Spontaneous Forniceal Rupture Identified by Point-of-care Ultrasound
By Ali Celik, Mehmet AltuntasAffiliations
doi: 10.29271/jcpsp.2022.10.1341ABSTRACT
Spontaneous forniceal rupture is one of the rarest diagnoses of abrupt onset abdominal pain. Moreover, urolithiasis is the most prevalent cause and coexistent condition. Delayed-phased Contrast-enhanced computed tomography scans or intravenous pyelograms are needed for an exact diagnosis in most circumstances. Herein, we report a case of a healthy middle-aged female who presented to the emergency department with flank and abdominal pain. The diagnosis of forniceal rupture was made by the emergency point of care ultrasound. To the best of our knowledge, this is one of the first cases of spontaneous forniceal rupture secondary to urolithiasis diagnosed by the physician-performed ultrasound before confirmation of the diagnosis with computed tomography. In conclusion, emergency physicians and surgeons should be aware of rare conditions like spontaneous forniceal rupture and its sonographic findings to make a rapid diagnosis of urine extravasation so that unwanted complications are avoided.
Key Words: Renal stone, Ultrasound, Forniceal rupture, Renal colic, Urinoma.
INTRODUCTION
Spontaneous forniceal rupture (SFR) is a rare cause of abrupt onset abdominal pain. Although, the correct understanding of SFR is unexplained, a rupture can occur due to external trauma, an obstruction by urolithiasis, tumours, pregnancy, or as an iatrogenic complication. Cases of SFR may be missed or diagnosed late as patients present with symptoms similar to urolithiasis or peritonitis, resulting in complications of peritonitis, severe perirenal abscess, and even renal scars.1 Diagnosis is made with contrast-enhanced computed tomography (CT). We present a case of SFR secondary to urolithiasis, identified with the point of care ultrasound (POCUS) done by an emergency medicine specialist.
CASE REPORT
An otherwise healthy 49-year female patient presented to the emergency department (ED) with acute flank pain (AFP) localised in the right lower quadrant that began one hour prior, accompanied by nausea and vomiting. Her pain had then progressed to the suprapubic region. She did not experience such pain before.
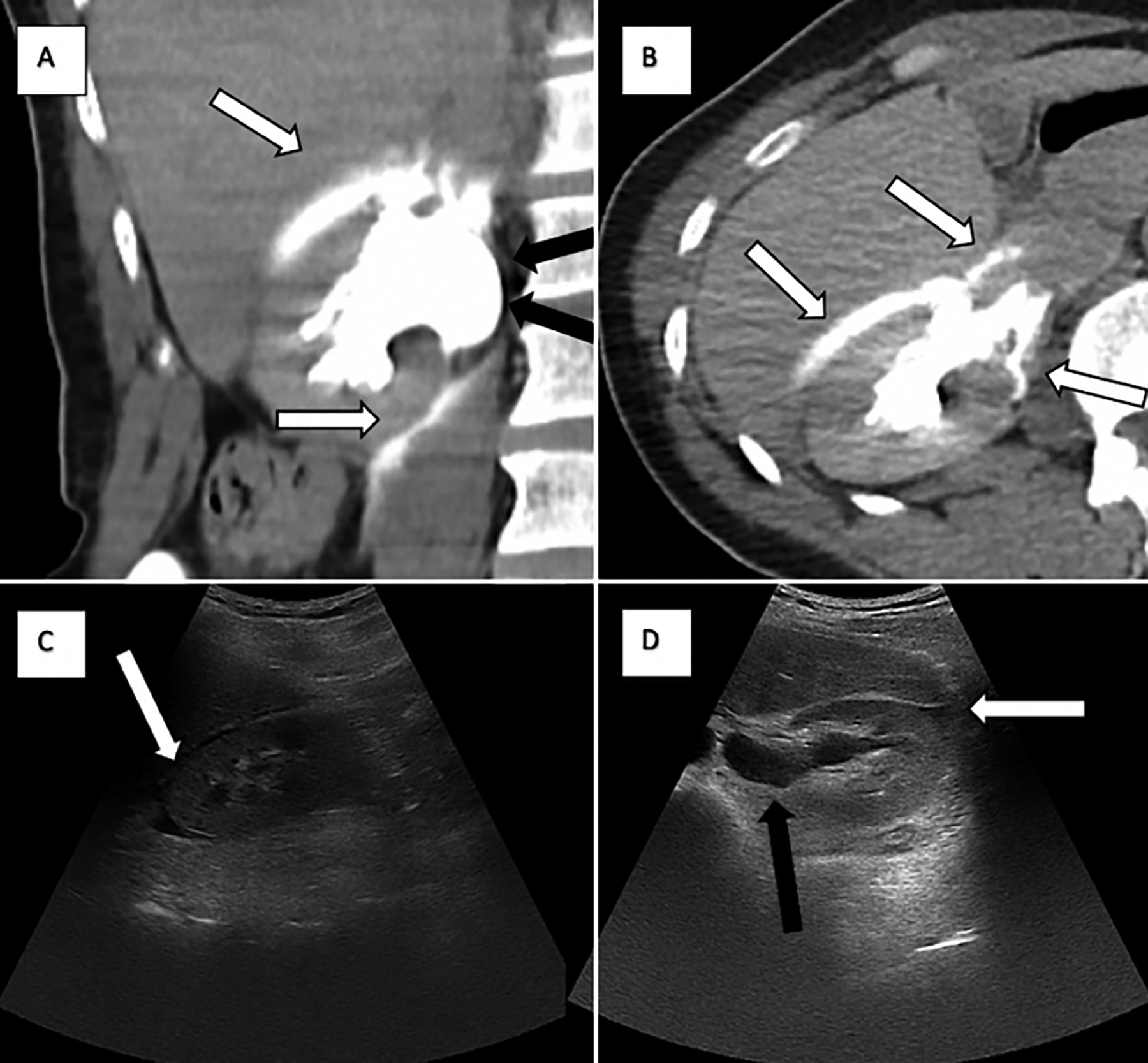 Figure 1: A and B: Pyelogram phase contrast-enhanced axial and coronal CT scans of the abdomen showing a collection of contrast medium at right upper perinephric region around the right psoas muscle compatible with forniceal rupture (white arrows) and a moderate dilatation of the urinary collecting system (black arrows). C and D: Point of care ultrasound images showing perinephric fluid collection (white arrows) and hydronephrosis (black arrows).
Figure 1: A and B: Pyelogram phase contrast-enhanced axial and coronal CT scans of the abdomen showing a collection of contrast medium at right upper perinephric region around the right psoas muscle compatible with forniceal rupture (white arrows) and a moderate dilatation of the urinary collecting system (black arrows). C and D: Point of care ultrasound images showing perinephric fluid collection (white arrows) and hydronephrosis (black arrows).
The blood pressure was 135/80 mmHg, heart rate was regular at 88 beats per minute, and her temperature was 37.2°C at admission. Physical examination was notable for right-sided costovertebral angle tenderness and rebound tenderness in right mid to lower abdominal quadrant. Antiemetic and analgesic agents were administered. Complete blood count, renal function tests, hepatic function tests, and C-reactive protein tests were unremarkable; however, midstream urinalysis revealed mild microscopic hematuria.
