Pancreatic Tuberculosis mimicking as a Pancreatic Mass Lesion
By Zain Majid1, Adeel ur Rehman1, Hina Ismail1, Nasir Hassan Luck1, Muhammad Mubarak2Affiliations
doi: 10.29271/jcpsp.2022.11.1486ABSTRACT
Tuberculosis is a global health problem and commonly affects the respiratory system. The involvement of the pancreas in this disease is a rare event. We hereby report a case of a young male who presented with right hypochondrial pain along with significant weight loss. Further workup revealed a raised erythrocyte sedimentation rate along with a pancreatic mass lesion on the CT scan. Endoscopic ultrasound-guided biopsy of the pancreatic lesion revealed evidence of caseation necrosis along with epithelioid granuloma, findings suggestive of tuberculosis. He was started on anti-tuberculous therapy for 6 months and a repeat CT scan showed complete disappearance of the mass lesion and resolution of symptoms.
Key Words: Tuberculosis, Pancreatic mass, Endoscopic ultrasound, Biopsy.
INTRODUCTION
Tuberculosis (TB) is one of the leading infectious causes of death and globally is among the top 10 causes of death.1 It most commonly affects the lungs,1 while the involvement of the pancreas is rare and is mostly seen in areas having a high prevalence of the disease.2
Over 10% of those with pulmonary TB have extra-pulmonary involvement, with pancreatic TB being an uncommon form of extra-pulmonary TB that usually mimics a pancreatic neoplastic lesion in the majority.2
CASE REPORT
A 32-year unmarried male, having no prior comorbids presented to our outpatients’ department with the complaints of right hypochondrial pain, on and off, for the past 1 year. He also had a history of weight loss of around 15 kg during this time, which the patient attributed to loss of appetite. He denied any history of night sweats or fever. His general practitioner had prescribed him proton pump inhibitors, but his symptoms did not resolve. His family history was not significant for any disease or malignancy.
His initial workup outside showed a hemoglobulin of 13.7 g/dl with a total leukocyte count of 11,700 cells/mm,3 platelet count of 231 × 109 /l, INR of 1.08, Creatinine (Cr), 0.9mg/dL, total bilirubin,0.84 mg/dl, Alanine aminotransferase (ALT), 16 U/L and a fasting blood sugar (FBS) of 79 mg/dL. His Fasting lipid profile (FLP) showed serum cholesterol of 169 mg/dL and triglyceride of 61 mg/dL. Viral serology (HbsAg and Anti-HCV) was negative (Table I).
Table I: Laboratory workup of the patient.
|
Labs |
Result |
Labs |
Result |
|
Haemoglobin |
13.7 g/dl |
Creatinine |
0.9 mg/dL |
|
TLC |
11,700 cells/mm3 |
Bilirubin |
0.84 mg/dL |
|
Platelets |
231×109/L |
ALT |
16 U/L |
|
INR |
1.08 |
Cholesterol |
169 mg/dL |
|
HbsAg |
-ve |
Triglyceride |
61 mg/dL |
|
Anti HCV |
-ve |
ESR |
60 mm/1st hr |
|
Stool for fat globules |
-ve |
Amylase |
33 mg/dl |
|
Faecal elastase |
270 ug/g |
CA 19-9 |
1.6 U/ml |
|
AFP |
2.9 ng/ml |
CEA |
2 ng/ml |
|
|
|
IgG4 |
100 mg/dl |
Chest X-Ray revealed no visible abnormality, while erythrocyte sedimentation rate (ESR) was raised at 60 mm/1st hour. The tuberculin skin test had shown an induration of more than 5 mm. His serum amylase (33 mg/dL), stool for fat globules and faecal elastase were all within normal limits. Ultrasound (US) abdomen showed bulky pancreas while the rest of the organs appeared normal.
Contrast enhanced CT showed an ill-defined, rounded poorly enhanced, soft tissue density mass involving the pancreatic head measuring 3.7 × 4.8 cm abutting the inferior vena cava and left renal vein and causing pressure effects to the adjacent structures with no major lymphadenopathy (Figure 1). The rest of the scan appeared normal.
For epigastric pain, an upper gastrointestinal endoscopy was performed that showed moderate antral erythema, biopsy of which was non-specific.
Later on, serum IgG4 levels were sent to rule out IgG4-associated disease and were within normal range.
 Figure 1: Pre-ATT contrast enhanced CT scan of abdomen axial section showing a mass lesion noted in the head of the pancreas as shown by the arrow.
Figure 1: Pre-ATT contrast enhanced CT scan of abdomen axial section showing a mass lesion noted in the head of the pancreas as shown by the arrow.
