Perfusion Index Value in Determining the Success of Axillary Block
By Nurgul Cetgen1, Dilek Ener2, Mevlut Dogukan1, Mehmet Duran1, Oznur Uludag1Affiliations
doi: 10.29271/jcpsp.2022.09.1105ABSTRACT
Objective: To evaluate whether the perfusion index (PI) can be used to predict and provide a cut-off value for ultrasound-guided axillary nerve block success.
Study Design: Quasi-experimental study.
Place and Duration of Study: Department of Anaesthesiology and Reanimation, Adiyaman University Training and Research Hospital, Adiyaman, Turkey, from July to August 2020.
Methodology: Fifty patients between the ages of 18 and 65 years, who were in the ASA 1-2 group, undergoing hand, wrist and forearm surgery, were included in the study. PI value was measured from the extremity to the block and the healthy extremity before and after the procedure. Sensory block was evaluated with the pin-prick test, Motor block was evaluated with the Modified Bromage Scale. The minutes when sensory and motor blocks occurred were recorded, and the PI value at these moments were recorded.
Results: Pin-prick test was positive in patients at average 8.4±2.4 minutes. The average PI value for which the pin-prick test was positive was 7.41±2.54, and the cut-off value of the sensory block PI ratio was determined as 1.7 times. The modified Bromage scale reached a score of 2 in 7.6±2.3 minutes on average. The average PI value is 7.27±2.69 for which the modified Bromage Scale score is 2. At modified Bromage Scale-2, PI ratio cut-off value was determined as 1.7 times. The modified Bromage Scale reached a score of 3 in an average of 12.6±4.2 minutes. The mean PI value for the modified Bromage Scale score of 3 is 9.56±6.97. The motor block PI ratio cut-off value was determined as 1.9 times.
Conclusion: Pulse oximetry perfusion index is a sensitive and simple method that can be used to evaluate the success of axillary block. The cut-off value, indicating successful block for the rate of sensory block and modified Bromage scale PI, was determined as 1.7 times and the motor block PI ratio as 1.9 times.
Key Words: Axillary block, Perfusion index, Oximetry, Ultrasonography, Modified bromage scale.
INTRODUCTION
Axillary block is the most frequently applied block among the brachial plexus blocks. It is widely used in the forearm, wrist, and hand surgeries due to the superficial nature of the nerves in this region, ease of application, high-block success rate, and relatively low-risk of complications.1 The advantages of peripheral nerve blocks are that the patient is conscious, airway control is in the patient, and accordingly, the risk of aspiration of gastric contents is low which reduces the stress response that may occur due to the surgery and trauma, reduces the need for analgesia in the postoperative period, reduces the cost of administration, and shortens the hospital stay.1,2
It creates anaesthesia by temporarily making sensory, motor, and sympathetic blocks in dermatomes belonging to the nerve or nerve group to which the block is applied. Whether the block is effective or successful is decided by the sensory, motor, and sympathetic block levels.2 Routine methods, which evaluate sensory examination such as loss of hot-cold sensation and pin-prick test, require very good communication with the patient, and the evaluation of the results is subjective. After a successful block with these methods, increased blood flow and increased skin temperature, due to the local vasodilation as a result of sympathetic nerve blockade in the blocked area, were evaluated. However, these methods do not respond rapidly in terms of the clinical use in intensive operating room conditions and in the emergency cases where time is important.3-5
Photoplethysmography (PPG) has been extensively used for pulse oximetry monitoring the anaesthesia perioperatively in intensive care. The perfusion index (PI) is derived from PPG signal and represents the ratio of pulsatile on non-pulsatile light absorbance or reflectance of the PPG signal. The PI determinants are complex and interlinked, involving and reflecting the interaction between the peripheral and central haemodynamic characteristics, such as vascular tone and stroke volume.6 Recently, there have been various studies that shed light on the performance of this variable, especially evaluating the success of regional or neuraxial block. The perfusion index provides more quantitative information about peripheral circulation and gives an advantage in eliminating the deficiencies of other methods.7
The aim of the study was to determine the perfusion index (cut-off) values to indicate successful axillary nerve blocks performed under ultrasonography (USG) guidance.
