Relationship between Migraine and Patent Foramen Ovale Observed by Contrast-enhanced Transthoracic Echocardiography
By Xuerong Fu, Mingxing LiAffiliations
doi: 10.29271/jcpsp.2023.03.352ABSTRACT
To observe the association between migraine and patent foramen ovale (PFO) using contrast-enhanced transthoracic echocardiography (cTTE). Eighty-five migraine with aura (MA) patients and 85 migraine without aura (MO) patients from January 2020 to February 2022 were divided into group A and group B, respectively. Sixty-five healthy people were included in normal control group. Difference of PFO positive rate among group A, group B, and normal control group was significant (p=0.002). Difference of PFO related right-to-left shunt (PFO-RLS), Grade 2 shunt, and Grade 3 shunt among group A, group B, and normal control group was significant (p=0.043 and p=0.013 respectively). PFO-RLS Grade 2 and 3 shunts may play an important role in MA patients and MO patients, and the size of PFO-RLS shunt may be associated with migraine.
Key Words: Migraine, Patent foramen ovale (PFO), Right-to-left shunt (RLS), Contrast-enhanced transthoracic echocardiography (cTTE).
Migraine is a recurrent throbbing headache disorder on one or both sides.1 Patent foramen ovale (PFO) is a congenital developmental defect of the atrial septum.2 Transesophageal echocardiography is a "gold standard" for the diagnosis of PFO, but it belongs to a semi-invasive test that is painful for patients during the procedure. Contrast-enhanced transthoracic echocardiography (cTTE) can be performed by imaging the right heart with Valsalva maneuver to look for the presence of a PFO.3 At present, there are few research reports on the use of cTTE to evaluate the association between migraine and PFO. So, the authors want to observe the association between migraine and PFO using cTTE.
This analytical study was conducted in the Affiliated Hospital of Southwest Medical University, China, from January 2020 to February 2022. G*Power software was used to calculate the sample. Eighty-five migraine with aura (MA) patients were selected as group A, and 85 migraine without aura (MO) patients were selected as group B. Sixty-five healthy people were included in the normal control group.
Inclusion criteria for group A and group B those patients who met the diagnostic criteria of MA or MO in the International Classification of Headache Disorders, 3rd edition by the International Headache Society (IHS) in 2013; without a history of substance abuse or prophylactic medication use; no contraindication to right heart acoustic imaging. Exclusion criteria for group A and group B were those patients with other medical and psychosomatic diseases, with the history of cardiovascular and cerebrovascular diseases, and those who were unable to cooperate with the completion of cTTE.
The inclusion criteria for the normal control group were those healthy individuals matched for age and gender in group A and group B, with no history of MA or MO.
The aura that occurred in group A was all visual aura. cTTE was performed in patient of group A, group B, and normal control group. The patient was instructed to practice the standard Vasalva maneuver before examination and lie in a 45° left lateral position, connected with the II-lead electrocardiograph during the examination. The apical four-chamber view and two-atrium view of the patient were routinely observed. After that, the patient was instructed to perform standard Vasalva action. After inhaling, the patient held his breath for several seconds or coughed forcefully to increase the filling volume of the right atrium. After the conventional two-dimensional and colour Doppler ultrasound examination was completed, the patient maintained the same position to establish elbow vein access (upper left extremity). Hand-vibrated physiological sodium chloride solution (contrast agent) was injected, and microbubble signal could be displayed and identified on the screen.4
PFO related right-to-left shunt (PFO-RLS) were graded that 1-10 microbubbles/frame as a small PFO-RLS shunt (Grade 1, Figure 1a), 11-30 microbubbles/frame as a medium PFO-RLS shunt (Grade 2, Figure 1b), and >30 microbubbles/frame as a large PFO-RLS shunt (Grade 3, Figure 1c).