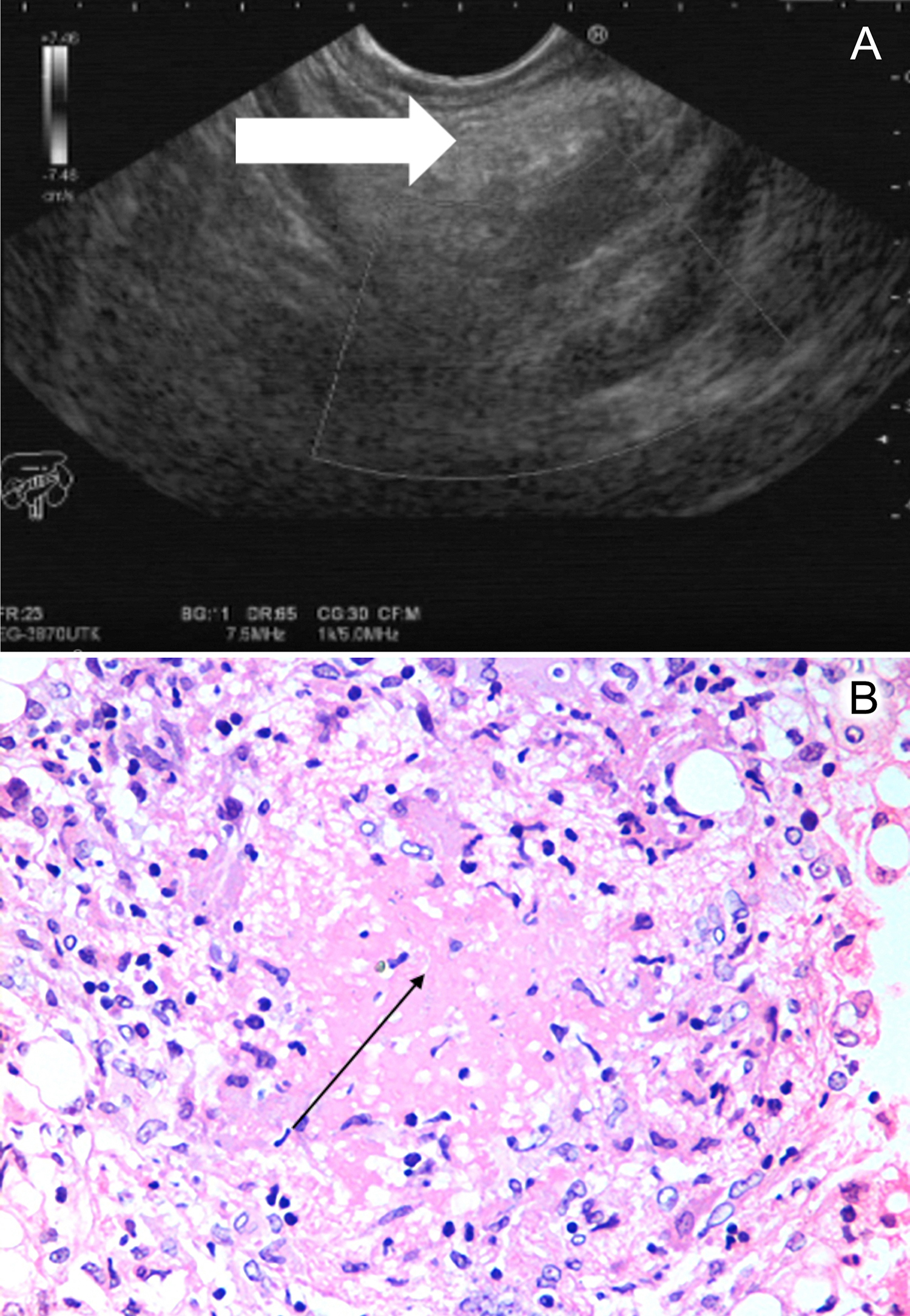 Figure 2: (A) Endoscopic Ultrasound (EUS) image showing the mass in the head of the pancreas as depicted by the arrow. (B) EUS-guided biopsy of the head of the pancreas showing the evidence of caseation necrosis (shown by the arrow) surrounded by epithelioid cells forming a granuloma, highly suggestive of Tuberculosis.
Figure 2: (A) Endoscopic Ultrasound (EUS) image showing the mass in the head of the pancreas as depicted by the arrow. (B) EUS-guided biopsy of the head of the pancreas showing the evidence of caseation necrosis (shown by the arrow) surrounded by epithelioid cells forming a granuloma, highly suggestive of Tuberculosis.