METHODOLOGY
This study was conducted at the Department of Anaesthesiology and Reanimation, Faculty of Medicine, Adıyaman University Training and Research Hospital, between July and August 2020, following the approval of the Ethical Committee (No. 18/05/2020; 05/24) and after obtaining written informed consent from the patients. The study included a total of 50 patients between 18 and 65 years of age with an American Society of Anaesthesiologists (ASA) status of I-II, who underwent an axillary block due to the elective hand, wrist, and forearm surgery operations. Patients with a neurological deficit and peripheral artery disease, mental retardation, alcohol or drug abuse, allergy to local anaesthetic agent, morbid obesity, coagulopathy, chronic analgesic therapy, diabetes mellitus, those who were pregnant, and those with contraindications to axillary block, were excluded from the study. The demographic characteristics (age, height, weight, and gender) and ASA risk groups of the patients were recorded.
Prior to the blockage, electrocardiographic data (ECG), heart rate (HR), respiratory rate (RR), non-invasive blood pressure (from the contralateral arm) (BP), and peripheral oxygen saturation (SpO2) were monitored. The vascular access was established from the contralateral arm using a 20-gauge intracath, and a crystalloid infusion at 10 mL/Kg/h was begun. The patients were administered 0.01 mg/Kg of intravenous (IV) midazolam (Zolamid 5 mg/5 mL, Defarma, Turkey) and 1 µg/Kg of fentanyl (Talinat 0.5 mg/10 mL, Vem Ilac, Cerkezkoy, Turkey). All the patients underwent blockage and received 2-4 L/minutes of oxygen through a face mask throughout the operation. To measure the perfusion index (PI), a pulse oximeter sensor (RZ-25 adult sensors Masimo SET® Radical™ pulse oximeters; Masimo Corp, Irvine, CA USA) was attached to the arm to be blocked and then to the other arm. This was also connected to the Rad-7™ Pulse CO-oximeter device.
Following the baseline data recording, the axillary block procedure was begun. While the patient was lying in the supine position, their heads were turned to the opposite side of the side to be blocked. The arm to be blocked was brought to abduction and external rotation; the forearm to flexion and supination. For the block procedure, the patient's head was moved. The area to be injected was cleaned with povidone-iodine. Before the block, the gel was applied on the linear probe of the Siemens’ brand USG device and covered with a sterile nylon sheath. After the block area was covered, sterile local anaesthesia was performed with 1 cc 2% lidocaine (Jetmonal 2%, 20mg/ml, Adeka, Turkey). An in-plane image was obtained with USG by applying sterile gel to the area to be treated. Then, the motor response of the terminal branches of the brachial plexus (median, ulnar, radial, and musculocutaneous) with a 22G 50 mm needle isolated against electrical leakage using a neurostimulator (StimuplexDig®, B-Braun, Germany), together with the ultrasound device is 0.2-0.8 was evaluated by giving mA electrical stimulation. Extension of the fingers or wrist was evaluated as the adequate response for the radial nerve, flexion of the second and third fingers for the median nerve, flexion of the fourth and fifth fingers or adduction of the fist for the ulnar nerve, and flexion of the forearm for the musculocutaneous nerve. After these terminal branches of the brachial plexus were identified, a separate injection of local anaesthesia was performed with a needle perpendicular to the ultrasound probe.
The injections were administered by performing a negative aspiration test. For the block, 20 ml 0.5% bupivacaine (Buvicaine 0.5%, 5 mg/ml Polifarma) and 10 ml lidocaine were prepared separately. A total of 30 ml (20 ml bupivacaine+10 ml lidocaine) local anaesthesia was used in all the patients.
The peripheral oxygen saturation, heart rate, non-invasive arterial pressure, and PI values measured from both extremities were recorded at the 5th, 10th and 20th minutes, after the block application was completed.