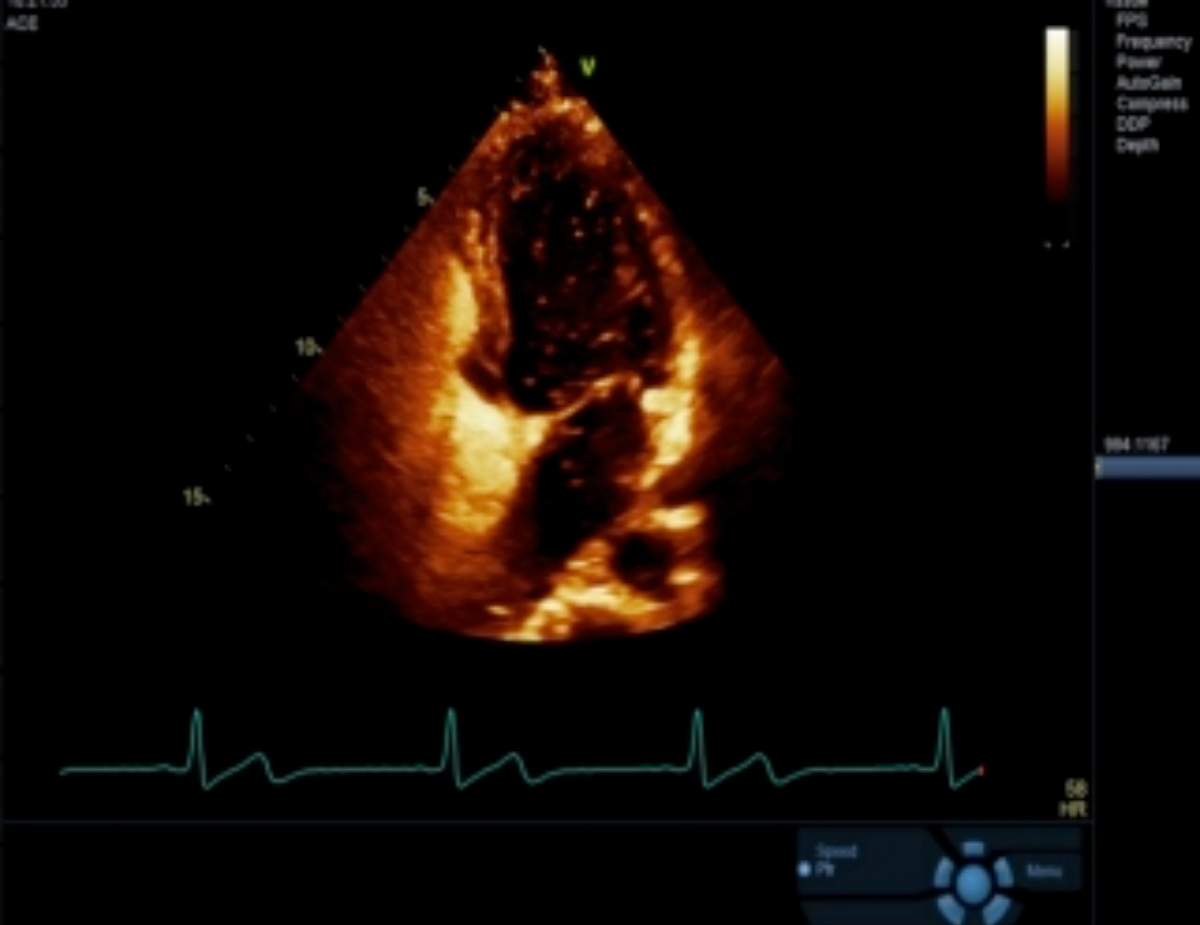 Figure 1-a: cTTE examination showed PFO-RLS Grade 1 shunt.
Figure 1-a: cTTE examination showed PFO-RLS Grade 1 shunt.
