Percutaneous Uniplanar Pedicle Screw-Rod System with Injured Vertebra Fixation for Thoracolumbar Burst Fracture and Technique Notes
By Qilin Lu, Hui Kang, Chengjie Xiong, Chao Sun, Feng XuAffiliations
doi: 10.29271/jcpsp.2022.10.1295ABSTRACT
Objective: To evaluate the efficacy of percutaneous uniplanar pedicle screw (PUPS) combined with injured vertebra fixation for treating thoracolumbar burst fracture and provide technique notes.
Study Design: A descriptive study.
Place and Duration of Study: Department of Orthopaedics, General Hospital of Central Theater Command, Wuhan, China, from February 2019 to December 2021.
Methodology: Patients who had undergone PUPS internal fixation for thoracolumbar burst fracture were followed up for more than 12 months in the General Hospital of Central Theater Command, Wuhan, China. The operation time, intraoperative blood loss, and hospital stay were recorded. Visual analysis scale (VAS), score of low back pain, ODI (oswestry disability endex), anterior vertebral height (AVH), Cobb angle were documented before and after the operation, Also, the complications and postoperative tail shank angles (TSA) were documented.
Results: All 23 patients were followed up for more than 12 months without re-fracture, loosening or breakage of the screw and rod. The operation time, intraoperative blood loss, and hospital stay were 51.34±8.30 minutes, 75.67±16.55 minutes, and 9.86±1.96 days respectively. VAS and ODI scores after the operation were significantly lower than before (p <0.05). The AVH and Cobb angle after operation were significantly better as compared with those before the operation (p <0.05), but no statistically significant difference was found in those two values at 1 week, 3 months, and 12 months after operation (p >0.05). No statistically significant difference was found in TSA after the operation (p >0.05).
Conclusions: PUPS combined with injured vertebra fixation reveals satisfactory efficacy for thoracolumbar burst fracture with well reduction of the fracture, the AVH, and Cobb angle maintenance.
Key Words: Percutaneous uniplanar pedicle screw, Minimally invasive surgery, Thoracolumbar vertebral body fracture, Injured vertebra fixation.
INTRODUCTION
Thoracolumbar vertebral body burst fracture is a common spinal injury among young and middle-aged patients which accounts for 5% to 6% of all fractures and impacts the patient’s life quality.1,2 Surgical treatment was recommended to patients (AO, type A3) with thoracolumbar injury classification and severity score (TLICS) >3. Percutaneous pedicle screw fixation with polyaxial or fixed-headed has become the main treatment for thoracolumbar fractures without neurological symptoms.3 For polyaxial-headed screws fixation, The height reduction of injured vertebrae is poor.
Local kyphosis is difficult to completely correct, and late-onset kyphosis can easily occur in the long-term. For fixed-headed screws fixation, the connecting rod is difficult to be installed percutaneously and the high concentrated stress is prone to causing the screw and rod system broken.4,5 Improvement of screw property was noticed, and percutaneous uniplanar pedicle screw (PUPS) was proposed as a novel screw.
This study was carried out to investigate the advantages and efficacy in treating thoracolumbar burst fracture with injured vertebra fixation.
METHODOLOGY
Files were analysed retrospectively for 23 patients who had undergone PUPS combined with injured vertebra fixation for thoracolumbar burst fracture from February 2019 to December 2021 in the General Hospital of Central Theater Command. This retrospective study had been approved by the Research Ethics Committee of Medical Service (No. HRECMS20190112). All patients signed on informed consent forms before surgery. Surgeries were performed by the same senior surgeon. Inclusion criteria were single level thoracolumbar vertebral body fracture, thoracolumbar burst fracture with AO, type A3, occupying less than 1 / 4 of sagittal diameter in the spinal canal, no lower extremity symptom, mild neurological symptom, obvious injury of the pedicle and spinal appendage, intact intervertebral disc, no obvious contraindications of operation in the preoperative examination, and follow-up available for more than one year after the operation. Exclusion criteria were preoperative examination did not meet the operation requirement, female >60 years, male >65 years, or / and with osteoporosis, pathological fracture or combined with other parts of the malignant tumour, spinal canal stenosis caused by obvious bone or hematoma, marked neurological symptoms, fracture to operation time more than 2 years, and multiple injuries of viscera and head.
