Mucormycosis of Maxilla: An Enigma to the Clinician
By Suman SenAffiliations
doi: 10.29271/jcpsp.2022.09.1219ABSTRACT
Mucormycosis is an acute opportunistic infection caused by a saprophytic fungus found in the soil, decaying fruits, and vegetables. It is a rapidly progressing fungal infection mainly seen in nose and its surrounding sinuses due to inhalation of the spores of fungus from the contaminated areas. If not diagnosed and treated early, it can be life-threatening. A case of a 60-year male farmer is reported with an extensive spread of the fungal infection involving alveolar bone of maxilla, zygomatic process, and the right orbit. The radiographs demonstrated alveolar, palatal, and zygomatic bone destruction. The diagnosis of mucormycosis was made through clinical, radiographic, and histopathologic findings. An early diagnosis and treatment with antifungal drugs like amphotericin B and surgical resection can improve the prognosis.
Key Words: Mucormycosis, Maxilla, Zygomatic bone, Antifungal.
INTRODUCTION
Mucormycosis is a rare emerging fungal infection seen in the oral cavity with a high mortality and morbidity. Mucormysosis is one of the rapidly spreading fungal infection that can invade the bony structures. It is caused by the organisms of Mucorales order among the class of Zygomycetes. There are more than 25 species that infect humans. It is an angio-invasive fungal disease. The incidence of mucormycosis is rising at a rapid rate in the Southeast Asian countries.1 The increase in the cases of Mucormycosis is perceived globally, but it is very high in the Asian continent.2
Mucormycosis represents the third most common angio-invasive fungal infection following candidiasis and aspergillosis.3 Immunocompromised patients with severe underlying diseases, such as hematologic malignancies, transplantation, uncontrolled diabetes mellitus, severe trauma, burns, and individuals on long-term steroid therapy are more prone to be affected by mucormycosis.4,5 The diagnosis of Mucormycosis is based on the clinical suspicion, recognition of host factors, and prompt assessment of the clinical and radiological findings in order to improve the survival.
CASE REPORT
A 60-year male farmer came to the dental hospital with the chief complaint of pain and ulceration over the right side of the face and inside the oral cavity for the last 5 months.
The patient was asymptomatic initially, the pain started 2 months back and was gradually increasing with difficulty in eating. One month back, his right upper 1st and 2nd molar teeth became mobile and got exfoliated. He also complained of reduced smell sensation and eyesight for the last 10 days. His medical and family history was non-contributory. The extra-oral examination revealed diffuse swelling over the face with single ulcerative necrotic area measuring around 0.5 cm in diameter seen over right side of the face, 1 cm below the pupil of the eye (Figure 1). On palpation, it was tender and soft to firm in consistency. Intra-oral examination showed complete maxillary edentulous arch and yellowish ulcerative necrosis of hard palate (Figure 2) and alveolar mucosa with exposure of underlying bone of entire alveolar ridge of maxillary arch extending to the maxillary tuberosity (Figure 3). There was oroantral communication in the right molar region (Figure 2).
A maxillary occlusal radiograph showed destruction of buccolingual cortical plates along with bony tooth sockets of the entire maxillary arch. Computed Tomography (CT) scan (Figure 4) revealed homogeneous density mass with the destruction of zygomatic and pterygoid processes of maxilla along with the right lateral wall of orbit. Hard palate osteolysis was noted on right side. Hyperdensity of the maxillary antrum with destruction of the right nasal wall was seen. Radiography was suggestive of rhinocerebral mucormycosis. Based on the clinical findings and the patient’s history, it was provisionally diagnosed as mucormycosis of maxilla and zygoma with differential diagnoses of osteomyelitis and granulomatous disease.
A biopsy was performed under local anaesthesia from the tooth socket of the alveolar ridge and palatal mucosa. Microscopy identified the presence of broad, non-septate hyphae with the right-angle branching within necrotic areas. The patient was advised for intravenous administration of Amphotericin B for 7 days at 5 mg/Kg/day in combination with the surgical intervention.