Sensory blockade of each nerve was evaluated by pin-prick method in sensory dermatomes related to the sensory areas and graded as score 0 (no sensation), score 1 (dull sensation), and score 2 (sharp pain felt). Motor blockade was evaluated by using a modified Bromage scale as 3 (elbow flexion against gravity force), 2 (wrist flexion against gravity force), 1 (finger movement), and 0 (no motion).4 The PI values at the minutes and at this moment, when the pin-prick test was positive, were recorded. The modified Bromage scale and the PI values at the minute the score was 2 and 3 and at this time were recorded. The patient was given surgery after 20 minutes of observation. Intraoperative HR, SpO2, diastolic arterial pressure (DAP) and systolic arterial pressure (SAB) values of the patients were recorded. The surgical time was recorded.
The data were analysed using the SPSS 21.0 program. The G*Power (v3.1.9) program was used to determine the number of samples. The effect size was calculated as 0.8 based on the mean value of perfusion indices obtained from a previous study. When the power of the study was 95%, the effect size was 0.8, and α error was 0.05, it was calculated that at least 20 patients should be included in the sample. However, 50 patients were included in the study group because the minimum sample size required to perform ROC analysis was 50.8,9 Counts, percentages (%), mean, and standard deviation (SD) values were used for descriptive statistics. Descriptive data were patients' age, gender, BMI, smoking status, ASA scores, duration of the surgery, surgery scores, systolic arterial pressures, diastolic arterial pressures, heart rate, and peripheral oxygen saturation. The quantitative data were determined to be suitable for normal distribution by the Shapiro-Wilk test, histograms and Q-Q plots. For normally distributed data the Unpaired t-test was performed on the independent groups. For non-normally distributed data repeated measures ANOVA test and Friedman’s test were used on the dependent groups. While the application of the block was taken as an independent variable. The Perfusion Index Rate (PI), which indicates the development of the block, was taken as the dependent variable. In the study, receiver operating characteristic (ROC) analysis was applied to determine the PI rate, sensitivity, and specificity values which indicate the development of the block. The p<0.05 value was considered statistically significant.
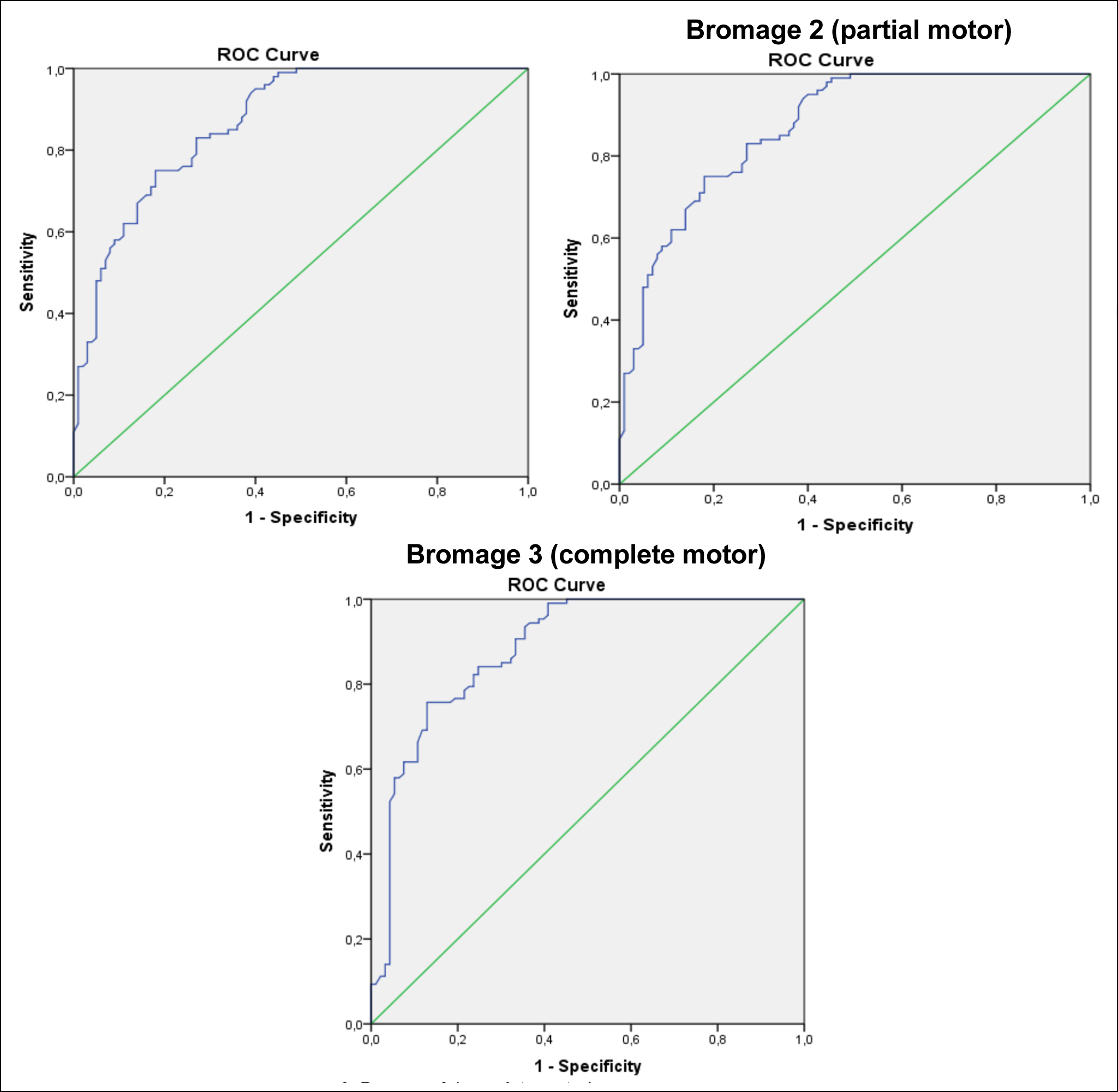 Figure 1: ROC curve of the sensory, partial motor, and complete motor blocks pin-prick test (sensory).