Preoperative X-ray, CT, MRI, ECG, and blood examination were carried out. Routine intraoperative use of antibiotics to prevent possible incision infection. VAS and ODI were evaluated, AVH and Cobb angle were measured on a computer by an imaging system. The result value has been automatically retained with 0.01. Introduction of the disease condition and treatment were carried out, and the patients and their families were informed of the risk and agreed to the operation.
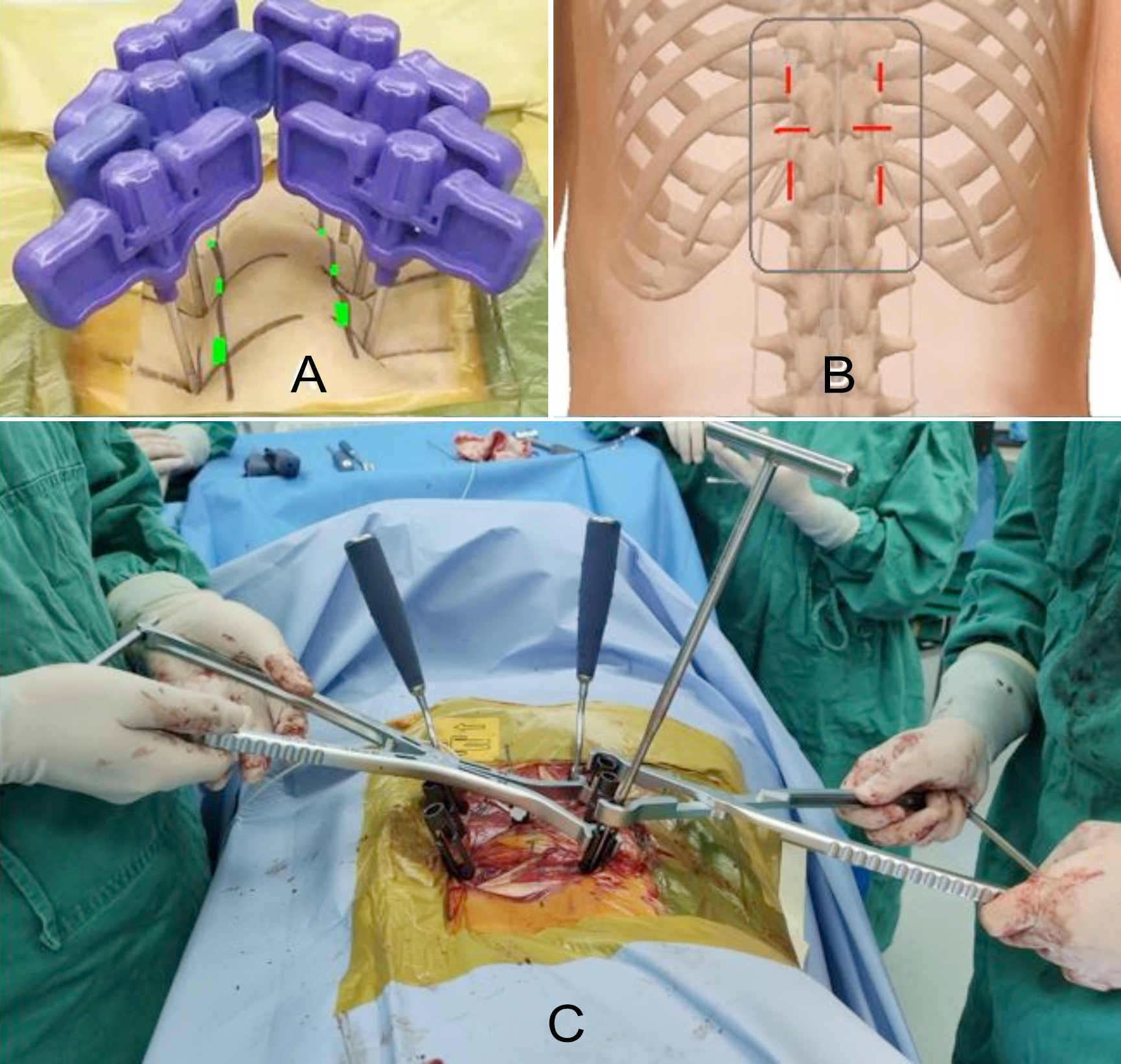 Figure 1: A showed six pedicle shadows were marked on the skin surface (green part), and six puncture needles puncture skin points at a little laterosuperior distance away from skin pedicle marks. B showed the alternated vertical and horizontal skin incisions centred on guide wires were made. C showed that the surgical instrument performed stretch reduction with only the lower nut on the rod lock.
