Saved by the Clot in Superior Vena Cava Injury
By Pratikshya Thapaliya, Tanveer Ahmad, Nazish Sikander, Misauq Mazcuri, Ambreen AbidAffiliations
doi: 10.29271/jcpsp.2022.08.1083ABSTRACT
Penetrating neck injuries (PNIs) can cause injuries to great vessels. Superior vena cava (SVC) injury from a stab to the neck is rare and when it occurs, poses a significant risk of exsanguinating hemorrhage. We report a case of a 17-year female who survived a delayed presentation of five hours after sustaining stab injury to zone 1 of the neck. Her external wound was just above the medial 1/3rd of the clavicle which resulted in SVC laceration. Mechanism and site of injury along with clinical presentation with right hemothorax was highly suspicious for a vascular injury. Exsanguinating hemorrhage was halted by a soft clot in this hypotensive patient. Furthermore, permissive hypotension with judicious resuscitation stabilised the patient enough to undergo a contrast venogram to identify the level of SVC injury. The patient underwent successful surgical repair of SVC. This case illustrates the point that control of bleeding by soft clots does not rule out major vascular injury. Additionally, it demonstrates how permissive hypotension can be helpful as a damage control stepping stone in the management of these critical patients.
Key Words: Penetrating neck injury, Permissive hypotension, SVC laceration, Venorrhaphy.
INTRODUCTION
Isolated penetrating injury to the SVC is rare and lethal.1 SVC injury is mostly seen as a result of iatrogenic trauma during central venous catheterisation or placement of pacemakers.2 True incidence of SVC injury secondary to trauma has not been reported in the literature, as most of these cases succumb to the injury before reaching hospital or before diagnosis.2 Injury may occur in extra-pericardial or intra-pericardial portion of SVC. Depending upon the site, bleeding may occur in the pleural space, mediastinum, or the pericardial space.2 Often the level of external wound does not correlate with the internal injury in PNIs.3 Hence, the zonal approach to the management of these patients has been questioned.3 We report a case of an isolated injury to SVC secondary to penetrating neck trauma to zone 1 who survived delayed presentation of five hours.
CASE REPORT
A 17-year female presented after five hours of stab injury over the base of her neck. Her initial vitals recorded were blood pressure (BP) of 80/60 mmHg, pulse of 120 beats/min, respiratory rate of 28 breaths/min, and oxygen saturation of 86% on room air.
There was a single stab wound sized 2.5×1 cm at zone 1 of the neck just above the medial 1/3rd of the clavicle. No active bleeding was noted from the wound. There was reduced chest movement on the right side with dull percussion note and absent breath sounds.
Advanced trauma life support (ATLS)® protocol was started immediately and initially resuscitated accordingly. Needle thoracentesis was positive for hemothorax. The patient responded to initial resuscitation and BP was maintained at 90/60 mmHg.
The chest X-ray was done which showed opacified right hemithorax with contralateral mediastinal shift (Figure 1). Site of stab injury over the base of neck with clinical and radiological diagnosis of hemothorax was highly suspicious for vascular injury. Urgent contrast-enhanced CT chest demonstrated contrast extravasation near the brachiocephalic-caval junction (Figure 2). The decision to proceed with emergency thoracotomy was made and the patient was operated for 2 hours after presentation. Right posterolateral thoracotomy revealed clotted hemothorax and on removal of the soft clots, a gush of bleeding was noted from the extra-cardiac portion of SVC. Lateral venorraphy was done in a continuous method with polypropylene suture 5/0 (Figure 3). The patient was managed in a high dependency unit (HDU) for 1 day and then shifted to the ward. Postoperatively, no sign of SVC obstruction was noted. The patient was discharged on the 4th postoperative day after tube removal.
 Figure 1: Chest X-ray showing right hemothorax with contralateral mediastinal shift.
Figure 1: Chest X-ray showing right hemothorax with contralateral mediastinal shift.
 Figure 2: CT scan with contrast showing extravasation of contrast at the bracheocephalic-caval junction (Straight arrow).
Figure 2: CT scan with contrast showing extravasation of contrast at the bracheocephalic-caval junction (Straight arrow).