Simultaneously with primary evaluation and analgesic infusions, bedside sonographic evaluation was performed. POCUS examination revealed a 4 mm calculus detected in the right ureterovesical junction with moderate hydronephrosis and perinephric-periureteric fluid collection (Figure 1). To confirm the diagnosis of SFR, a delayed-phased contrast-enhanced CT examination was carried out. A collection of contrast medium at the right perinephric region through the right psoas muscle and a moderate dilatation of the urinary tract proximal to the stone were observed. Consequently, the diagnosis was verified as SFR secondary to ureterolithiasis (Figure 1).
The patient was referred to the urology clinic, discharged with tamsulosin and instructed to go to the urology clinic follow-up in two days. Eight days later, a spontaneous stone passage was observed. Furthermore, the patient was followed up conservatively, and after six weeks of follow-up, no hydronephrosis or free fluid collection was appreciated on ultrasound.
DISCUSSION
Spontaneous extravasation of urine is usually caused by disruption of the urinary collecting system at any level but mostly renal or caliceal fornix without any external trauma, ureteric instrumentation or extracorporeal shock wave lithotripsy. Urolithiasis is one of the most common causes of SFR. SFRs are mostly caused by sudden hydronephrosis resulting from tiny distal ureteric calculi. These result in many complications like electrolyte disorders, paralytic ileus, urinoma, abscess formation, peritonitis, sepsis, renal scars, and retroperitoneal fibrosis.1 Depending on the size of urinoma and localisation of extravasation, an open surgical intervention might be required. Usually, ureter stents, nephrostomy, percutaneous drainage of the collection, and infrequently nephrectomy due to massive scars are needed.2,3 Although, SFR cases usually need prolonged hospitalisations because of pain and complications, there are many cases in the literature with small stones that were conservatively followed up and discharged without any other intervention. In many reviews, it is reported that the optimal treatment of SFR is a dilemma because there are not enough randomised controlled prospective studies to support decision-making in these subjects.1,4 Morgan et al. stated that surgical treatment should be chosen considering the clinical status of patients and by the following criteria; 1) Signs of infection including leukocytosis, fever, or pyuria; 2) Renal function abnormalities; 3) Bilateral disease; 4) Recurrent nausea and emesis.4 Additionally, Morgan et al., reported that more than half of their 103 patients were followed up conservatively without any complications when these criteria were followed.4 Similarly, in the retrospective case series of Chen et al. 28% of cases were followed conservatively without any complications.5 Hence, in a very recent review, Harvey et al., reported that a conservative approach seems to be safe when patients are chosen carefully.6
In this case, there were no signs of infection or renal impairment. Besides, the patient had a small amount of extravasated urine with a tiny distal ureteric stone with potential for spontaneous passage. So, the patient was followed up conservatively successfully.
