Paediatric Emergency Medicine: Reality, Expectation, Experience, and Need for Improvements from a Low- Income Settings
By Emad uddin Siddiqui, Sara Fatima, Abid Ali Jamali, Tooba SiddiquiAffiliations
doi: 10.29271/jcpsp.2023.06.601During the late 17th century, Dr Benjamin Rush wrote a visionary book "Diseases Specific to Children" which was the initial literature available on the importance of paediatric-specific illnesses; a couple of centuries later, paediatric medicine was recognised as a separate entity. Considering the unique physiological, anatomical, pathological, aetiological, and psychological spectrum of paediatric disease, the first children’s hospital became functional in 1855 (Children’s Hospital, Philadelphia - CHOP), while the first recognised paediatric speciality chapter was established as the American Academy of paediatrics in 1930.1
Paediatric emergencies are quite different from adult emergencies, as children are sub-optional communicators of their symptoms, they are less cooperative when in distress, parental anxiety may also aggravate child fretfulness, and examination will be difficult and anxiety may aggravate or portray disease severity differently. Moreover, many symptoms may mimic other illnesses like inborn errors of metabolism, congenital defects, occult trauma or child abuse etc. Paediatric emergency medicine (PEM) is a medical speciality with the principal mission of evaluating, managing, and treating illnesses and injuries among children. Paediatric emergency care is one of the critical components of the healthcare system that poses a huge impact on improving mortality and morbidity of common childhood illnesses.
In 1981, the first PEM training program was started at CHOP, and the first PEM subspeciality board certification was administered in the US in 1992.2 In the last few decades, PEM gained sub-speciality recognition from different professional organisations like the American Academy of Paediatrics (AAP), American College of Emergency Physicians (ACEP), Ambulatory Paediatric Association (APA), International Federation of Emergency Medicine (IFEM), and Pakistan Society of Emergency Medicine (PSEM).3,4
In developing countries, PEM is a much newer concept. PEM links between specialities of General Paediatric and Emergency Medicine (EM). Residency training in EM or Paediatrics covers some aspects of PEM, however, via such training, residents are neither able to learn comprehensive experience nor able to deliver mastery in PEM. Over the last four decades, developed nations have started PEM fellowship/training as their advanced training program, a second training opportunity, for candidates who are already trained in Paediatrics or EM. But the scenario is quite different in developing countries including Pakistan. In Pakistan, the first PEM training program was started in 2017 with a two-year training structure.
There is a dire need to develop well-structured training programs in PEM that should be able to train and equip our paediatricians and/or emergency physicians with the art of managing PEM skills and to develop an understanding with all stakeholders, including the College of Physicians and Surgeon Pakistan (CPSP), Pakistan Medical and Dental Council (PMDC), Pakistan Paediatric Association (PPA), and Pakistan Society of Emergency Medicine (PSEM) to recognise the PEM as a separate speciality at the national level. At present, there is only one institutional fellowship that produces 1-2 PEM-trained physicians in a year, but the need is extremely high.
Fellowship's goal is to train our paediatricians and emergency physicians to establish robust emergency care, define key elements for PEM education and scholarships (that would close the academic gaps in PEM), establish a system with defined standards and assure ongoing communication of best practices between institutions.5 Hence creating an optimal environment and training opportunities where experienced physicians can deliver their expertise to trainees for safe, effective and time-bound management of non-serious to life-threatening childhood illnesses in busy tertiary care centres.
An efficient and well-organised/structured training program in PEM needs open access and comprehensive paediatric-focused curricula for emergency and trauma care. Furthermore, paediatric curricula currently implemented have not been evaluated and validated by independent evaluators and scholars.6-9 There should be well-defined national curricula, rooted contextually as per the Pakistani disease profile. These curricula should also help to build PEM physicians as future leaders and life-long learners with skills outside the realm of medical knowledge and practice that are required to lead EDs, manage healthcare teams, and act as a teacher and consultants to learners, the ED team, the patients and the families. PEM physicians should also customise themselves as advocates for children's rights for better healthcare and improved outcome.
Most pioneers in PEM learned by trial and error using the see one do one and teach one approach.1 However, this is a non-sustainable approach; hence the need is to establish a structured, approved, and well-documented academic program of PEM to improve our training structure and patient care (Figure 1).