Figure 1: A showed six pedicle shadows were marked on the skin surface (green part), and six puncture needles puncture skin points at a little laterosuperior distance away from skin pedicle marks. B showed the alternated vertical and horizontal skin incisions centred on guide wires were made. C showed that the surgical instrument performed stretch reduction with only the lower nut on the rod lock.
The patient was placed in a prone position after general anaesthesia. C-arm fluoroscopy was used to locate the six pedicle shadows marked on the skin. Six puncture needles were used to puncture skin points that were at a little laterosuperior distance away from skin pedicle marks (Figure 1A) after disinfection of skin. When each needle tip reached the bony part at the right point, the AP view under fluoroscopy showed that the needle tip was located in the upper and outer parts of pedicle shadows (left on 10 o’clock position and right on 2 o’clock position). The angle of each puncture needle was adjusted on the lateral view, so that, the puncture needle could insert into the vertebral body through the pedicle with parallel to the upper endplate of each vertebra. When needles reached the posterior wall of the vertebral body (the base of the pedicle), the puncture needles should not exceed the inner edge of the pedicle shadow in AP view. After passing over the posterior wall of every vertebral body, the puncture needle continuously entered 5 mm depth. Needle cores were put out with the sleeve left in the vertebral body. Guide wires were inserted until they reached the bony part at the bottom. Alternated vertical and horizontal skin incisions centred on guide wires were made (Figure 1B). Percutaneous cannulated screws with added long tail leaves were inserted along the guide wires one by one. Fluoroscopy checked the position of the screws. The physiological curvature rods were directly locked by screw nuts if the height of the anterior edge of the injured vertebra and the correction of deformity were satisfied. If they were not satisfied, the stretch reduction was performed by surgical instrument (Figure 1C). Fluoroscopy confirmed the position of the pedicle screw-rod system and reduction condition. The added long tail leaves of the screw were taken off. The wound was washed with saline and sutured.
 Figure 2: Typical case: 42 years male patient was admitted to the hospital with lumbar pain caused by trauma for one day. A showed fresh L2 burst fracture without occupation in the spinal canal. B showed the reduction of fracture and PUPS combined with injured vertebra fixation one week after surgery. C and D showed spine and PUPS internal fixation condition at 3rd and 12th months follow-up. E showed internal fixation was removed 15 months after bone healing.
Figure 2: Typical case: 42 years male patient was admitted to the hospital with lumbar pain caused by trauma for one day. A showed fresh L2 burst fracture without occupation in the spinal canal. B showed the reduction of fracture and PUPS combined with injured vertebra fixation one week after surgery. C and D showed spine and PUPS internal fixation condition at 3rd and 12th months follow-up. E showed internal fixation was removed 15 months after bone healing.