 Figure 1: Facial profile showing diffuse swelling of the right side of face with necrotic ulcerative lesion in the region zygomatic arch.
Figure 1: Facial profile showing diffuse swelling of the right side of face with necrotic ulcerative lesion in the region zygomatic arch.
 Figure 2: Ulcerative necrosis of hard palate exposing the underlying bone with oroantral communication in the right molar region.
Figure 2: Ulcerative necrosis of hard palate exposing the underlying bone with oroantral communication in the right molar region.
DISCUSSION
Mucormycosis is a relatively uncommon invasive fungal infection that is seen in the oral cavity. The most common clinical presentation of infection is rhino-orbito-cerebral mucormycosis, as in the present case. It involved the sinuses, orbital wall, zygoma, and oral cavity leading to the fever, swelling of one side of the face, and lesions inside the mouth and outside on the face. Other types can be pulmonary mucormycosis that affects the lungs leading to the chest pain, disturbance in breathing, fever, and cough; cutaneous mucormycosis that causes local skin infections leading to the ulcers or blisters, redness and swelling of the infected skin region; gastrointestinal mucormycosis that is commonly seen among the premature neonates leading to the nausea, vomiting, gastrointestinal bleeding, and abdominal pain; and disseminated mucormycosis seen in the patients suffering from the multiple medical complications hindering the symptomatic discrimination of mucormycosis from other infectious diseases.6 It is caused by the asexual spores of fungi. The tiny spores come in contact with the oral or nasal mucosa and cause germination. Then the fungal hyphae invade the blood vessels that can lead to thrombosis, ischemia, infarction with dry gangrene and necrosis.7 Occasionally, it maybe seen in the individuals without any debilitating conditions that compromise cellular and humoral defense mechanisms. In this case, the patient had a history of laceration over the right lips and by occupation he was a farmer with direct contact with soil. The maxilla is not commonly affected by mucormycosis since it has good blood supply due to the numerous blood vessels surrounding the maxillofacial region. In this case, it involved the maxilla and zygomatic region. In the initial stages, rhinocerebral mucormycosis may resemble bacterial sinusitis and malignancy.
 Figure 3: Necrotic bone of entire alveolar ridge of maxilla.
Figure 3: Necrotic bone of entire alveolar ridge of maxilla.
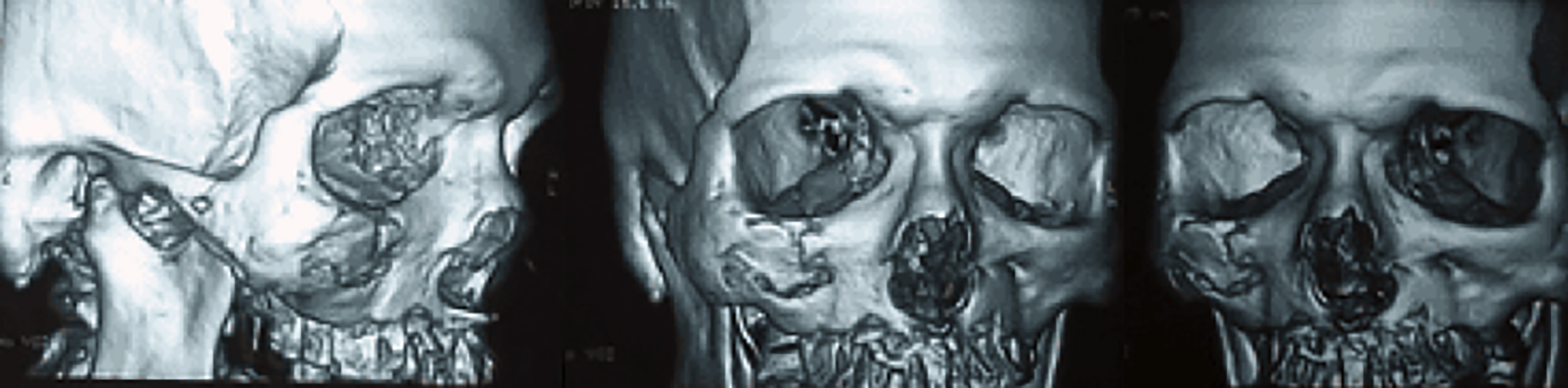 Figure 4: CT scan showing bone involvement of maxilla and zygomatic arch.
