Outcomes Associated with Indwelling Momentary Probe for Congenital Nasolacrimal Duct Obstruction Treatment
By Xuemei Han1, Yang Bian2, Bo Yu3Affiliations
doi: 10.29271/jcpsp.2022.12.1581ABSTRACT
Objective: To compare the outcomes of congenital nasolacrimal duct obstruction (CNLDO) patients undergoing nasolacrimal duct obstruction (NLD) probing in whom momentary probe indwelling was and was not performed.
Study Design: Randomised controlled trial.
Place and Duration of Study: Department of Orbital and Oculoplastic Surgery, Eye Hospital, Wenzhou Medical University, Wenzhou, China, from June 1, 2021, to January 30, 2022.
Methodology: Two hundred and four patients with CNLDO (217 eyes) were enrolled and underwent NLD probing. These patients were randomly assigned to undergo NLD probing with or without momentary probe indwelling. Specifically, no indwelling was performed for patients in Group A, whereas probe indwelling for 5 minutes was performed for patients in Group B. Patients were additionally separated into simple and complex CNLDO groups based on intraoperative exploration results. Preoperative characteristics, success rates, and procedure-related complications were compared among these patient groups, with the shortest follow-up time point being 6 months.
Results: In total, 205 eyes from 192 patients were included in the final study analyses. The respective success rates in Groups A and B were 92.08% and 94.23%, respectively (p = 0.541). The success rates for simple CNLDO procedures in Groups A and B were 97.65% and 96.43%, respectively (p = 0.640), whereas for complex CNLDO procedures these success rates were 62.50% and 85.00% (p = 0.146). Age, unilateral or bilateral disease, and prior dacryocyst massage were not found to be associated with the risk of operative failure.
Conclusion: While NLD probing is a beneficial treatment for children affected by CNLDO that is associated with satisfactory outcomes, momentary probe indwelling did not confer any additional benefits and is thus likely to be unnecessary.
Key Words: Congenital nasolacrimal duct obstruction, Nasolacrimal duct probing, Indwelling time.
INTRODUCTION
Congenital nasolacrimal duct obstruction (CNLDO) is one of the most prevalent ocular disorders among infants and can result in a range of clinical symptoms such as persistent epiphora, increased tear accumulation, and recurrent mucopurulent discharge.1 This condition spontaneously resolves in at least 75% of cases with conservative treatment consisting of topical antibiotics and dacryocyst massage,2,3 while nasolacrimal duct (NLD) probing has been established as a first-line treatment for the remaining 25% of patients who experience persistent CNLDO.
Reported operative success rates for this procedure range from 72-98.1%.1,2,4,5 However, the timing of such probing remains a matter of some controversy,2,3,6,7 with most researchers positing that NLD probing should ideally be performed from 9-15 months of age.6 While momentary probe indwelling has the potential to impact NLD probing outcomes, the effects of this operative technique have yet to be studied in detail. Some surgeons immediately remove the probe following NLD probing,8,9 whereas others retain the probe in the NLD for 1 minute following probing,10 and others extend this indwelling time to more than 10 minutes,11,12 positing that this can support the NLD wall, thereby improving operative success rates.
In general, researchers agree that NLD probing should be performed with patients under general anaesthesia (GA) given that physical restraints may not be sufficient to ensure that such probing can be safely performed.13,14 During extended indwelling, patients may absorb additional anaesthetic medicines, with inhaled sevoflurane being the most commonly utilised sedative in paediatric surgical settings owing to the rapidity of associated induction and elimination.15
This study aimed to compare differences in surgical outcomes for congenital nasolacrimal duct obstruction (CNLDO) patients with and without the use of momentary probe indwelling.
METHODOLOGY
The institutional ethical committee of the Eye Hospital of Wenzhou Medical University approved this study, and all patients participated in this study with the informed consent of their parents or other guardians. Cases were enrolled from June 1, 2021 to January 30, 2022 at the Eye Hospital of Wenzhou Medical University.