Patients left the bed wearing thoracolumbar brace 3 days after the operation. VAS and ODI were evaluated, AVH Cobb angle and TSA were measured one week after the operation. Functional exercise of lumbodorsal muscles was instructed to patients one week after the operation. The sutures were removed according to the wound conditions around 10 days after the operation. The patients were followed up at 3rd and 12th months. The internal fixation was removed according to the bone healing 1 year later. Evaluation indexes: The operation-related indexes (operation time, intraoperative blood loss volume, and hospital stay time); VAS and ODI were calculated. The anterior height of injured vertebrae (AHV) was measured on the lateral view. Cobb angle was measured as the intersection angle of the vertical line of the upper endplate line of the upper vertebrae and the vertical line of the lower endplate line of lower vertebrae. Two lines were drawn along the axis of the screw body and the screw tail were made in lateral view of the X-ray picture and the tail-shank angle (TSA) was measured between the two axes.
The SPSS 24.0 software was used for statistical analysis. The measurement data was recorded as mean ± standard deviation. The t-test was used to compare values before and after surgery. Repeated measures ANOVA was used to compare the values on three time points. The p-value <0.05 was regarded as a significant statistical difference.
RESULTS
All patients (23 cases) with thoracolumbar fractures who had undergone reduction and PUPS combined with injured vertebra fixation were followed up for more than 12 months (12~19, 14.82±2.08 on average months). The average operation time was 51.34±8.30 minutes, the blood loss was 75.67±16.55 ml, and the average hospital stay was 9.86±1.96 days. One patient’s incision was red and scabby, and experienced delayed healing in 20 days.
CT scanning showed that all the screws were in the pedicles. VAS score and ODI after operation were significantly lower than before (p <0.05). The AVH and Cobb angle after operation were statistically significantly better as compared with those before the operation (p <0.05), but no statistically significant difference in those two values was found at 1 week 3 months, and 12 months after operation (p >0.05). There was no statistically significant difference found in TSA at 1 week 3 months, and 12 months after operation (p >0.05, Table I). During the follow-up period, there was no re-fracture, loosening or breakage of internal fixation happened (Figure 2).
DISCUSSION
The thoracolumbar region is the most common site of spinal fracture. And thoracolumbar burst fracture with TLICS >3 is mainly treated surgically.6 Surgery aims to correct the deformity, immobilise the spine, and indirectly decompress the spinal canal.7,8 Open surgery is a frequently used treatment for thoracolumbar vertebral body fractures. However, the traditional procedure has disadvantages of long operative time, large blood loss, posterior ligaments complex injury, high infection rate, and persistent postoperative low back pain, which significantly affect the patient’s quality of life.9 With the development of minimally invasive concepts and minimally invasive surgery, percutaneous pedicle screw has various advantages, including less trauma, less bleeding, short operation time, and quick recovery.10 It is an ideal method for patients suffering from thoracolumbar burst fracture with mild or without obvious lower-extremity neurological symptoms.
PUPS is a combination type of percutaneous fixed-axis and multiaxial screw. Although the fixed-axis pedicle screw has a good reduction ability for vertebral body fracture, it still has two main shortcomings.11-13 Firstly, when more screws are implanted, it is not easy to longitudinally install the rod. Secondly, Stress concentration at the interface of screw and rod tends to cause fixation breakage, especially on the upper part of fixation for the connection region stress. Multiaxial screws are currently the procedure of choice when treating vertebrae fractures.14 The screw shaft connects a universal direction tail which could be rotated freely along the screw’s axial direction. It can decrease the difficulty of intraoperative manipulation. However, when a multiaxial screw is applicated, it is hard to achieve satisfactory kyphosis correct for the injured spine, and delayed kyphosis may occur in the long term.15 Therefore, to combine the advantages and discard the disadvantages of these two screws, a uniplanar pedicle screw has been developed and applied in the clinic. It can be divided into sagittal and coronal uniplanar movement pedicle screws according to the direction of motion. This sagittal uniplanar pedicle screw’s U-shaped tail is fixed in the coronal plane but can move in the sagittal direction, mainly used to correct and maintain the coronal rotation deformity. It is more effective in correcting and maintaining the coronal deformity of the spine than the multiaxial pedicle screw. While coronal uniplanar pedicle screw tail can move in the coronal plane but is fixed in the sagittal plane, which has an advantage in correcting kyphosis in sagittal reduction of thoracolumbar vertebral body fracture (Figure 3). PUPS is easier to fix titanium rod than monoaxial screw and has better reduction and longitudinal support effect than the multiaxial screw. In addition, the distraction of the anterior longitudinal ligament, vertebral body, and intervertebral disc by the distraction device can promote the recovery of the height of the anterior edge and the correction of kyphosis.