Figure 1: ROC curve of the sensory, partial motor, and complete motor blocks pin-prick test (sensory).
RESULTS
The mean age of the 50 patients included in the study was 40.6±15.5 years. Fifty six percent of the patients were in the 18-39 age group, 76% were males, and 36% were smokers. Sixty percent of the patients have an ASA score of 2, 40% have a score of 1. The mean body mass index is 26.01±3.70 Kg/m2, and 46% of the patients were in the obese group. The average operation time is 102.7 minutes.
The general mean intraoperative systolic arterial pressure of the patients was 128.04±15.21. The differences among the systolic arterial pressures were between 0th minute with 10th, 20th, 30th, and 60th minutes. The systolic arterial pressures were significantly lower compared to the 0th minute (Friedman's test; 43.75, p<0.001). The general mean diastolic arterial pressure of the patients during the operation was 73.56±10.20. There was a significant change in the diastolic arterial pressure during the operation. The differences among the diastolic arterial pressures were ranging as the 0th minute with 10th, 20th, 30th, and 60th minutes. The diastolic arterial pressures were significantly lower compared to the 0th minute (Friedman's test; 28.46, p<0.001). The general average heart rate of the patients during the surgery was 75.66±11.69. Heart rates were significantly lower compared to the 0th minute. Differences among heart rates were between 0th minute with 10th, 20th, 30th and 60th minutes; 10th minutes with 20th and 60th minutes. Heart rates decreased as time progressed (Repeated Measures Anova test; 17.69, p<0.001). The peripheral oxygen saturations were significantly higher compared to the 0th minute except for the 10th minute. Thirty minutes and 60th -minute peripheral oxygen saturations were significantly higher compared to the 10th minute. Peripheral oxygen saturation increased as time progressed (Friedman's test; 88.25, p<0.001).
There was no significant difference among the PI values measured from both extremities before the block. In the 5th, 10th and 20 minutes after the block, the mean PI in the blocked arm was significantly higher than in the non-blocked arm. In the non-blocked extremity; there was no statistically significant difference among the mean PI values before the block, at the 5th minute, at the 10th minutes and at the 20th minutes. In the blocked extremity, the PI averages at the 5, 10, and 20 minutes after the block were significantly higher than the mean PI before the block. The mean PI at the 10 and 20 minutes after the block was significantly higher than the mean of the 5 minutes PI.