CNLDO patients eligible for inclusion in this study were paediatric patients 9-15 months of age with at least one symptom of NLDO (epiphora, an enlarged lacrimal lake, discharge, and/or positive fluorescein dye disappearance test [FDDT] results) who had not experienced upper respiratory infections or irritation of the ocular surface within the last 6 months. Patients were excluded if they were affected by Down syndrome, craniofacial deformities, punctal disease, or a history of eyelid dislocation, prior CNLDO surgery, or acute dacryocystitis. Patients were additionally omitted if they underwent follow-up evaluation for <6 months.
A total of 204 patients (217 eyes) were randomly assigned to two groups according to the random number table method, including Group A (101 patients, 107 eyes) and Group B (103 patients, 110 eyes). Prior to surgery, all patients were treated three times per day with topical antibiotics (0.3% Tobramycin eye drops) for 5 days.
The same surgeon (BY) performed all surgical procedures in this study. Patients were fasted as per institutional guidelines prior to sedative inhalation (clear liquids for 2 hours, breast milk for 4 hours, milk and solids for 6 hours preoperatively). After patients entered the operating room, they were subject to electrocardiogram (ECG), heart rate (HR), mean arterial pressure (MAP), and pulse oximetry (SpO2) monitoring. Patients were positioned with shoulder pads with their heads back, and 8% sevoflurane was inhaled during induction at an oxygen flow rate of 6 L/min. After patients were unconscious, anesthetization was maintained with 3-4% sevoflurane and an oxygen flow rate of 2-3 L/min, with spontaneous breathing being maintained throughout the procedure. NLD probing was then initiated.
Probing was performed via the same approach in both groups. Initially, proparacaine hydrochloride eye drops were used for the topical anesthetization of the affected eye. Following the use of a punctal dilator for punctum dilation, a No. 6 (diameter 0.6 mm) blunt, hollow, side-hole probe was attached to a 5 mL syringe filled with 2 mL of fluorescein sodium saline solution (Figure 1). The probe was then inserted into the ampulla of the lower canaliculus through the lower punctum and rotated horizontally to allow the probe to fit within the canaliculus. To prevent kink formation, the eyelid was subject to lateral traction. When a hard stop was encountered, the probe was moved back by ~1 mm, and the syringe was injected until the irrigation fluid flowed from the upper punctum, after which the probe was removed from the lower lacrimal canaliculus. This was performed to preclude the blockage of the lacrimal canaliculus and to confirm that patients were suffering from NLDO.