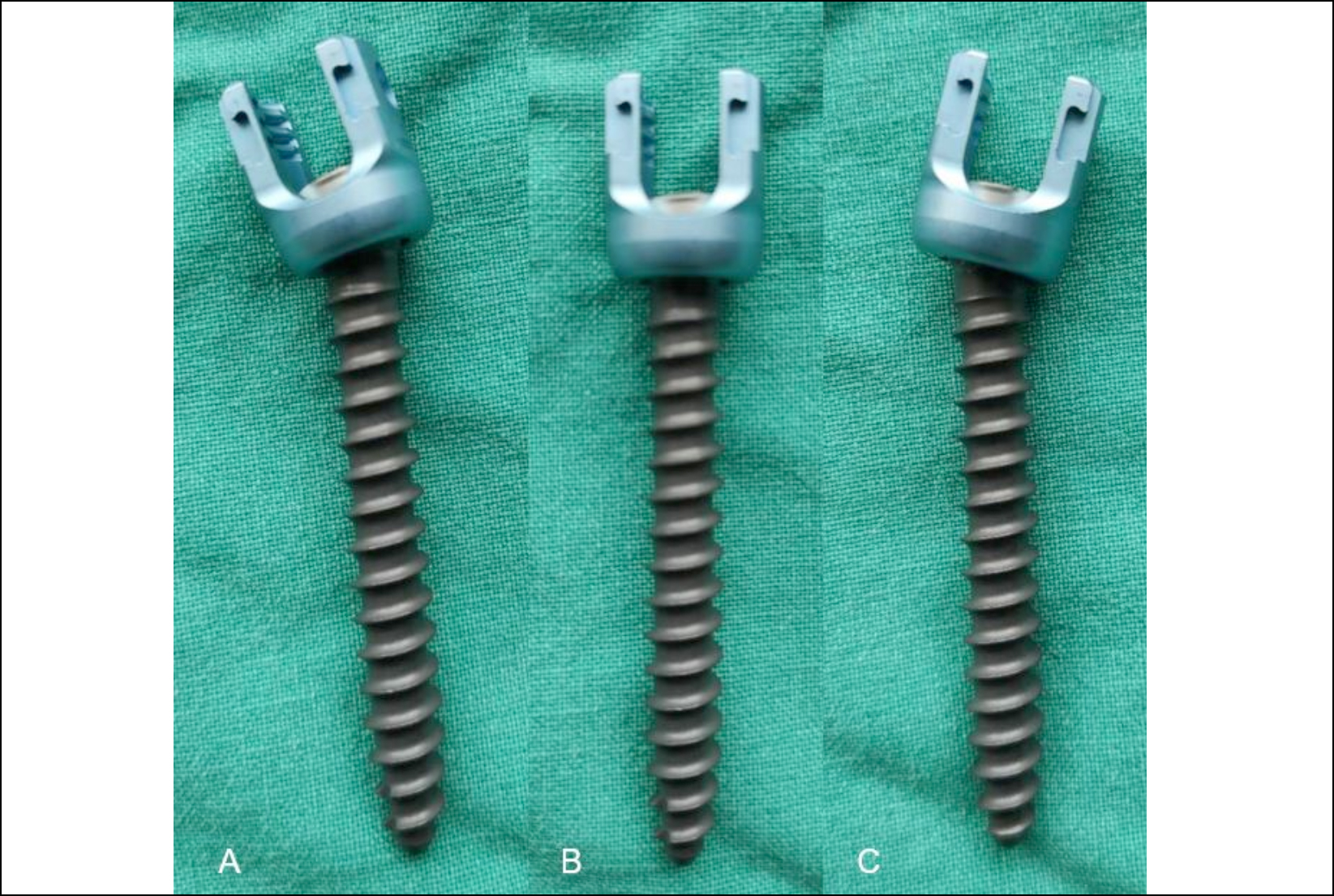 Figure 3: Percutaneous cannulated coronal uniplanar pedicle screw has a movable tail, which can move in the coronal plane but is fixed in the sagittal plane.
