Laboratory Evaluation and Pathological Features of Bone Marrow Metastasis in Non-haematological Malignancies
By Noman Anjum Rana1, Asad Mahmood1, Helen Mary Robert1, Saima Zahir1, Muhammad Bilal Asghar1, Sana Riaz2
Affiliations
doi: 10.29271/jcpsp.2022.10.1367ABSTRACT
This study aimed to analyse the diagnostic accuracy of different laboratory parameters that can predict bone marrow metastasis. A cross-sectional analytical study was conducted at the Armed Forces Institute of Pathology (AFIP), Rawalpindi from March 2021 to August 2021. Bone marrow aspirates and biopsy procedures were done on 60 newly diagnosed cases of non-haematological malignancies as part of staging. Laboratory parameters noted for the study included peripheral blood smear findings, serum lactate dehydrogenase (LDH), radiological findings, and bone marrow aspirate/trephine biopsy results. Bone marrow metastasis was seen in 21/60 patients. The most common malignancies with bone marrow involvement were retinoblastoma and neuroblastoma. Laboratory findings showed no significant statistical difference in mean haemoglobin and total leukocyte count between cases and controls. Positive cases had a mean platelet count of 261.7 x 109/L and mean LDH of 750.1 U/L (p <0.05) for both parameters. ROC analysis showed the area under the curve (AUC) for LDH to be 0.969 (highly significant) showing a strong predictive value of LDH. Positive radiological findings were detected in only one case with bone marrow metastasis. The elevated level of serum LDH is not only cost-effective but also has high diagnostic accuracy to predict bone marrow metastasis.
Key Words: Bone marrow, Biochemical, Lactate dehydrogenase, Metastasis, Non-haematological malignancies.
Bone marrow aspirate and biopsy are routinely performed for diagnosis of haematological malignancies as well as for bone marrow involvement by non-haematologic malignancies.1 Bone marrow involvement by nonhaematologic malignancies though rare, it is important to diagnose and establish bone marrow involvement at the earliest as this influences the stage of disease, response to treatment, and overall patient survival. Bone marrow aspirate is mostly indicated for staging purposes in patients with known primary tumours, abnormal findings on peripheral blood (e.g. unexplained cytopenias), and development of nonspecific symptoms.2 The objective of this study was to analyse laboratory parameters including haematological and biochemical parameters that can predict bone marrow metastasis.
A cross-sectional analytical study was conducted at the Armed Forces Institute of Pathology (AFIP), Rawalpindi, from March 2021 to August 2021 after approval from the ethical review committee. Patients who underwent bone marrow biopsies for the staging of newly diagnosed non-haematological malignancies were included. All cases of leukaemias and lymphomas were excluded from the study. Patients with known primary tumours and no prior therapy (chemotherapy/radiotherapy) were included in the study. Patients were divided into controls and cases based on the absence and presence of bone marrow infiltration respectively. Controls and cases included 39/60 and 21/60 patients respectively.
Factors noted for laboratory evaluation included haematologic parameters (complete blood counts (CBC) assessed on Sysmex XN-3000 automated haematology analyzer, peripheral blood film findings, biochemical (serum Lactate Dehydrogenase) on Advia-1800 chemistry analyzer, radiological findings (if any), and bone marrow findings. Anaemia was defined as haemoglobin (Hb) less than 13g /dL in males and less than 12g /dL in females. Thrombocytopenia was defined as platelet count (Plt) less than 150 x 109/L. Leukocytosis and leukopenia as total leukocyte count (TLC) more than 10 x 109/L and less than 4 x 109/L respectively. BMA was performed after counselling and getting signed consent from the patients or guardians in case of children. The procedure was carried out under strict aseptic measures. Aspirates and imprints were stained with Leishman stain. Trephine biopsies were adequately fixed, decalcified, processed, and stained with haematoxylin-eosin and reticulin stains. The World Health Organization (WHO) adequacy criterion of 1.5 cm was used for trephine biopsies. After microscopic examination parameters noted were cellularity, megakaryocytes, presence / absence of tumour cells, pattern of infiltration, fibrosis, and immunohistochemistry.
Statistical analysis was done using SPSS version 26.0 in windows 10. Quantitative variables were expressed as mean and standard deviation and qualitative variables as frequencies and percentages. An independent sample t-test was run to assess the statistically significant difference in variables between cases and controls. A p-value less than 0.05 was considered statistically significant. The diagnostic utility was calculated using a receiver operating characteristic curve (ROC). A cut-off value was determined with the most optimal sensitivity and specificity to predict bone marrow metastasis.
A total of 1259 bone marrow aspirates and biopsies were performed. Out of these, 60 (4.7%) were done as a part of staging for non-haematologic malignancies and selected for the study. The mean age of patients was 12.9 years (0.5-64 years). Forty-eight (80%) patients were Children (age less than 18 years) and 12 (20%) patients were adults. Male-to-female ratio was 1.5 (36/24).
In 21/60 cases (35%) patients had bone marrow metastasis by non-haematologic malignancies. Males included 9 patients and females were 12 with a male-to-female ratio of 0.75. The most common primary tumours with bone marrow metastasis were retinoblastoma (n=6), neuroblastoma and ganglioneuroma (n=5 each), Ewing’s sarcoma, and carcinoma breast (n=3 each). Out of 21 positive cases, anaemia was present in 14 (66%), bicytopenia in 5 (23%), pancytopenia, and leucoerythroblastic picture in 1 (4.7%) patient each. On physical examination, the most frequent positive findings were pallor in 10 (47%) patients and hepatosplenomegaly in 3 (14%) of patients. Only one patient with positive bone marrow metastasis had positive changes on radiological investigation.