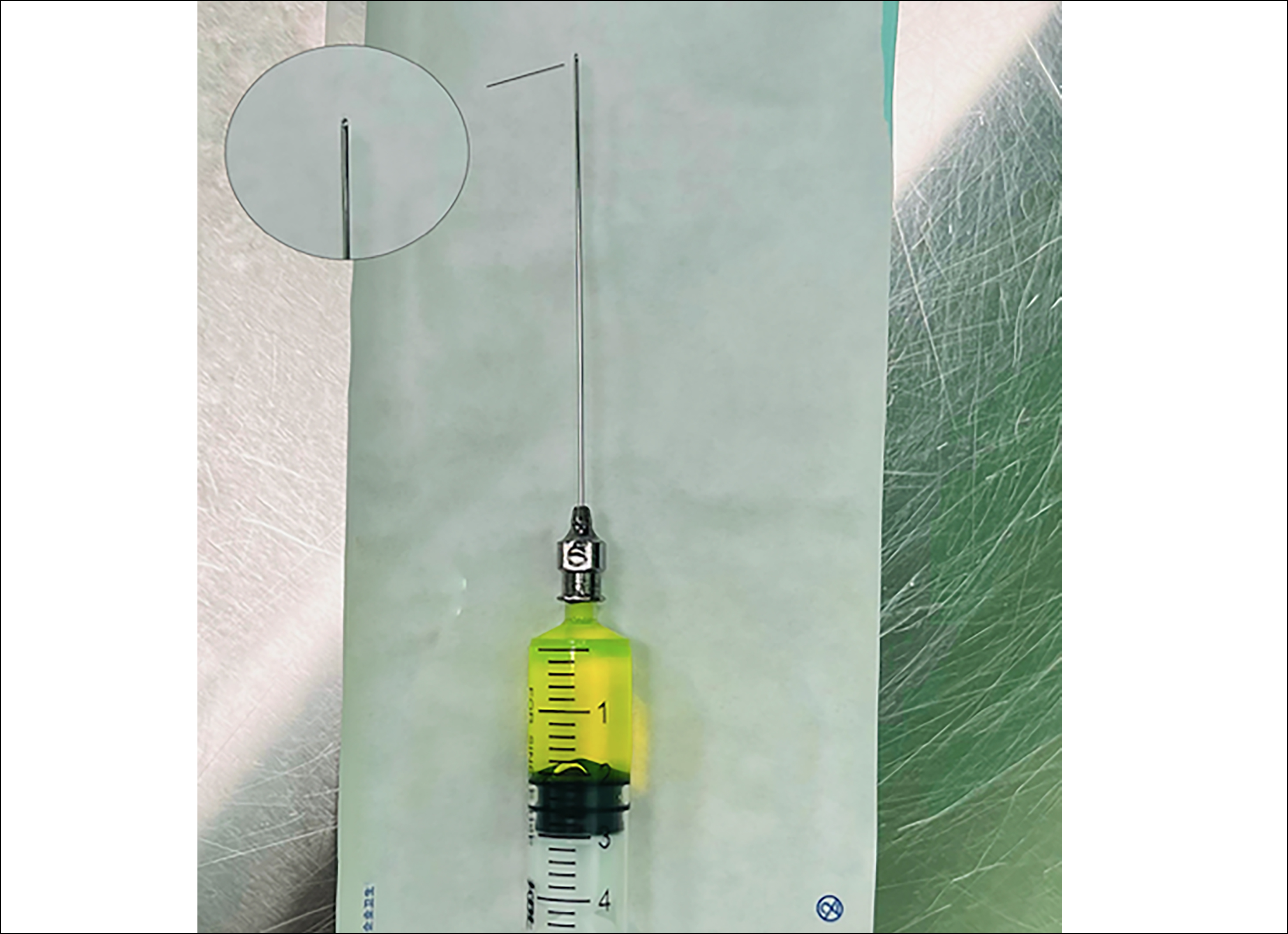 Figure 1: A No.6 probe attached to a 5 mL syringe filled with 2 mL of sodium fluorescein-stained saline solution. Magnification shows the blunt, hollow, side-hole probe.
Figure 1: A No.6 probe attached to a 5 mL syringe filled with 2 mL of sodium fluorescein-stained saline solution. Magnification shows the blunt, hollow, side-hole probe.
This same procedure was then performed for the upper punctum until encountering a hard stop, at which time the probe was rotated and advanced downward into the NLD until passing the site of the obstruction. Fluorescein irrigation was used to confirm lacrimal drainage system patency, and direct dye drainage was assessed by placing a cotton swab within the nasal cavity. The saline solution was injected slowly, with ≤2 mL being injected to prevent irrigation fluid aspiration.
After these procedures were complete, the probe was immediately removed for patients in Group A, whereas for patients in Group B the probe was removed after an additional 5-minute indwelling period (Figure 2). After the operation was complete, sevoflurane inhalation was immediately discontinued and pure oxygen was inhaled through a nasal mask until patients awoke from anaesthesia.
 Figure 2: The patient inhales sevoflurane through a mask during probe indwelling.
Figure 2: The patient inhales sevoflurane through a mask during probe indwelling.
The NLDO type in these patients was classified as either being simple, as defined by a thin film in the lower NLD that was readily bypassed by a No. 6 probe without any gritty sensation, or complex, as defined by an unusually positioned obstruction in the upper of middle layers of the NLD or a tight/thick obstruction with a gritty feeling requiring greater force to bypass, as per the criteria previously established by Al-Faky et al.8 Patients were excluded from further analyses if difficulties during probing or a lack of smooth flushing were observed during this procedure. For bilateral CNLDO patients, the right eye was probed prior to the left eye.