Figure 3: Percutaneous cannulated coronal uniplanar pedicle screw has a movable tail, which can move in the coronal plane but is fixed in the sagittal plane.
Table I: VAS score, ODI, AVH (mm), Cobb angle (°), and TSA (°) before and after surgery.
|
|
(1) Before surgery |
(2) 1 Week after surgery |
(3) 3 Months after surgery |
(4) 12 Months after surgery |
(1)(2)t / (2)(3)(4)F |
(1)(2)P / (2)(3)(4) |
|
VAS |
7.43±0.79 |
1.83±0.72 |
1.04±0. 56 |
1.00±0.74 |
26.04 /10.84 |
<0.001/<0.001 |
|
ODI |
80.65±2.89 |
27.83±2.64 |
18.78±2.84 |
16.74±1.60 |
70.85/136.32 |
<0.001/<0.001 |
|
AVH |
18.06±1.68 |
26.96±1.19 |
26.61±1.23 |
26.16±1.10 |
27.48/2.672 |
<0.001/0.07 |
|
Cobb |
24.56±3.70 |
9.57±1.13 |
9.85±1.34 |
10.12±1.33 |
21.55/1.07 |
<0.001/0.34 |
|
TSA |
- |
3.37±0.76 |
3.39±0.81 |
3.47±0.62 |
/0.13 |
/0.88 |
|
Data were compared (1) with (2) using paired samples t-test. Data were compared among (2)(3) and (4) using repeated measures ANOVA. |
||||||
In this study, the AVH and Cobb angle significantly recovered from 18.06±1.68 and 24.56±3.70° to 26.96±1.19 and 9.57±1.13°, respectively before and after the operation. It was still maintained at 26.16±1.10 and 10.12±1.33°, with no internal fixation fracture after one year. There was no significant difference in TSA angle between the three segments [(3.37±0.76)°, (3.39±0.81)°, and (3.47±0.62)°] after the operation. This showed that the coronal uniplanar pedicle screw could provide a better distraction reduction effect, mechanical stability, and fatigue resistance. The WAS and ODI significantly reduced from 7.43±0.79 and 80.65±2.89 to 7.43±0.79 and 27.83±2.64 respectively before and after the operation. It was still significantly decreased to 1.00±0.74 and 16.74±1.60 after one year. Therefore, the satisfactory reduction and stable fixation were the premises of symptom improvement. In addition, the average operation time, amount of bleeding, and average hospital stay were 51.34±8.30 min, 75.67±16.55 ml, and 9.86±1.96 days respectively, have indicated that the application of PUPS combined with injured vertebra fixation revealed no obvious disadvantage in terms of surgical injury or operation difficulty.
