom Manage 2000; 19(4):274-86. doi: 10.1016/s0885- 3924(00)00119-6.
- Catz SL, Gore-Felton C, McClure JB. Psychological distress among minority and low-income women living with HIV. J Behav Med 2002; 28(2):53-60. doi: 10.1080/08964280 209596398.
- Gritz ER, Vidrine DJ, Lazev AB, Amick BC, Arduino RC. Smoking behaviour in a low-income multiethnic HIV/AIDS population. Nicotine Tob Res 2004; 6(1):71-7. doi: 10.1080/ 14622200310001656885.
- Milam JE. Posttraumatic growth among HIV/AIDS patients. J Appl Soc. Psychol 2004;34(11):2353-76. doi:10.1111/j. 1559-1816.2004.tb01981.x.
- Krupitsky EM, Horton NJ, Williams EC, Lioznov D, Kuznetsova M, Zvartau E, Samet JH. Alcohol use and HIV risk behaviours among HIV-infected hospitalised patients in St. Petersburg, Russia. Drug Alcohol Depend 2005;79(2):251-6. doi: 10.1016/j.drugalcdep.2005.01.015.
- Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS 2006;20(12):1571. DOI: 10.1097/01.aids.0000238402. 70379.d4.
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: A systematic review of empirical findings. Prev. Sci 2007; 8(2):141-51.doi: 10.1007/s11121-006-0061-2.
- Brandt R. The mental health of people living with HIV/AIDS in Africa: A systematic review. Afr J AIDS Res 2009; 8(2):123-33. doi: 10.2989/AJAR.2009.8.2.1.853.
- Sherr L, Clucas C, Harding R, Sibley E, Catalan J. HIV, and depression-a systematic review of interventions. Psychol Health Med 2011; 16(5):493-527. doi:10.1080/13548 506.2011.579990.
- Brown T, Morgan KA. Psychological distress and substance abuse in Jamaican youths living with HIV/AIDS. West Indian Med J 2013; 62(4):341-45. doi: 10.7727/wimj.2013.024.
- Schadé A, van Grootheest G, Smit JH. HIV-infected mental health patients: characteristics and comparison with HIV-infected patients from the general population and non-infected mental health patients. BMC Psychiatry 2013; 13(1):1-10. doi:10.1186/1471-244X-13-35.
- Scott-Sheldon LA, Carey MP, Carey KB, Cain D, Vermaak R, Mthembu J, et al. Does life stress mediate the association between HIV status and alcohol use? Evidence from adults living in Cape Town, South Africa. AIDS Care 2013; 25(8):1026-32. doi: 10.1080/09540121.2012.749335.
- Chibanda D, Benjamin L, Weiss HA, Abas M. Mental, neurological, and substance use disorders in people living with HIV/AIDS in low-and middle-income countries. J Acquir Immune Defic Syndr 2014; 67:S54-67. doi: 10.1097/QAI. 0000000000000258.
- Uebelacker LA, Weisberg RB, Herman DS, Bailey GL, Pinkston-Camp MM, Stein MD. Chronic pain in HIV-infected patients: Relationship to depression, substance use, and mental health and pain treatment. Pain med 2015; 16(10):1870-81. doi: 10.1111/pme.12799.
- Secor AM, Wahome E, Michelini M, Rao D, Simoni JM, Sanders EJ et al. Depression, substance abuse and stigma among men who have gender with men in coastal Kenya. AIDS 2015; 29(3):S251-9. doi: 10.1097/QAD.000000000 0000846.
- Zhang C, Li X, Liu Y, Qiao S, Zhou Y, Shen Z, Chen Y. Substance use and psycho-social status among people living with HIV/AIDS who encountered HIV stigma in China: Stratified analyses by socioeconomic status. PLoS One 2016; 11(11):e0165624. doi: 10.1371/journal.pone.016 5624.
- Quinn K, Voisin DR, Bouris A, Schneider J. Psychological distress, drug use, sexual risks and medication adherence among young HIV-positive Black men who have gender with men: Exposure to community violence matters. AIDS Care 2016; 28(7):866-72. doi: 10.1080/09540121.2016.1153596.
- Egbe CO, Dakum PS, Ekong E, Kohrt BA, Minto JG, Ticao CJ. Depression, suicidality, and alcohol use disorder among people living with HIV/AIDS in Nigeria. BMC Public Health 2017; 17(1):542. doi: 10.1186/s12889-017-4467-5.
- Cichowitz C, Maraba N, Hamilton R, Charalambous S, Hoffmann CJ. Depression and alcohol use disorder at antiretroviral therapy initiation led to disengagement from care in South Africa. PloS One 2017; 12(12):e0189820. doi: 10.1371/journal.pone.0189820.
- Mthembu JC, Mabaso ML, Khan G, Simbayi LC. Prevalence of psychological distress and its association with socio-demographic and HIV-risk factors in South Africa: Findings of the 2012 HIV prevalence, incidence and behavior survey. SSM-Popul Health 2017; 3:658-662. doi: 10.1016/j.ssmph.2017. 07.009.