Antibiotic eye drops (0.3% tobramycin) were administered to all patients three times per day for 1 week postoperatively. Patient follow-up was conducted at 1 week, 1 month, 3 months, and 6 months postoperatively. At each follow-up time point, patients were evaluated for any clinical signs and symptoms, and the same testing procedures were performed (epiphora, increased tear lake, discharge, FDDT). Operative success was defined by complete NLDO symptom remission, normal tear lake height, and negative FDDT results.
SPSS 24.0 was used for all statistical testing. The Shapiro-Wilk test was used for normality analyses of the ages of the two groups of patients, revealing them to be normally distributed, and an independent sample t-test was used to compare the ages of these two groups. Other qualitative data such as gender, unilateral/bilateral, previous history of dacryocyst massage, and success rates were compared using Pearson's chi-square tests or Fisher's exact test. Quantitative variables were expressed as means and SD, while qualitative variables were expressed as counts and percentages. A p-value of < 0.05 was considered statistically significant.
RESULTS
Of the 204 consecutive CNLDO patients (217 eyes) included in this study, 12 were ultimately excluded. These included 1 and 2 patients in Groups A and B, respectively, that did not complete follow-up, as well as 5 and 4 patients in Groups A and B, respectively, that experienced difficulty during intraoperative probing. The remaining 95 patients (101 eyes) and 97 patients (104 eyes) in Groups A and B, respectively, were included in the final analyses. Participant demographic and clinical characteristics are compiled in Table I. There were no significant relationships between any of these preoperative characteristics and operative outcomes in either patient group. The operative success rates did not differ significantly between simple CNLDO cases in Group A (97.60%; 83/85) and Group B (96.43%; 81/84, p = 0.640). Similarly, no differences in operative success rates were observed when comparing complex CNLDO cases in Group A (62.50%; 10/16) and Group B (85%; 17/20, p = 0.146). Procedure success rates in these different patient groups are summarised in Table I.
In the overall study population, 169 (82.44%) and 36 (17.56%) eyes were respectively affected by cases of simple and complex CNLDO. Respective operative success rates for simple and complex CNLDO were 97% (164/169) and 75% (27/36), with a significant difference between these two classifications (p <0.001).
No patients in this study experienced complications reported in prior studies such as the tearing of the puncta or canaliculi, false channel creation, cellulitis, or irrigation fluid aspiration.
Table I: Comparisons of characteristics and success rates between experimental groups.
|
Parameter |
Group |
p-value |
|
|
A |
B |
||
|
Characteristics No. of patients / No. of eyes |
95/101 |
97/104 |
|
|
Age (mean ± SD; months) |
11.50±1.49 |
11.29±1.41 |
0.309* |
|
Male/Female, n1/n2 (%) |
46/49 (48.42 / 51.58) |
47/50 (48.45) / 51.55) |
0.996# |
|
Bilateral, n (%) |
6(6.32) |
7(7.22) |
0.804# |
|
Previous lacrimal massage eyes (%) |
80(79.21) |
79(75.96) |
0.578# |
|
Complex, eyes (%) |
16(15.84) |
20(19.23) |
0.524# |
|
Success rates |
|
|
|
|
Total eyes (%) |
93(92.08) |
98(94.23) |
0.541# |
|
Complex eyes (%) |
10(62.50) |
17(85.00) |
0.146& |
|
Simple eyes (%) |
83(97.65) |
81(96.43) |
0.640# |
|
Group A: No momentary probe indwelling; Group B: momentary probe indwelling; SD: standard deviation; *Independent samples t-test; # Pearson’s chi-square test, &Fisher’s exact test. |
|||
DISCUSSION
CNLDO occurs as a consequence of incomplete lower NLD development, incomplete ductalization, or left membranous obstruction, and it is the leading cause of epiphora among infants. Overall, an estimated 73.6-96% of cases resolve spontaneously with further development or following the compression or massage of the nasolacrimal sac.4,6,7,16,17 When discharge is present, conservative treatment for CNLDO patients consists of nasolacrimal sac massage and the application of topical antibiotics.