The pin-prick test was positive in patients at an average of 8.4±2.4 minutes. The mean PI value for which the pin-prick test is positive is 7.41±2.54. The cut-off value of the PI ratio, which is intended to be used as an alternative to the pin-prick test in determining the development of sensory block with ROC analysis, was determined at a significant level. The modified Bromage scale reached a score of 2 on an average of 7.6±2.3 minutes. The mean PI value with a modified Bromage scale score of 2 is 7.27±2.69. The modified Bromage scale achieved a mean score of 3 at 12.6±4.2 minutes. The mean PI value with the modified Bromage scale score of 3 is 9.56±6.97. The cut-off value of the PI ratio to be used as an alternative to the modified Bromage scale in determining the development of complete motor block by ROC analysis was significantly found to be 1.86 (Table I).
The cut-off value for the rate of sensory block PI was determined as 1.7 times. The point at which the PI value was 1.7 times the basal PI value in the patient, indicated that the sensory block had developed. As an alternative to the pin-prick test, the formula-1.7 x basal PI value-can be used as a more objective method. A 70% increase in basal PI showed that sensory block had developed.
The cut-off value of the modified Bromage scale PI ratio was determined as 1.7 times. The modified Bromage scale becomes 2, when the PI value is 1.7 times the basal PI value in the patient. As an alternative to the modified Bromage scale, the formula-1.7 X basal PI value can be used as a more objective method. This formula is the threshold PI ratio for the both sensory and partial motor blocks. A 70% increase in basal PI indicated the development of the partial motor block.
Table I: The difference, among the 5, 10, and 20 minutes PI average before and after the block between the non-blocking and the blocking arm.|
PI Mean±SD |
Non-blocking Arm |
Blocking arm |
t* |
p |
|
Before block |
3.39±1.51 |
3.40±1.55 |
0.05 |
0.964 |
|
5-min. |
3.37±1.50 |
6.27±2.53 |
6.96 |
<0.001 |
|
10-min |
3.36±1.48 |
8.04±2.95 |
10.01 |
<0.001 |
|
20-min. |
3.35±1.47 |
8.98±3.10 |
11.59 |
<0.001 |
|
Overall mean |
3.37±1.48 |
6.67±3.35 |
|
|
|
|
F**: 0,85 p: 0.426 |
F**: 127.41, p: <0.001 |
|
|
|
* Unpaired t-test; **Repeated measures anova test. |
||||
Table II: PI ratio threshold values of the blocks and ROC analysis results.
|
|
Cut-off value |
Sensitivity |
Specificity |
Likelihood ratio |
Under curve area |
||
|
% |
95% CI |
p |
|||||
|
Sensory block |
1.7 |
83% |
73% |
3.07 |
87.0 |
82.2-91.7 |
<0.001 |
|
Partial motor block |
1.7 |
82% |
76% |
3.47 |
88.3 |
83.5-93.1 |
<0.001 |
|
Complete motor block |
1.9 |
75% |
71% |
2,61 |
80.8 |
74.8-86.8 |
<0.001 |
The cut-off value of the motor block PI ratio was determined as 1.9 times. The point at which the PI value was 1.9 times the basal PI value in the patient, indicated the development of the motor block. When the modified Bromage scale was 3, the formula-1.9 X basal PI value-could be used as an alternative to the evaluation showed that a complete motor block had developed. A 90% increase in basal PI indicated the development of the motor block (Table II, Figure 1).
DISCUSSION
PI is not a measurement of blood flow, but rather a measurement of its pulsatility.10 Each vasoconstrictor stimulation or activation of the sympathetic nervous system decreases PI, because the height of the pulsatile part of the curve decreases. In contrast, any vasodilator stimulus, parasympathetic activation or inhibition of the sympathetic nervous system increases PI, because the height of the pulsatile part of the curve increases. The role of PI in predicting the success of axillary nerve blocks has been evaluated in this study. Sympathetic block results in peripheral vasodilatation in the extremity and thus, an increase in PI. The cut-off values of the PI value indicating the formation of the axillary block were: pin-prick sensory block PI rate was 1.7 times; the modified Bromage scale-2 PI rate was 1.7 times; and the modified Bromage scale was 1.9 times for complete motor block PI rate. The sensitivity of the method was high, and the specificity was moderately high.