- Cook JA, Burke-Miller JK, Steigman PJ, Schwartz RM, Hessol NA, Milam J, et al. Prevalence, comorbidity, and correlates of psychiatric and substance use disorders and associations with HIV risk behaviors in a multisite cohort of women living with HIV. AIDS Behav 2018; 22(10):3141-3154. doi: 10. 1007/s10461-018-2051-3.
- Bassey RB, Chapman SN, Pessu M, Jayam-Trouth A, Gondré-Lewis MC. Is the history of substance abuse correlated with neuropsychiatric disorders and co-morbid HIV infection? An urban population study. J Neurol Neurosci 2018; 9(2):1-12. doi: 10.21767/2171-6625.1000251.
- Glynn TR, Llabre MM, Lee JS, Bedoya CA, Pinkston MM, O'Cleirigh C et al. Pathways to Health: An examination of HIV-related stigma, life stressors, depression, and substance use. Int J Behav Med 2019; 26(3):286-296. doi: 10.1007/s12529-019-09786-3.
- Basha EA, Derseh BT, Haile YG, Tafere G. Factors affecting psychological distress among people living with HIV/AIDS at selected hospitals of north shewa zone, Amhara region, Ethiopia. AIDS Res Treat 2019; 2019:1-8. doi: 10.1155/ 2019/8329483.
- Bitty-Anderson AM, Gbeasor-Komlanvi FA, Johnson P, Sewu EK, Dagnra CA, Salou M et al. Prevalence and correlates of alcohol and tobacco use among key populations in Togo in 2017: A cross-sectional study. BMJ Open 2019; 9(11): e028934. doi: 10.1136/bmjopen-2019-028934.
- Singh NK, Kumar P, Srivastava M. Substance abuse and psychiatric disorders in HIV-positive patients: An insight into triple diagnosis. Int J Contemp Med Res 2020; 7(9):I15-I18.
- Tchankoni MK, Gbeasor-Komlanvi FA, Bitty-Anderson AM, Sewu EK, Zida-Compaore WI, Alioum A, et al. Prevalence and factors associated with psychological distress among key populations in Togo, 2017. PloS one 2020; 15(4): e0231726. doi:10.1371/journal.pone.0231726.
- Higueras CV, García MM, Domínguez-Rodríguez S, Sáez BR, Cuéllar-Flores I, García-Navarro C, et al. Prevalence of psychological symptoms and associated risk factors in a Spanish sample of HIV-positive youth compared to uninfected peers. An d Pediatr (Engl Ed) 2020; S1695- 4033(20)30489-6. doi: 10.1016/j.anpedi.2020.05.028.
- Moges NA, Adesina OA, Okunlola MA, Berhane Y, Akinyemi JO. Psychological distress and its correlates among newly diagnosed people living with HIV in Northwest ethiopia: Ordinal logistic regression analyses. Infec dis (Auckl) 2021; 14:1178633721994598. doi:10.1177/1178633721994598.
- Chander G, Himelhoch S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients. Drugs 2006; 66(6):769-89. doi: 10.2165/00003495-200666060-00004.
- Seid S, Abdu O, Mitiku M, Tamirat KS. Prevalence of depression and associated factors among HIV/AIDS patients attending antiretroviral therapy clinic at dessie referral hospital, South Wollo, Ethiopia. Int J Ment Health Syst 2020; 14:55. doi: 10.1186/s13033-020-00389-0.
- Mathai M, Obando A, Mutavi T, Kumar M. Undetected psychiatric morbidity among HIV/AIDS patients attending comprehensive care clinic (CCC) in Nairobi Kenya: Towards an integrated mental health care. Ann Gen psychiatry 2018; 17(1):1-7. doi: 10.1186/s12991-018-0179-1.
- Hartzler B, Dombrowski JC, Crane HM, Eron JJ, Geng EH, Mathews WC, et al. Prevalence and predictors of substance use disorders among HIV care enrollees in the United States. AIDS Behavior 2017; 21(4):1138-48. doi: 10.1007/ s10461-016-1584-6.
- Bhatta DN, Subedi A, Sharma N. Tobacco smoking and alcohol drinking among HIV infected people using antiretroviral therapy. Tob Induc Dis 2018; 16(2):1-10. 10. 18332/ tid/86716.
- Duko B, Ayalew M, Ayano G. The prevalence of alcohol use disorders among people living with HIV/AIDS: A systematic review and meta-analysis. Substance Abuse Treat Prev Policy 2019; 14(1):1-9. doi:10.1186/s13011-019-0240-3.
- Wang T, Fu H, Kaminga AC, Li Z, Guo G, Chen L, et al. Prevalence of depression or depressive symptoms among people living with HIV/AIDS in China: A systematic review and meta-analysis. BMC Psychiatry 2018; 18(1):1-4. doi: 10. 1186/s12888-018-1741-8.
- Prajapati RK, Shyam R, Rathee S. Depressive symptoms and suicidal ideation in people living with HIV/AIDS and their caregivers: A comparative study. Open J Psychiatr Allied Sci 2019; 10(2):159-62. doi: 10.5958/2394-2061.2019.000 36.3.
- Ayano G, Solomon M, Abraha M. A systematic review and meta-analysis of epidemiology of depression in people living with HIV in east Africa. BMC Psychiatry 2018; 18(1):1-3. doi:10.1186/s12888-018-1835-3.