According to the technical requirements of screws’ placement, pedicle screws are inserted into the vertebrae one level above and one level below the fractured vertebra, which is the classical approach for surgical management in the early development stage.16 However, multiple subsequent studies have shown that this fixation way is prone to developing postoperative vertebral height loss, aggravation of kyphosis deformity, rod/screw breakage, or loosening.17 Against the above backdrops, the application of pedicle screws at the fractured vertebral level has developed gradually. The advantages of this way are multiple. The body height of the fractured vertebrae can be restored by pry-poking with pedicle screws directly, and also acquire enough supporting strength. After the screw placement, the stability of the injured vertebrae is increased to reduce the compressive stress of the vertebral body and the stress load on internal fixation. Previous studies have also shown that the fractured vertebrae fixed with pedicle screws could provide multiple-point fixation, overcome the “quadrilateral or suspension effect”, and get better biomechanical properties.18
Technique notes about PUPS combined with injured vertebra fixation in treating thoracolumbar burst fracture are many. Six PUPS are always implanted to treat single-segment vertebra fractures. Alternated vertical and horizontal skin incisions are made to avoid connecting with each other on both sides (Figure 1B). The skin tension around each small incision should be considered not to affect incision healing. Manual reduction for fractured vertebra is an important procedure before the surgery, which is helpful for the fractured vertebra screw placement at the next step. Type A3 fractures sometimes lead to vertebral compression with different degrees on the right and left sides endplate. Once the manual reduction before screw placement fails, the screw placement on the heavy compression side is at risk of upper endplate penetration. In this case, screws can be placed on the light compression side first, and stretch reduction by the instrument is performed from this side. Subsequently, contralateral screw placement parallel to the endplate will be easy to achieve. Successful placement of the pedicle screw at one time is sure to improve the force in performing and keeping the reduction. During the screw insertion, it is essential to hold and watch the guide wire to avoid the guide wire going forehead with the screw to penetrate the anterior wall of the vertebral body. Screw placed in injured vertebrae should be chosen with enough diameter and length. It is always close to the upper endplate, which can increase the force to perform intraoperatively and maintain stability postoperatively. The force for stretch reduction by surgical instrument should be controlled to prevent iatrogenic bony injury. After reduction, the curve of the two rods is determined and put on according to the intraoperative fluoroscopy on the spine. Nets lock on the lower vertebrae screw first and the upper vertebrae screw at second are essential. This kind of caudal and cranial screw lock with curved rods can perform reduction for injured vertebrae at the first time. Then, the second reduction and support can be carried out by the next net lock on the injured vertebra between the connecting rod and screw. After reduction and fixation according to the above step, the two nuts on the upper vertebrae are loosed for a few seconds and locked again one by one. This is a stress adjustment procedure that hardly affects the reduction effect but can reduce the breakage of the internal fixation for the screw rod connection region stress in the long-term.
CONCLUSION
PUPS combined with injured vertebra fixation reveals satisfied efficacy in treating thoracolumbar burst fracture without nerve injury. Moreover, it has the advantages of restoring vertebral height, maintaining Cobb angle, and symptom improvement. It also shows well mechanical stability and anti-fatigue property on the spine. Therefore, PUPS combined with injured vertebra fixation is worthy of clinical promotion for thoracolumbar vertebral body fracture.
PATIENTS’ CONSENT:
Informed consent was obtained from all patients.
ETHICAL APPROVAL:
The study was approved by the Research Ethics Committee of Medical Service of General Hospital of Central Theater Command (Decision date: 1/10/2019, Decision No. HRECMS20190110).
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
QL, HK, CX, CS, FX: Contributed to the study's conception and design.
CS, CX: Performed material preparation, data collection, and analyses.
HK: Performed operations.
QL, FX: Designed the surgery plan and wrote the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- De Iure F, Lofrese G, De Bonis P, Cultrera F, Cappuccio M, Battisti S. Vertebral body spread in thoracolumbar burst fractures can predict posterior construct failure. Spine J 2018; 18(6): 1005-13. doi: 10.1016/j.spinee.2017.10.064.
- Hong JY, Choi SW, Kim GD, Kim HK, Shin BJ, Kim EH, et al. Reliability analyses of radiographic measures of vertebral body height loss in thoracolumbar burst fractures. World Neurosurg 2019; 129: 191-8. doi10.1016/j.wneu.2019. 05.094.
- Sahai N, Faloon MJ, Dunn CJ, Issa K, Sinha K, Hwang KS, et al. Short-segment fixation with percutaneous pedicle screws in the treatment of unstable thoracolumbar vertebral body fractures. Orthopedics 2018; 41(6):e802-6. doi: 10.3928/ 01477447-20180912-05.
- Zhao Q, Hao D, Wang B. A novel, percutaneous, self-expanding, forceful reduction screw system for the treatment of thoracolumbar fracture with severe vertebral height loss. J Orthop Surg Res 2018; 13(1):174. doi: 10.1186/s13018- 018-0880-4.