Block success was evaluated using PI in patients who underwent peripheral block. Galvin et al. evaluated the change in PI in the patients with an axillary and sciatic block, and concluded that PI was simple, early, objective, high-specificity, and high-sensitivity compared to the traditional methods in patients with axillary and sciatic blocks. In the same study, a 1.55-fold increase in PI compared to the baseline values, was evaluated as a successful block, and it was observed that these values were reached at the 10th minute in the axillary block and the 12th minute in the sciatic block.11
Kuş A et al., in their study examine the usefulness of the perfusion index in determining the effect of brachial plexus block, investigated whether the perfusion index, which is a measure of peripheral perfusion, is a reliable and objective method for evaluating the adequacy of the infraclavicular blockade. The mean PI and mean percent change in PI were calculated from the baseline 10, 20, and 30 minutes after administration of the block. At 10 minutes, PI increased by 120±119% from baseline. At 20 and 30 minutes, the perfusion index increased by 133±125% and 155±144% from baseline. The PI increased continuously during the 30-minute observation period. It was found that the greatest changes in PI occurred 30 minutes after block administration, but significant changes in PI occurred 10 minutes after administration. It has been reported that the perfusion index has been determined as an indicator of the success of infraclavicular block.7
Abdelnasser et al., in their study investigating whether the perfusion index can be used to predict and ensure the success of ultrasound-guided supraclavicular nerve block, found the PI useful for the evaluation of successful supraclavicular nerve block. They concluded that a PI ratio above 1.4 was a good predictor of block success.12
Eskin et al., applied supraclavicular, interscalene, and infraclavicular blockades in equal numbers to the 60 patients aged 18-60 years with an ASA score of I or II, who were undergoing upper extremity surgery, and observed PI values. Initially, PI values were measured non-invasively at the 10th, 20th, and 30th minutes and in the post-anaesthesia care unit. A statistically significant increase in PI values was detected in all the patients after a successful brachial plexus blockade. According to the first determined values, the mean rate of change in PI was found to be significantly higher in the interscalene group than in the supraclavicular and infraclavicular groups (p <0.001). It has been shown that PI application can be used as a non-invasive standard monitoring method in determining the success of brachial plexus blockade.13
Visual guidance provided by USG, which is increasingly used in regional anaesthesia practice, has enabled the visualisation of the needle site, drug distribution, and important anatomical neighbourhoods as well as nerve localisation.14 In the present study, the authors performed an axillary block with USG and peripheral nerve stimulator (PSS). With the use of USG, it is easier to find anatomical landmarks. As the practitioner gains experience in the use of USG, the success rate of the block increases, the onset time of the block is shortened, the side effects and the volume of local anaesthesia decrease. Thus, the quality of the block increases and the need for additional anaesthesia and analgesia decreases.15 The purpose of using USG in this study is direct visualisation of anatomical structures (tissue, vessels, muscles, and tendons) and the localisation of the nerve, direct visualisation of the spread of the local anaesthetic agent during injection, and an attempt to prevent accidental displacement of the needle through this imaging. In addition, it is to reduce the risk of toxicity by reducing the dose of local anaesthesia and to provide a longer and quality block.
In this study, stable intraoperative hemodynamics were observed. There were statistically significant differences among the systolic arterial pressure, diastolic arterial pressures, heart rates and peripheral oxygen saturation of the patients during the operation, and the general average of the patients' intraoperative systolic arterial pressure was 128.04±15.21 mmHg. The general average of the patients' intraoperative diastolic arterial pressure was 73.56±10.20 mmHg. The overall mean heart rate of the patients during the surgery was 75.66±11.69 beats/minutes. The general mean of peripheral oxygen saturation during the surgery was 98.55±1.89%. As the operation time progressed, while the mean heart rate was decreased, peripheral oxygen saturation was increased. The authors attributed this to the intraoperative oxygenation.
CONCLUSION
Pulse oximetry perfusion index is a sensitive and simple method that can be used to evaluate the success of axillary block. The cut-off value, indicating successful block for the rate of sensory block and modified Bromage scale PI, was determined as 1.7 times and the motor block PI ratio as 1.9 times.
ETHICAL APPROVAL:
The study was approved by the Institutional Ethics Committee of Adiyaman University (Date: 18.05.2020; No. 2020/5-24).