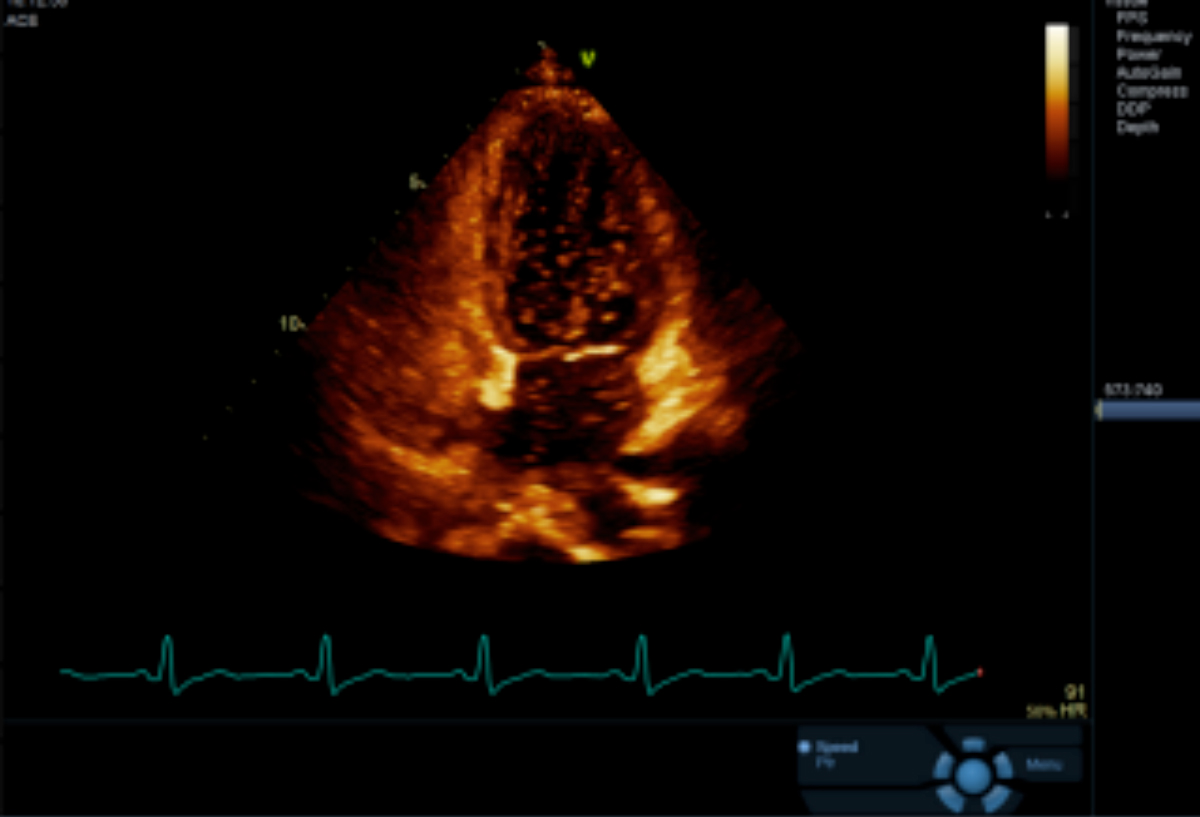 Figure 1-b: cTTE examination showed PFO-RLS Grade 2 shunt
Figure 1-b: cTTE examination showed PFO-RLS Grade 2 shunt
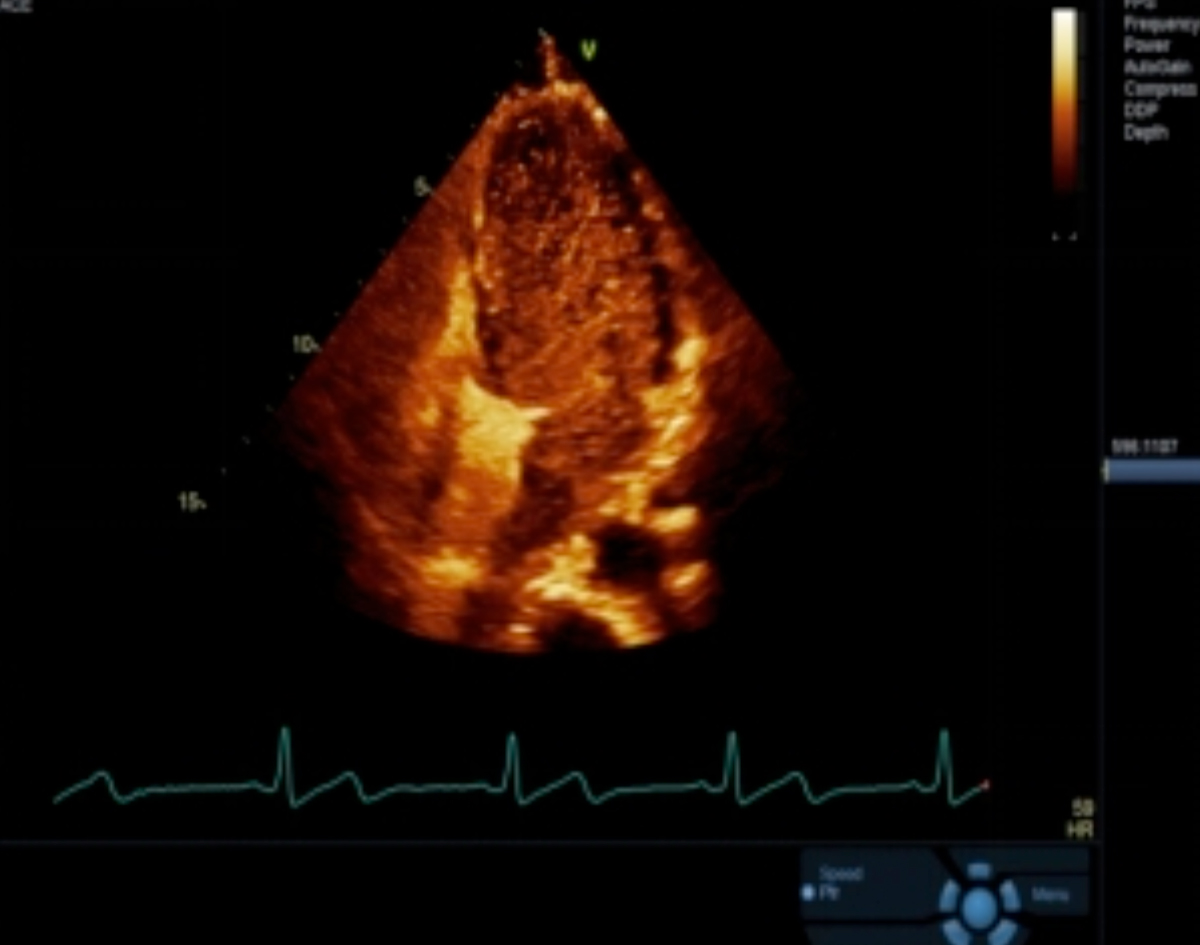 Figure 1-c: cTTE examination showed PFO-RLS Grade 3 shunt.
Figure 1-c: cTTE examination showed PFO-RLS Grade 3 shunt.
Table I: Results of cTTE examination.
|
Parameter |
Group A (n=85) |
Group B (n=85) |
Normal control group (n=65) |
p-value |
|
PFO positive rate [n (%)] |
34(40.00)ab |
29(34.12)c |
9(13.85) |
0.002 |
|
PFO-RLS Grade 1 shunt [n (%)] |
12(14.12)de |
11(12.94)f |
7(10.77) |
0.829 |
|
PFO-RLS Grade 2 shunt [n (%)] |
13(15.29)gh |
12(14.12)i |
2(3.08) |
0.043 |
|
PFO-RLS Grade 3 shunt [n (%)] |
9(10.59)jk |
6(7.06)l |
0(0) |
0.013∆ |
|
a Group A vs. group B, P=0.427; b group A vs. normal control group, P<0.001; c group B vs. normal control group, P=0.005; d group A vs. group B, P=0.823; e group A vs. normal control group, P=0.541; f group B vs. normal control group, P=0.685; g group A vs. group B, P=0.829;h group A vs. normal control group, P=0.013; i group B vs. normal control group, P=0.021; j group A vs. group B, P=0.417; k group A vs. normal control group, P=0.005; l group B vs. normal control group, P=0.036; ∆: Fisher's Exact test. |
||||
SPSS 25 was used to process data. Measurement data were shown by mean ± standard deviation. Count data were summarised as n (%), and chi-square test or Fisher's exact test was used. A value of p<0.05 was considered as significant.
In group A, there were 85 participants consisting of 35 (41.18%) men and 50 (58.82%) were women. Participants were aged 33.81±4.16 years.
In group B, there were 85 participants consisting of 34 (40.00%) men and 51 (60.00%) women. Participants were aged 32.82 ±4.17 years.