DISCUSSION
PNIs are observed in 10% of all the trauma patients with overall mortatlity rate of 3–6%.4 Mortality raises to 50% when there are associated vascular injuries in PNIs.4 Although the zonal approach was introduced in the management of PNIs, it is important to remember that often the level of external wound does not correlate with internal injury and this method has been questioned lately.3,4 The goal of successful trauma management is to identify whether any life-threatening condition exists and address it as early as possible. SVC is a low- pressure system but with a high-flow rate, therefore, its injury can cause colossal blood loss and can risk exsanguination.2 A minor laceration in the SVC in a hypotensive patient might permit a soft clot formation at the laceration site.1 This soft clot may prevent excessive bleeding from the vessel. During resuscitation, administration of excessive fluid before hemostasis risks additional blood loss via disruption of soft fibrin clot by raising intravascular pressure.5-7 Aggressive fluid therapy also causes dilution of clotting factors and hypothermia, which further predispose to bleeding.5-7 Permissive hypotension implies accepting a satisfactory but not aberrant blood pressure until hemostasis can be secured by surgery. It plays a vital role in the management of such injuries.5-7 Recommendations aim to titrate fluid resuscitation to sustain a systolic BP around 80–90 mmHg which maintains cerebral perfusion pressure.5,7 Depending upon the mechanism and site of injury along with clinical findings, we had a high suspicion of vascular injury in this case. Hence, we were careful not to carry out overzealeous fluid rescuscitation and keep the systolic BP below 100 mmHg until major vascular injury was ruled out. Our patient was responsive to resuscitation. We presume that a soft clot around SVC laceration in this patient prevented exsanguination. Permissive hypotension proved to be lifesaving in this case. A hemodynamically stable patient, whenever possible, should undergo CT with intravenous contrast as it can identify the location and define the grade of injury. This in turn aids in planning further management of the patient.8 Surgical exploration must always be the rule in patients with unstable condition. It was pertinent to know the exact site and origin of bleeding to decide about our approach and need for cardiopulmonary bypass (CPB) as our facility did not have cardiac surgery backup. CT venogram successfully identified the cause of bleed as from extra-cardiac portion of the SVC. This information permitted us to plan an urgent right thoracotomy without CPB need.
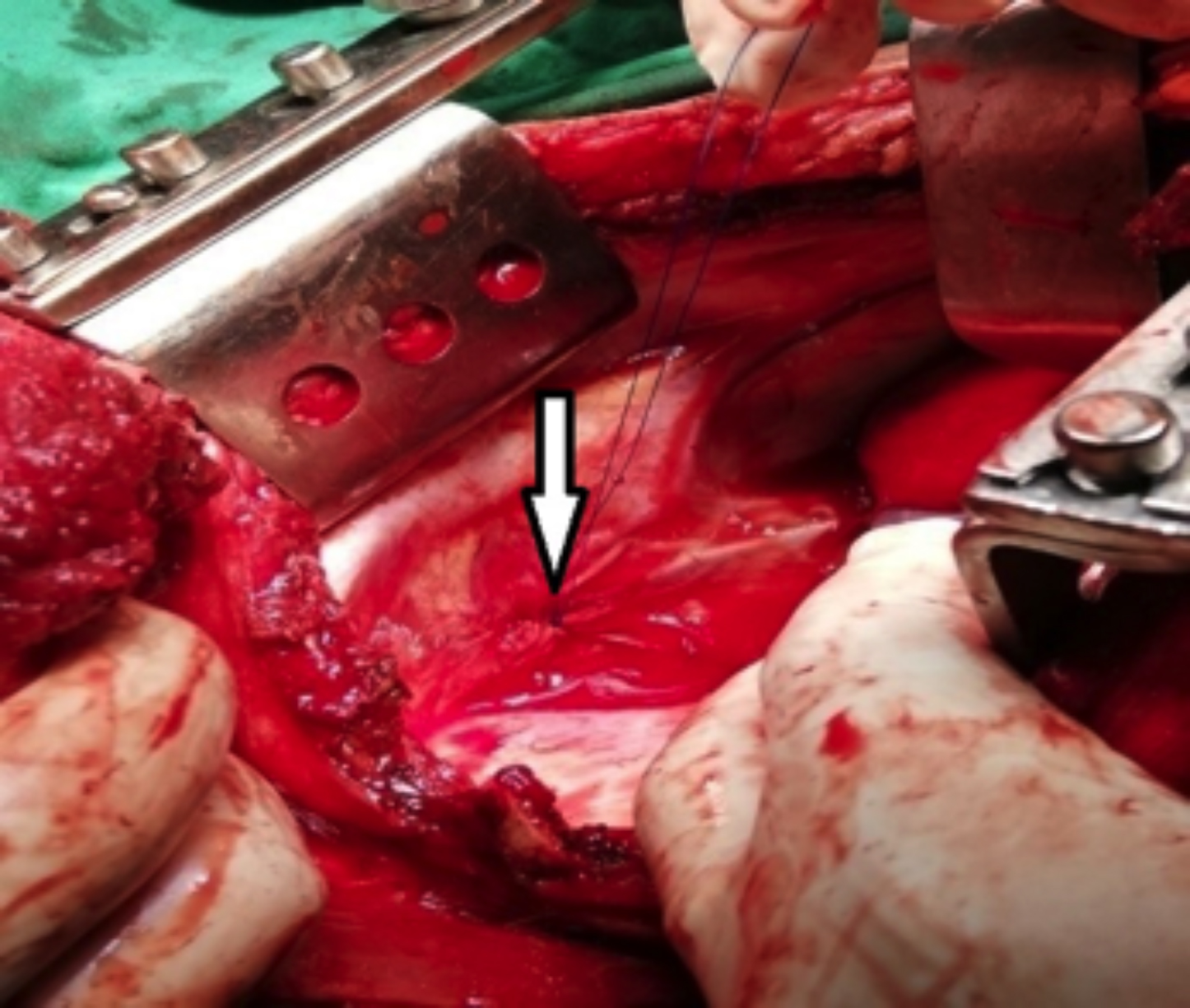 Figure 3: Lateral venorraphy of superior vena cava (SVC).
Figure 3: Lateral venorraphy of superior vena cava (SVC).