In CNLDO patients that fail to benefit from such conservative treatment, NLD probing is the preferred first-line interventional approach. During this procedure, a probe is advanced through the NLD and perforates the embryonic membrane, although the choice to conduct subsequent probe indwelling is at the discretion of the operating surgeon. While some surgeons immediately withdraw the probe,8,9 others withdraw it after 1 min in the NLD,10 and others conduct probe indwelling for up to 30 minutes.11,12 To examine the impact of probe indwelling on NLD probing outcomes, the present prospective randomized controlled trial was developed.
In this study, there were no significant differences in the power of Group A (92.08%) and Group B (94.23%). No significant differences in success rates were observed between these groups for simple CNLDO procedures (97.65% vs. 96.43%). This may be because simple CNLDO cases entail the obstruction of the Hasner valve at the distal end of the NLD. Probing removes this membranous obstruction, while probe indwelling has no additional impact. There were also no significant differences in complex CNLDO procedure success rates in Group A (62.5%) and Group B (85%) (p= 0.146). He et al. previously reported that probe indwelling in the NLD for 30 minutes was associated with improved operative success rates for complex CNLDO procedures,11 and proposed that this was because prolonged probe indwelling was conducive to the adequate dilation of the bony NLD lumen. In the present study, all patients underwent sevoflurane inhalation anaesthesia treatment, and the indwelling time was shortened to 5 minutes to reduce the duration of exposure to anaesthesia. This may account for the differences in results between these two studies given the dramatic difference in indwelling time. Alternatively, these results may be attributable to the small size of the complex CLNDO patient group in this study, precluding the reliable detection of differences between Groups A and B. While the probe can dilate the narrow NLD and maintain the patency of the membrane distal to the NLD, the narrow lumen and thick membrane can retract in an elastic manner following probe removal, potentially explaining why momentary probe indwelling has no impact on surgical success rates.
Here, the NLD success rates were significantly higher for cases of simple CNLDO relative to complex CNLDO (97% vs. 75%, p < 0.001), consistent with many prior studies. Kushner et al.,18 for example, reported respective operative success rates of 100% and 36% in children affected by simple and complex obstructions, while Kashkouli et al.10 reported corresponding rates of 90.2% and 33.3%.
The overall success rate in this study of 93.66% is in line with rates reported in other large case series (72%-98.1%).1,2,4,5 As young children cannot cooperate or perform lacrimal duct irrigation in the same manner as adults, CNLDO diagnostic criteria are primarily reliant on symptoms including epiphora, increased discharge, and increased tear lake levels. In this study, participants were placed under inhalation anaesthesia and the probe was inserted from the lower lacrimal canaliculus until it encountered a hard stop, after which it was retracted by ~1 mm and the lacrimal duct was flushed. This allowed for the exclusion of possible obstruction of the inferior lacrimal canaliculus and the common lacrimal duct while also confirming the CNLDO diagnosis. As the angle between the superior lacrimal canaliculus and the NLD is smaller than that between the inferior lacrimal canaliculus and the NLD, a superior lacrimal canaliculus probing procedure was herein used to minimize probe-mediated tension on the lacrimal punctum, thereby better protecting it. This likely accounts for the lack of any complications such as puncta or tear duct tearing in this case series.
No consensus regarding the optimal timing of NLD probing interventions has been established to date. While some authors suggest delaying the procedure until children are 12-13 months old given that CNLDO symptoms often spontaneously resolve,3,7 others report that delaying probing can increase the risk of fibrosis and inflammation, potentially reducing subsequent probing success rates.2 Sathiamoorthi et al. found the spontaneous CNLDO remission rate to stabilize at 9 months of age, with initial probing success rates declining after 15 months, leading to the proposal that NLD probing should ideally be performed from 9-15 months of age. In this study, 192 cases (205 eyes) of children aged 9-15 months were evaluated, with an overall operative success rate of 93.66%.6 This success rate was higher than that reported previously, in support of the conclusion established by Sathiamoorthi et al.6
Here, no differences in operative success rates were observed as a function of whether patients exhibited bilateral or unilateral disease. This is in contrast to the data published by Miller et al.,19 who reported significantly lower success rates for bilateral exploration (63%) than for unilateral exploration (80%), with this difference having been attributed to the increased amount of time required to probe both eyes while patients were restrained and under local anaesthesia, making this procedure more challenging when children are held in place by physical constraints. For the present study, all procedures were performed under general anaesthesia, thus eliminating these difficulties and supporting the explanation proposed by Miller et al.