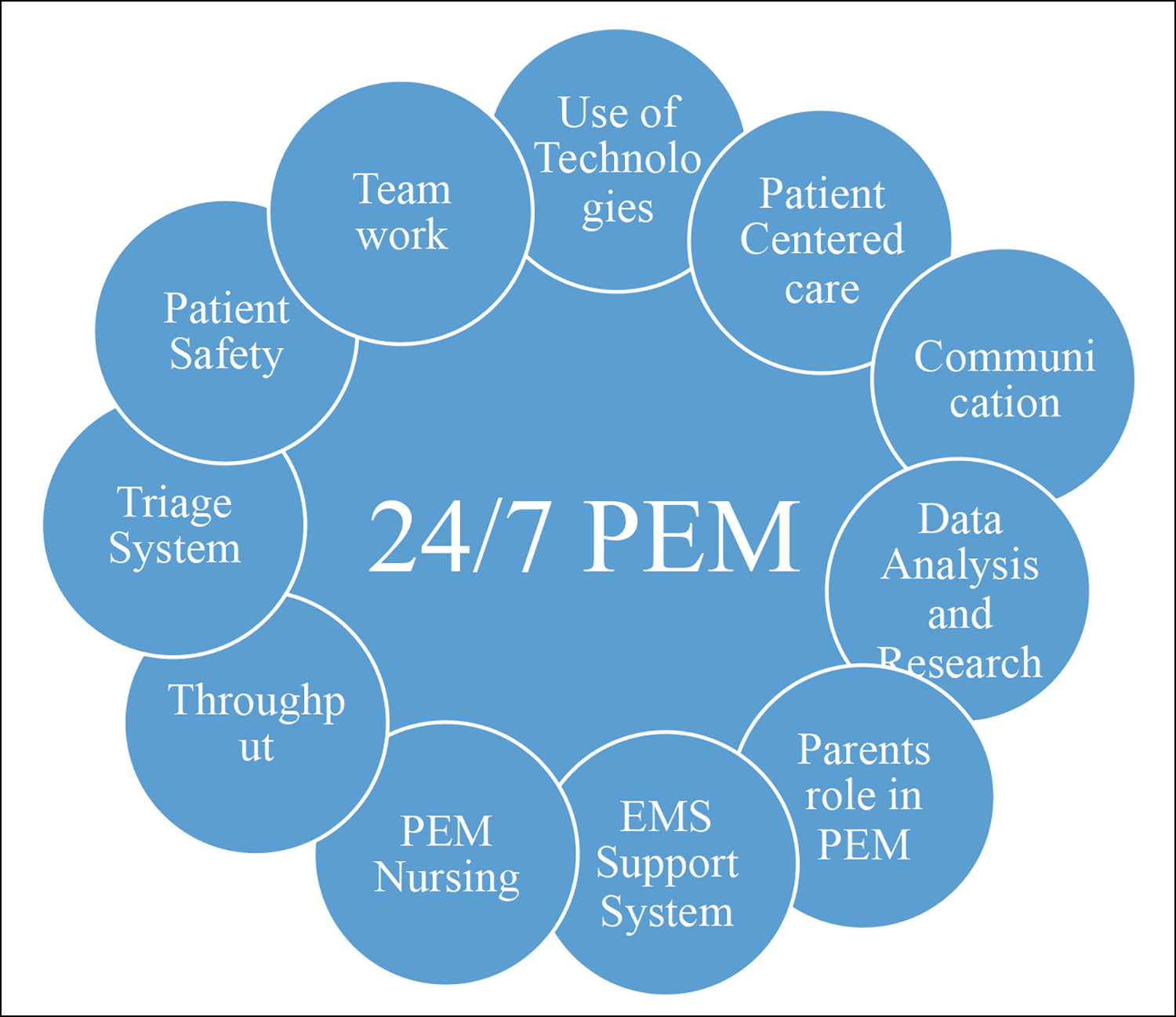 Figure I: Smooth Working of PEM.
Figure I: Smooth Working of PEM.
To establish PEM as a properly functioning and successful sub-speciality, dedicated, experienced and trained individuals with keen interest, vision, knowledge, and understanding of the subject and patient care, are needed. Pakistan, a low-middle-income country (LMIC), suffers severe financial crises and unreliable health issues at the tertiary levels, especially focusing on paediatric emergency care. With this initiative, a setup of PEM to groom and train PEM personnel, must be augmented and supported by a hierarchy from different stakes holders and the community so that we can build a better PEM for better future care.
REFERENCES
- Li M, Baker, Ropp LJ. Paediatric emergency medicine: A developing subspeciality. Paediatrics 1989; 84(2):336-42.
- Waldrop RD. A Very General overview of the development paediatric emergency medicine as a speciality in the United States and advocacy for paediatric healthcare; the charge to other countries. Adv J Emerg Med 2018; 2(1):e1. doi: 10.22114/AJEM.v0i0.39.
- UNDER-FIVE MORTALITY RATE. UN inter-agency group for child mortality estimation. [Internet].UN IGME 2020. [Cited 2021 February 2]. Available from: https://childmortality. org/data/Pakistan.
- Ijaz N, Strehlow M, Ewen Wang N, Pirrotta E, Tariq A, Mahmood N, et al. Epidemiology of patients presenting to a paediatric emergency department in Karachi, Pakistan. BMC Emerg Med 2018; 18(1):1-9. https://doi.org/10.1186/ s12873-018-0175-4.
- Klig JE, Fang A, Fox SM, Hom J, Strobel A, Tat S, et al. 2018 Academic emergency medicine consensus conference: Advancing paediatric emergency medicine education through research and scholarship. Acad Emerg Med 2018; 25(12):1327-35. doi: 10.1111/acem.13632.
- Kiragu AW, Dunlop SJ, Wachira BW, Saruni SI, Mwachiro M, Slusher T. Paediatric trauma care in low-and middle-income countries: A brief review of the current state and recommendations for management and a way forward. J Pediatr Intensive Care 2017; 6(1):52-9. doi: 10.1055/ s-0036-1584676.
- Chang MP, Walters CB, Tsai C, Aksamit D, Kateh F, Sampson J. Evaluation of a neonatal resuscitation curriculum in Liberia. Children (Basel) 2019; 6(4):56. doi: 10.3390/children6040056.
- Fant CD, Schwartz KR, Patel H, Fredricks K, Nelson BD, Ouma K, et al. Developing and implementing a paediatric emergency care curriculum for providers at district level Hospitals in sub-saharan africa: A case study in Kenya. Front Public Health 2017; 5:322. doi: 10.3389/fpubh. 2017.00322.
- Wesson HK, Plant V, Helou M, Wharton K, Fray D, Haynes J, et al. Piloting a paediatric trauma course in Western Jamaica: Lessons learned and future directions. J Pediatr Surg 2017; 52(7):1173-6. doi: 10.1016/j.jpedsurg.2017. 01.003.