- Fogel GR, Reitman CA, Liu W, Esses SI. Physical characteristics of polyaxial-headed pedicle screws and biomechanical comparison of load with their failure. Spine (Phila Pa 1976) 2003; 28(5):470-3. doi: 10.1097/01.BRS. 0000048652.45964.2E.
- Wang S, Duan CY, Yang H, Kang JP, Wang Q. Novel screw insertion method for anterior surgical treatment of unstable thoracolumbar fracture: Quadrant positioning method. Orthop Surg 2019; 11(4):613-9. doi: 10.1111/os.12506.
- Kao FC, Hsieh MK, Yu CW, Tsai TT, Lai PL, Niu PL, et al. Additional vertebral augmentation with posterior instrumentation for unstable thoracolumbar burst fractures. Injury 2017; 48(8): 1806-12. doi: 10.1016/j.injury.2017. 06.015.
- Kirkham B Wood, Weishi Li, Darren R Leb. Management of thoracolumbar spine fractures Spine J 2014; 14(1): 145-64. doi: 10.1016/j.spinee.2012.10.041.
- Defino HLA, Costa HRT, Nunes AA. Open versus minimally invasive percutaneous surgery for surgical treatment of thoracolumbar spine fractures- a multicenter randomised controlled trial: Study protocol. BMC Musculoskelet Disord, 2019; 20(1):397. doi: 10.1186/s12891-019-2763-1.
- Walker CT, Xu DS, Godzik J. Minimally invasive surgery for thoracolumbar spinal trauma. Ann Transl Med 2018; 6(6):102. doi: 10.21037/atm.2018.02.10.
- Liu H, Wang H. Biomechanical comparison of posterior intermediate screw fixation techniques with hybrid monoaxial and polyaxial pedicle screws in the treatment of thoracolumbar burst fracture: A finite element study. J Orthop Surg Res 2019; 14(1):122. doi: 10.1186/s13018-019- 1149-2.
- Wang H, Zhao Y, Mo Z. Comparison of short-segment monoaxial and polyaxial pedicle screw fixation combined with intermediate screws in traumatic thoracolumbar fractures: A finite element study and clinical radiographic review. Clinics (Sao Paulo) 2017; 72(10):609-17. doi: 10. 6061/clinics/2017(10)04.
- Qin W, Chen K, Chen H. Comparison of polyaxial or poly/monoaxial mixed screw fixation for treatment of thoracolumbar fractures with o-arm navigation: A case-control study. World Neurosurg 2020; 138: e10-e16. doi: 10.1016/ j.wneu.2020.01.123.
- Xiong C, Huang B, Wei T. Effect of the short-segment internal fixation with intermediate inclined-angle polyaxial screw at the fractured vertebra on the treatment of Denis type B thoracolumbar fracture. J Orthop Surg Res 2020; 15(1):182. doi: 10.1186/s13018-020-01686-7.
- Kuklo T R, Potter B K, Polly D W. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2005; 30(18): 2113-20. doi: 10.1097/01.brs.0000179260.73267.f4.
- Dobran M, Nasi D. Treatment of unstable thoracolumbar junction fractures: short-segment pedicle fixation with inclusion of the fracture level versus long-segment instrumentation. Acta Neurochir (Wien) 2016; 158(10): 1883-9. doi: 10.1007/s00701-016-2907-0.
- Zbek Z, Zkara E, Nner H. Treatment of unstable thoracolumbar fractures: Does fracture-level fixation accelerate the bone healing? World Neurosurg 2017; 107:362-70. doi: 10.1016/j.wneu.2017.08.007.
- Kapoen C, Liu Y, Bloemers FW. Pedicle screw fixation of thoracolumbar fractures: Conventional short segment versus short segment with intermediate screws at the fracture level-a systematic review and meta-analysis. Eur Spine J 2020; 29(10):2491-2504. doi: 10.1007/s00586-020- 06479-4.