The anesthetisation approach also remains controversial in the context of NLD probing. Some researchers have remarked that in-office probing performed under physical restraint is more convenient,14,20 whereas others suggest that GA should be used given that physical restraint may not be sufficient to ensure that the procedure can be safely completed.21 Inhalation anaesthesia was used in the present study, with sedation having been achieved via the inhalation of sevoflurane through a mask. Sevoflurane exhibits a low blood/gas partition coefficient (0.69) that results in its more rapid absorption and elimination.15 Adverse events associated with recovery from sevoflurane-associated anaesthesia include nausea/vomiting, coughing, and agitation/delirium, although no such events were reported during or after NLD procedures for patients in this study.
In general, NLD probing is not associated with high complication rates, with only limited reports of puncta or nosebleeds following probing or instances of procedure failure associated with persistent tearing and mucus discharge. However, no patients in the present study cohort experienced any of these negative procedure-related outcomes.
While the prospective, randomised, and blinded nature of the outcome assessments in this study reinforce these conclusions, these results are nonetheless subject to certain limitations. For one, the study sample size was limited, particularly for eyes affected by complex CNLDO, potentially contributing to the lack of observed significance for these results. Second, the classification of CNLDO type (simple vs. complex) is primarily based on the subjective experience of the surgeon as they advance the probe through the NLD, and these classifications may thus not be generalizable.
CONCLUSION
The results of this study suggest that momentary probe indwelling is unnecessary when performing NLD probing in patients with both simple and complex CNLDO. However, additional large-scale prospective randomised comparative trials will be necessary to firmly establish the optimal approach to treating patients affected by this condition.
ETHICAL APPROVAL:
The study was approved by the institutional ethical committee of the Eye Hospital of Wenzhou Medical University (Approval No. 2021-105-K-89-01).
PATIENTS’ CONSENT:
Written informed consent were obtained from all patients’ guardians.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
XH: Research design, statistical analysis, and manuscript writing.
YB: Disease diagnosis and postoperative follow-up.
BY: Research design, surgical procedures, and manuscript writing.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Schnall BM. Pediatric nasolacrimal duct obstruction. Current Opinion in Ophthalmol 2013; 24(5):421-4. doi: 10. 1097/ICU.0b013e3283642e94.
- Robb RM. Success rates of nasolacrimal duct probing at time intervals after 1 year of age. Ophthalmology 1998; 105(7):1307-10. doi: 10.1016/S0161-6420(98)97038-5.
- Świerczyńska M, Tobiczyk E, Rodak P, Barchanowska D, Filipek E. Success rates of probing for congenital nasolacrimal duct obstruction at various ages. BMC Ophthalmology 2020; 20(1):403. doi: 10.1186/s12886- 020-01658-9.
- Arora S, Koushan K, Harvey JT. Success rates of primary probing for congenital nasolacrimal obstruction in children. J American Association for Pediatric Ophthalmology Strabismus 2012; 16(2):173-6. doi: 10.1016/j.jaapos. 2011.12.151.
- Limbu B, Akin DM, Saiju R. Age-based comparison of successful probing in Nepalese children with nasolacrimal duct obstruction. Orbit 2010; 29(1):16-20.doi: 10.3109/ 01676830903207844.
- Sathiamoorthi S, Frank RD, Mohney BG. Spontaneous resolution and timing of intervention in congenital nasolacrimal duct obstruction. JAMA Ophthalmology 2018; 136(11):1281-6. doi: 10.1001/jamaophthalmol.2018.3841.