Most injuries can be repaired successfully by lateral venorrhaphy as in this case.1 During repair, care should be taken not to narrow the diameter of SVC to less than 50% as some surgeons suggest luminal narrowing leads to SVC syndrome.1 There was no sign of postoperative SVC obstruction in the present case. Repair of SVC injury can be performed without CPB except when injuries are in confluence with the heart.2,9 Sometimes initial cessation of hemorrhage might be misleading and hemodynamic status of the patient is the most important determinant in the management of patients with PNIs.
In conclusion, penetrating trauma to the base of the neck can lead to SVC injury. High clinical suspicion, early recognition, and application of basic trauma principles can save a life. Permissive hypotension is a life saver in hemothorax secondary to SVC laceration.
PATIENT’S CONSENT:
Informed and written consent was obtained from the patient for publication of this case report and accompanying images.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
PT: Designed the study, wrote the draft of the manuscript, and finalised the draft.
TA: Critically analysed the draft and approved the final version to be published.
NS: Managed literature search and drafting.
MM: Managed literature search, proofreading, and critical revision of the work.
AA: Literature search and drafting.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Topal A, Unal O, Akgul A. Importance of surgical exploration in the diagnosis of the penetrating superior vena cava injury in case of soft clot formation and unusual injury site: Case report. Turkiye Klinikleri J Cardiovasc Sci 2011; 23(2): 150-3.
- Taha A. Shrapnel superior vena cava injury: Case report. Case Rep Clin Med 2014; 03(02):85-8.
- Madsen A, Bruce J, Oosthuizen G, Bekker W, Smith M, Manchev V, et al. Correlation between the level of the external wound and the internal injury in penetrating neck injury does not favour an initial zonal management approach. BJS Open 2020; 4(4):704-13. doi: 10.1002/bjs5. 50282.
- Vesovic N, Ristanovic A, Cvijanovic V, Stojkovic D, Maric N, Kostovski V, et al. Penetrating neck injury with consequential thoracic complications managed with use of video-assisted thoracoscopic surgery: A case report. Vojnosanit Pregl 2020; 77(3):330-4.
- Nevin D, Brohi K. Permissive hypotension for active haemorrhage in trauma. Anaesthesia 2017; 72(12):1443-8. doi: 10.1111/anae.14034.
- Carrick M, Leonard J, Slone D, Mains C, Bar-Or D. Hypotensive resuscitation among trauma patients. Bio Med Res Int 2016; 2016:1-8.
- Geeraedts L, Kaasjager H, van Vugt A, Frölke J. Exsanguination in trauma: A review of diagnostics and treatment options. Injury 2009; 40(1):11-20. doi: 10. 1016/j.injury.2008.10.007.
- Haq A, Restrepo C, Lamus D, Ocazionez-Trujillo D, Vargas D. Thoracic venous injuries: An imaging and management overview. Emerg Radiol 2016; 23(3):291-301. doi: 10. 1007/s10140-016-1386-1.
- Ekim H. Management of penetrating superior caval vein injury. Pak J Med Sci 2009; 25(5):869-71.