In the normal control group, there were 65 participants consisting of 27 (41.54%) men and 38 (58.46%) were women. Participants were aged 33.12±4.00 years.
The difference of PFO positive rate among group A, group B and normal control group was significant (p=0.002, Table I). Among them, the PFO positive rate of group A and group B was higher than that of normal control group (p<0.001 and p=0.005, respectively, Table I), while the difference of PFO positive rate between group A and group B was not significant (p=0.427, Table I).
There was no difference in the PFO-RLS Grade 1 shunt among group A, group B and normal control group (p=0.829, Table I). Among them, there was no difference in PFO-RLS Grade 1 shunt between group A and normal control group (p=0.541, Table I), there was no difference in PFO-RLS Grade 1 shunt between group B and normal control group (p=0.685, Table I), and there was no difference in PFO-RLS Grade 1 shunt between group A and group B (p=0.823, Table I).
Difference of PFO-RLS Grade 2 shunt among group A, group B and normal control group was significant (p=0.043, Table I). Among them, the difference of PFO-RLS Grade 2 shunt between group A and group B was higher than that of normal control group (p=0.013 and p=0.021, respectively, Table I), and the difference of PFO-RLS Grade 2 shunt between group A and group B was not significant (p=0.829, Table I).
Difference of PFO-RLS Grade 3 shunt among group A, group B, and the normal control group was significant (p=0.013, Table I). Among them, the difference of PFO-RLS Grade 3 shunt between group A and group B was higher than that of the normal control group (p=0.005, p=0.036, Table I), and the difference of PFO-RLS Grade 3 shunt between group A and group B was not significant (p=0.417, Table I).
RLS is mainly associated with PFO.5 The authors found that MA patients and MO patients had more PFOs than the healthy population, with significantly more PFO-RLS Grade 2 and 3 shunts. There was no difference in PFO positive rate between MA patients and MO patients. The findings of this study are generally consistent with previous study.6
The authors speculated that PFO-RLS Grade 2 and 3 shunts may play an important role in MA patients and MO patients, and the size of PFO-RLS shunt may be associated with migraine. Limitations of this study sample size was small and cTTE was not compared with other screening methods. The findings of this study need to be confirmed by further studies.
ETHICAL APPROVAL:
This study was approved by the ethics committee of the hospital.
PATIENTS’ CONSENT:
Informed consents were obtained from the patients.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
XF: Concept, design, data collection, and writing.
ML: Critical review and supervision.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Shao Q, Rascati KL, Barner JC, Lawson KA, Sonawane KB, Rousseau JF. Healthcare utilization and costs among patients with chronic migraine, episodic migraine, and tension‐type headache enrolled in commercial insurance plans. Headache 2022; 62(2):1-13. doi:10.1111/head. 14324.
- Vallance JK, Hale I, Hansen G. Commentary: Physical activity after patent foramen ovale (PFO)-associated stroke: A personal narrative and call to action. Top Stroke Rehabil 2022; 1-5. doi: 10.1080/10749357.2021.2021729.
- Kataoka A, Kito K, Sajima T, Watanabe Y, Kozuma K.Party balloon inflation maneuver during saline contrast trans-thoracic echocardiography to detect patent foramen ovale. JACC Case Rep 2022; 4(2):102-4.doi: 10.1016/j.jaccas. 2021.10.012
- Wu T, Hu Q, Zhang K, Xie S, Zhu J, Tang J. Value of real-time right heart sonography in the diagnosis of migraine with oval foramen. Clin Med 2020; 40(12)7-8. doi: 10.19528 /j.issn.1003-3548.2020.12.003.
- Tang Y, Peng A, Peng B, He S, Zhao X, Zhu Y, et al. Association between patent foramen ovale and migraine without aura: A community-based cross-sectional study in China. BMJ Open 2022; 12(3):e056937-43. doi:10.1136/ bmjopen-2021-056937
- Zhou Z, Yu S, Wang G, LiuX, Wang F, LiuR. Migraine and patent foramen Ovale: A contrast transcranial doppler study. Chin J Clin Neurosci 2008; 16(4):380-3. doi:10.3969/ j.issn.1008-0678.2008.04.009.