PATIENTS’ CONSENT:
Informed consent was obtained from all the patients/relatives before the study began.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’CONTRIBUTION:
NC: Conception, design, data acquisition, and manuscript drafting.
DE: Data analysis, interpretation, and statistical analysis.
MD, MD: Manuscript drafting and supervision.
OU: Critical revision of the manuscript and supervision.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Satapathy AR, Coventry DM. Axillary brachial plexus block. Anesthesiol Res Pract 2011; 2011:173796. doi: 10.1155/ 2011/173796.
- Ranganath A, Srinivasan KK, Iohom G. Ultrasound guided axillary brachial plexus block. Med Ultrason 2014; 16(3):246-51. doi: 10.11152/mu.2013. 2066.163.2kks.
- Kim D, Jeong JS, Park MJ, Ko JS. The effect of epinephrine on the perfusion index during ultrasound-guided supraclavicular brachial plexus block: A randomised controlled trial. Sci Rep 2020; 10(1):11585. doi: 10.1038/s41598-020-68475-4.
- Thakur A, Singh J, Kumar S, Rana S, Sood P, Verma V. Efficacy of dexmedetomidine in two different doses as an adjuvant to lignocaine in patients scheduled for surgeries under axillary block. J Clin Diagn Res 2017; 11(4):16-21. doi: 10.7860/JCDR/2017/23540.9678.
- Guzel A, Celik F, Uludag O, Dogan E, Alemdar C, Yildirım B. The usage of low dose lidocaine fentanyl in intravenous regional anaesthesia. J Int Dental Med Res 2013; 6(2): 96-9. https://dergipark.org.tr/en/pub/intdental/issue/8629/107766.
- Elshal MM, Hasanin AM, Mostafa M, Gamal RM. Plethysmographic peripheral perfusion index: Could it be a new vital sign? Front Med 2021; 8:651909. doi: 10.3389/fmed.2021. 651909.
- Kus A, Gurkan Y, Gormus SK, Solak M, Toker K. Usefulness of perfusion index to detect the effect of brachial plexus block. J Clin Monit Comput 2013; 27(3):325-8. doi: 10. 1007/s10877-013-9439-4.
- Unal I. Defining an optimal cut-point value in ROC analysis: An alternative approach. Comput Math Met Med 2017; 2017:1-14. doi.org/10.1155/2017/3762651.
- Kumar R, Indrayan A. Receiver operating characteristic (Roc) curve for medical researchers. Indian Pediatr 2011; 48(4):1-11. doi: 10.1007/s13312-011-0055-4.
- Bergek C, Zdolsek JH, Hahn R. Non-invasive blood haemoglobin and plethysmographic variability index during brachial plexus block. Br J Anaesth 2015; 114(5):812-7. doi: 10.1093/bja/aeu484.
- Galvin EM, Niehof S, Verbrugge SJ, Maissan I, Jahn A, Klein J, et al. Peripheral flow index is a reliable and early indicator of regional block success. Anesth Analg 2006; 103(1): 239-43. doi: 10.1213/01.ane.0000220947.02689.9f.
- Abdelnasser A, Abdelhamid B, Elsonbaty A, Hasanin A, Rady A. Predicting successful supraclavicular brachial plexus block using pulse oximeter perfusion index. Br J Anesth 2017; 119(2): 276-80.doi: 10.1093/BJA/aex166.
- Eskin MB, Ceylan A. Comparison of the effects of interscalene, supraclavicular and infraclavicular peripheral nerve blockades on perfusion index. Ortadogu Tip Dergisi 2020; 12(1); 96-102. doi.org/10.21601/ortadogutipdergisi.646 741.
- Gurkan Y, Kus A, Aksu C, Ohtaroglu C, Solak M, Toker K. Degisen akımlar ve Turkiye'de rejyonal anestezi uygulamaları. Agri 2014; 26(3):131-7. doi: 10.5505/agri.2014. 26056.
- Liu SS, Ngeow J, John RS. Evidence basis for ultrasound-guided block characteristics: Onset, quality and duration. Reg Anesth Pain Med 2010; 35(Suppl 2):26-35. doi: 10.1097/AAP.0b013e3181d266f0.