- MacEwen CJ, Young JD. Epiphora during the first year of life. Eye 1991; 5(5):596-600. doi: 10.1038/eye.1991.103.
- Al-Faky YH, Mousa A, Kalantan H, Al-Otaibi A, Alodan H, Alsuhaibani AH. A prospective, randomised comparison of probing versus bicanalicular silastic intubation for congenital nasolacrimal duct obstruction. British J Ophthalmology 2015; 99(2):246-50. doi: 10.1136/ bjophthalmol-2014-305376.
- Serin D, Buttanri IB, Sevim MS, Buttanri B. Primary probing for congenital nasolacrimal duct obstruction with manually curved Bowman probes. Clinical Ophthalmology (Auckland, NZ). 2013; 7:109-12. doi: 10.2147/OPTH.S39926.
- Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z. Late and very late initial probing for congenital nasolacrimal duct obstruction: What is the cause of failure? British J Ophthalmology 2003; 87(9):1151-3. doi: 10.1136/bjo.87.9.1151.
- He L, Liu Y, Tao X, Cen C. Clinical analysis of lacrimal passage combined with indwelling probe applied gatifloxacin gel in the treatment of infants older than 6 months with complicated nasolacrimal duct obstruction. Chinese J General Practice 2019; 17(9):1491-4. doi:10 .16766 /j.cnki.issn.1674-4152. 000977.
- Zhang H, Yang S, Xie XL, Qiu GZ, Gong YQ. Outcome of probing combined with probe retshling for complex congenital uasolacrimal duct obstruction. Chinese J Strabismus Pediatric Ophthalmology 2010; 18(4):182-5. doi: 10.3969/j.jssn.1005-328X.2010.04.016.
- Lee C, Jeong SM, Kim GJ, Joo EY, Song MH, Sa HS. Efficacy and safety of inhalation sedation during office probing for congenital nasolacrimal duct obstruction. J Clinical Medicine 2021; 10(8):1800. doi: 10.3390/jcm10081800.
- Basar E, Oguz H, Ozdemir H, Cicik E, Mirzatas C, Basarer T, et al. Outcome of office probing and irrigation under topical anaesthesia for congenital nasolacrimal duct obstruction. Annals Ophthalmol 2005; 37(2):95-8. doi: doi-org-443. bjmuilibs.cn/10.1385/AO:37:2:095.
- Brioni JD, Varughese S, Ahmed R, Bein B. A clinical review of inhalation anaesthesia with sevoflurane: from early research to emerging topics. J Anaesthesia 2017; 31(5):764-8. doi: 10.1007/s00540-017-2375-6.
- Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmolog 1987; 94(6):698-705.doi: 10.1016/s0161- 6420(87)33392-5.
- Pediatric eye disease investigator group. Primary treatment of nasolacrimal duct obstruction with probing in children younger than 4 years. Ophthalmology 2008; 115(3): 577-84. doi: 10.1016/j.ophtha.2007.07.030.
- Kushner BJ. The management of nasolacrimal duct obstruction in children between 18 months and 4 years old. J American Association Pediatric Ophthalmology Strabismus 1998; 2(1):57-60. doi: 10.1016/s1091-8531(98)90112-4.
- Miller AM, Chandler DL, Repka MX, Hoover DL, Lee KA, Melia M, et al. Pediatric eye disease investigator group. Office probing for treatment of nasolacrimal duct obstruction in infants. J American Association Pediatric Ophthalmology Strabismus 2014; 18(1):26-30. doi: 10. 1016/j.jaapos.2013.10.016.
- Kassoff J, Meyer DR. Early office-based vs. late hospital-based nasolacrimal duct probing: A clinical decision analysis. Archives Ophthalmology 1995 1; 113(9):1168- 71.doi: 10.1001/archopht.1995.01100090094028.
- Clark RA. Dilation probing as primary treatment for congenital nasolacrimal duct obstruction. J American Association Pediatric Ophthalmology Strabismus 2002; 6(6):364-7. doi:10.1067/mpa.2002.128210.