Pyelogram-phased contrast-enhanced abdominal CT scans are reference imaging modalities for the diagnosis of urine extravasation. Unfortunately, there are many concerns about using CT scans because of the high radiation dose, higher costs, and unavailability at all times. In the study of Metzler et al., the effects of using POCUS or CT on the management of patients were evaluated, and no significant difference was found.7 Finally, in 2014, the American College of Emergency Physicians (ACEP) suggested that ultrasound should be the first modality in young patients with renal colic.8 Also, The American College of Radiology (ACR) positioned ultrasound as “may be appropriate” for suspected stone disease in cases of AFP. Also, ultrasound is stated as “the first line test” for recurrent flank pain and pregnant patients with AFP.9
In the present case, we used POCUS at the same time as physical examination, and it showed us clues of urine extravasation before even analgesics were given to the patient. In the sonographic evaluation, hydronephrosis secondary to ureteric stone and the presence of perinephric and periureteric free fluid were demonstrated. If there is no other entity that explains these findings in patients with AFP, urine extravasation may be detected by POCUS in selected cases. Nevertheless, CT scans are essential for the establishment of diagnosis in most cases.
In conclusion, emergency physicians and surgeons should be aware of rare causes of abdominal pain including forniceal rupture and their sonographic clues in POCUS. Thus, rapid identification of urine extravasation can be made and also unwanted complications can be avoided.
PRIOR PUBLICATION:
This case report was presented at the Turkish Emergency Medicine Congress, November 21-24, Antalya, Turkey, 2019.
PATIENT’S CONSENT:
An informed consent document was signed by the patient and attached to the submission.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS‘ CONTRIBUTIONS:
AC, MA: Involved in the whole steps of the manuscript preparation process (the literature search, writing, and critical revision of the manuscript).
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Thom C, Eisenstat M, Moak J. Point-of-care ultrasound identifies urinoma complicating simple renal colic: A case series and literature review. J Emerg Med 2018; 55(1): 96-100. doi: 10.1016/j.jemermed.2018.02.033.
- Nadav G, Eyal K, Noam T, Yeruham K. Evaluation of the clinical significance of sonographic perinephric fluid in patients with renal colic. Am J Emerge Med 2019; 37(10): 1823-8. doi: 10.1016/j.ajem.2018.12.040.
- Sungur M, Caliskan S. High grade urothelial carcinoma of renal pelvis presenting as spontaneous urinoma. J Coll Physicians Surg Pak 2018; 28(6):S146-S7. doi: 10.29271/ jcpsp.2018.06.S146.
- Morgan TN, Bandari J, Shahait M, Averch T. Renal forniceal rupture: Is conservative management safe? Urology 2017; 109:51-4. doi: 10.1016/j.urology.2017.07.045.
- Chen GH, Hsiao PJ, Chang YH, Chen CC, Wu HC, Yang CR, et al. Spontaneous ureteral rupture and review of the literature. Am J Emerg Med 2014; 32(7):772-4. doi: 10. 1016/j.ajem.2014.03.034.
- Harvey N, Rudman H, Gall Z. Managing renal forniceal rupture secondary to ureteric calculi in line with the NICE renal and ureteric stone guidelines. J Clin Urology 2019; 0(0):2051415820961297.
- Metzler IS, Smith-Bindman R, Moghadassi M, Wang RC, Stoller ML, Chi T. Emergency department imaging modality effect on surgical management of nephrolithiasis: A multicenter, randomized clinical trial. J Urology 2017; 197 (3 Pt 1):710-4. doi: 10.1016/j.juro.2016.09.122.
- Sierzenski PR, Linton OW, Amis ES, Courtney DM, Larson PA, Mahesh M, et al. Applications of justification and optimisation in medical imaging: Examples of clinical guidance for computed tomography use in emergency medicine. Ann Emerg Med 2014; 63(1):25-32. doi: 10. 1016/j.annemergmed.2013.08.027.
- Coursey CA, Casalino DD, Remer EM, Arellano RS, Bishoff JT, Dighe M, et al. ACR appropriateness criteria® acute onset flank pain–suspicion of stone disease. Ultrasound Q 2012; 28(3):227-33. doi: 10.1097/RUQ.0b013e318262 5974.