In order to obtain biopsy of the pancreatic mass lesion, an endoscopic US (EUS)-guided biopsy was planned, which revealed the same ill-defined mass arising from the uncinate process measuring 1.8 × 4.7 cm. Fine needle biopsy (FNB) was done using a 22 gauge FNB needle via slow pass technique (Figure 2A).
Biopsy findings revealed extensive areas of caseating necrosis along with scattered epithelioid granulomas and multinucleated Langhan giant cells. No evidence of malignancy was noted (Figure 2B). Hence, a diagnosis of pancreatic TB was made.
The tumour markers showed CA19-9 of 1.6 U/mL, AFP, 2.9 ng/ml, and CEA, 02 ng/ml.
On the suspicion of pancreatic TB, the infectious disease department was taken on board and the patient was started on anti-tuberculous therapy (ATT) for 6 months, which included isoniazid (H), rifampicin (R), pyrazinamide (Z) and ethambutol (E) in fixed-dose combination HRZE for 3 months and was later kept on HR for the remainder of the course. He was advised regular twice weekly follow-ups initially and monthly follow-ups later on.
After a span of 6 months, he was followed up again in our OPD, having complete relief from his symptoms along with a weight gain of 3 kg during this time period. A repeat CT revealed no evidence of mass lesion in the pancreas (Figure 3).
 Figure 3: Post-ATT contrast enhanced CT scan of abdomen axial sections through the region of pancreas showing the disappearance of the previously noted mass lesion in the head of the pancreas.
Figure 3: Post-ATT contrast enhanced CT scan of abdomen axial sections through the region of pancreas showing the disappearance of the previously noted mass lesion in the head of the pancreas.
DISCUSSION
Pancreatic TB accounts for less than 5% of all cases of TB from the developing world.3 The main symptoms include abdominal pain, jaundice along with weight loss. Rare symptoms include gastro-intestinal bleed due to splenic vein thrombosis.2
As for the workup, the tuberculin skin test aids in the diagnosis while abdominal imaging is not specific, so an image-guided biopsy of the pancreatic mass lesion is recommended. Findings on the CT scan abdomen have been reported as a hypodense area in the pancreatic head,4 which was also the finding seen in our case. Currently, EUS-guided biopsy of the pancreatic mass lesion is the gold standard test for its diagnosis.5 Cytology of the biopsy specimen may show granulomatous inflammation, plasma cells and epithelioid histiocytes, while acid-fast bacilli are rarely noted.6 Other investigations include a positive mycobacterium TB (MTB) culture or MTB PCR.6,7
As for the treatment, pancreatic TB is treated with ATT for at least 6 months with resolution of symptoms and imaging, guiding the management as also seen in this case.
This case highlights the successful treatment of pancreatic TB with ATT and highlights that those physicians working in high TB endemic areas should keep in mind the diagnosis of pancreatic TB when encountering pancreatic mass lesion in a young individual.
PATIENT’S CONSENT:
Informed written consent was obtained
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
ZM: Wrote the manuscript and managed the patients.
AR: Did the EUS-guided biopsies and managed the patients.
HI: Wrote the manuscript.
NHL: Overall supervision and final correction/editing of the manuscript.
MM: Provided the histopathological images.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Tuberculosis (TB). Who.int. 2020 [cited 8 June 2020]. www.who.int/news-room/fact-sheets/detail/tuberculosis.
- Zacharia GS, Antony R, Kolassery S, Ramachandran TM. Isolated pancreatic tuberculosis masquerading as pancreatic cancer. Gastroenterol Rep (Oxf) 2014; 2(2): 154-7. doi: 10.1093/gastro/gou017.
- Zhu M, Zhang N, Tao W, Wang Z, He S. Pancreatic tuberculosis with vascular involvement and peritoneal dissemination in a young man. Case Rep Med 2017; 2017:4396759. doi: 10.1155/2017/4396759.
- Jethwani U, Singh G, Mohil R, Kandwal V, Chouhan J, Saroha R, et al. Pancreatic tuberculosis: A case report. OA Case Rep 2013; 5:41.
- Raghavan P, Rajan D. Isolated pancreatic tuberculosis mimicking malignancy in an immunocompetent host. Case Rep Med 2012; 2012:501246. doi: 10.1155/2012/501246.
- Levine R, Tenner S, Steinberg W, Ginsberg A, Borum M, Huntington D. Tuberculous abscess of the pancreas. Case report and review of the literature. Dig Dis Sci 1992; 37(7):1141-4. doi: 10.1007/BF01300301.
- Yokoyama T, Miyagawa S, Noike T, Shimada R, Kawasaki S. Isolated pancreatic tuberculosis. Hepatogastroenterol 1999; 46:2011-14.