Figure 4: CT scan showing bone involvement of maxilla and zygomatic arch.
The treatment of mucormycosis is quite limited and only two classes of molecules; polyenes and azoles are currently used in the clinical practice. Amphotericin B is considered the drug of choice for the primary treatment of mucormycosis with a dose of 5 mg/Kg/day.8 Newer triazoles like posaconazole, 400 mg BID and isavuconazole, 200 mg TID, act by depleting ergosterol from the fungal cell membrane and can be used as salvage therapy in patients unresponsive or intolerant to Amphotericin B.8,9 It is a life-threatening condition with a mortality rate of around 50%, if localised, and can be as high as 70–90%, if it spreads to adjacent regions and involves other organs. The prognosis ranges from fair to poor.10 No standard protocol and duration of antifungal drugs exist presently for the treatment. Surgical removal of infected necrotic tissues is important in the treatment of rhino-orbito-cerebral disease. Open surgeries are preferred for extensive disease that may include maxillectomy orbital exenteration, and craniofacial resection.8 A multidisciplinary approach is needed for the prompt diagnosis and management of mucormycosis.11 Early diagnosis and treatment help to limit the mortality rate. It can be cured by the combination of surgical removal of the affected areas along with the systemic administration of the combination of lipid formulations of amphotericin B.
PATIENT’S CONSENT:
Informed consent is obtained from the patient to publish the data concerning this case.
COMPETING INTEREST:
The author declared no competing interest.
AUTHOR’S CONTRIBUTION:
SS: Contributed to the conception of the work, collected the patient data and images, did literature review, wrote the manuscript, and approved the final version to be published.
REFERENCES
- Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, Savio J, et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med Mycol 2019; 57(4):395-402. doi: 10.1093/ mmy/myy060.
- Prakash H, Chakrabarti A. Global epidemiology of mucormycosis. J Fungi (Basel) 2019; 5(1):26. doi: 10.3390/ jof5010026.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect 2019; 25(1):26-34. doi: 10.1016/j.cmi.2018.07.011.
- Nucci M, Engelhardt M, Hamed K. Mucormycosis in South America: A review of 143 reported cases. Mycoses 2019; 62(9):730-8. doi: 10.1111/myc.12958
- Chakrabarti A, Singh R. Mucormycosis in India: Unique features. Mycoses 2014; 57(Suppl 3):85-90. doi: 10. 1111/myc.12243.
- Hassan MIA, Voigt K. Pathogenicity patterns of mucormycosis: Epidemiology, interaction with immune cells and virulence factors. Med Mycol 2019; 57 (Suppl 2): 245-56. doi: 10.1093/mmy/myz011.
- Afroze SN, Korlepara R, Rao GV, Madala J. Mucormycosis in a diabetic patient: A case report with an insight into its pathophysiology. Contemp Clin Dent 2017; 8(4):662-6. doi: 10.4103/ccd.ccd_558_17.
- Sipsas NV, Gamaletsou MN, Anastasopoulou A, Kontoyiannis DP. Therapy of mucormycosis. J Fungi (Basel) 2018; 4(3):90. doi: 10.3390/jof4030090.
- Marty FM, Ostrosky-Zeichner L, Cornely OA, Mullane KM, Perfect JR, Thompson GR, et al. Isavuconazole treatment for mucormycosis: A single-arm open-label trial and case-control analysis. Lancet Infect Dis 2016; 16(7):828-37. doi: 10.1016/S1473-3099(16)00071-2.
- Sahota R, Gambhir R, Anand S, Dixit A. Rhinocerebral mucormycosis: Report of a rare case. Ethiop J Health Sci 2017; 27(1):85-90. doi: 10.4314/ejhs.v27i1.11.
- Serris A, Danion F, Lanternier F. Disease Entities in Mucormycosis. J Fungi (Basel) 2019; 5(1):23. doi: 10. 3390/jof5010023.