In patients with bone marrow metastasis, the mean LDH level was 750.1+329.0 U/L as compared to the mean LDH 265.6+86.6 U/L in patients without metastasis. The independent sample t-test revealed no statistically significant difference in Hb (p=0.26) and TLC (p=0.73). Serum LDH levels and platelet counts both showed a significant difference between cases and controls (p <0.05, Table I).
An ROC curve was applied and the area under curve (AUC) was used to find out the diagnostic accuracy of haematological and biochemical variables. AUC for Hb, TLC, and Plt was non-discriminating with values of 0.400, 0.507, and 0.357 respectively. AUC for LDH was 0.969 (highly significant than haematological variables). A cut-off value of LDH >410 U/L had a sensitivity of 86%, specificity of 92%, and a likelihood ratio of 11.1 (Figure 1).
Table I: Comparison of haematological and biochemical findings between cases and controls.
|
Laboratory findings |
Cases |
Controls |
p-value |
|
Haemoglobin g/dL |
9.8 + 1.8 |
10.4 + 1.7 |
0.26 |
|
Total leukocyte count a/L |
8.8 + 3.4 |
9.2 + 3.5 |
0.73 |
|
Platelet count a/L |
261.7 + 159.6 |
360 + 166 |
0.03 |
|
LDH U/L |
750.1 + 329 |
265.6 + 86.6 |
<0.001 |
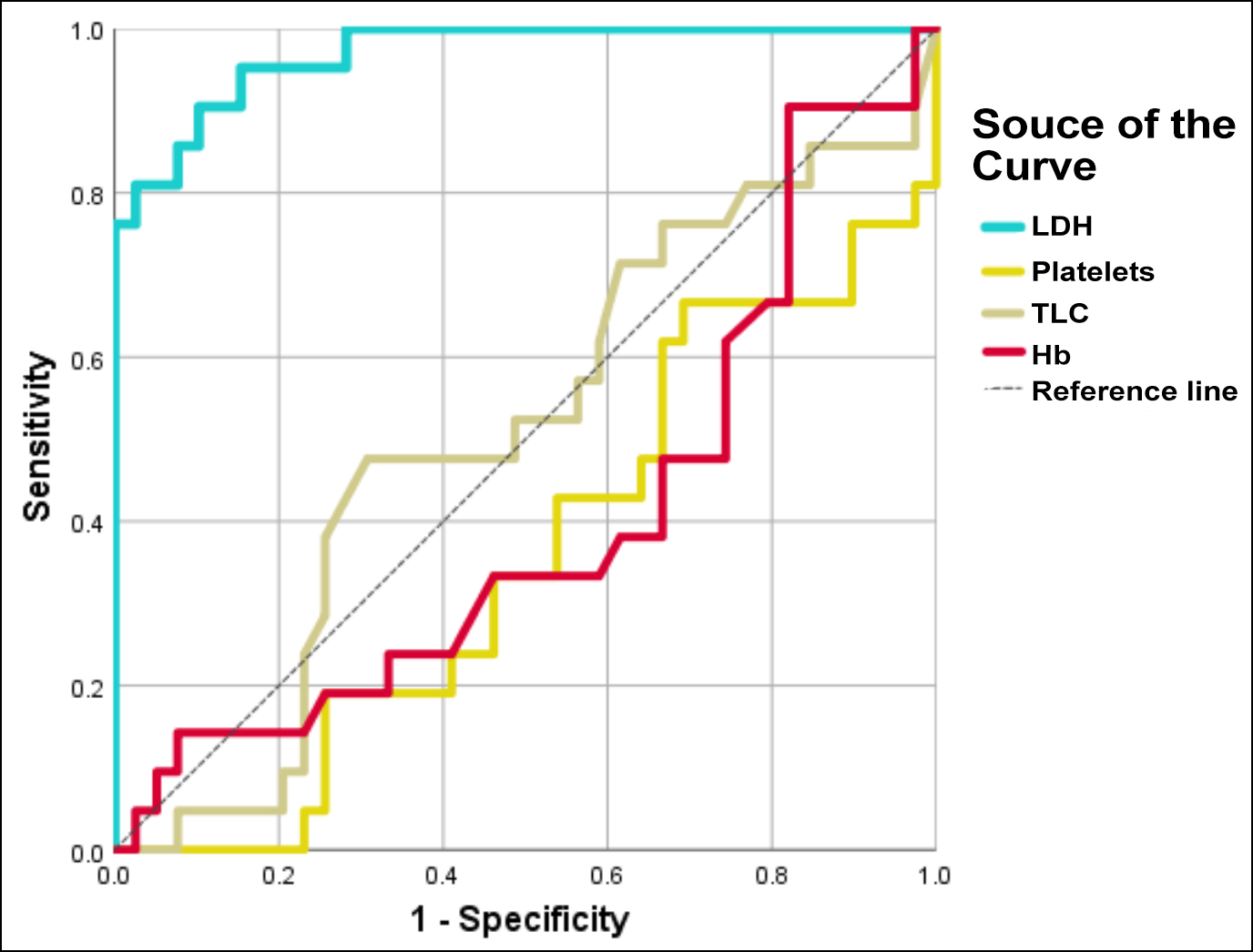 Figure 1: ROC curve analysis from SPSS (version 26.0) for lactate dehydrogenase (LDH), haemoglobin (Hb), total leucocyte count (TLC) and Platelet count (Plt).
Figure 1: ROC curve analysis from SPSS (version 26.0) for lactate dehydrogenase (LDH), haemoglobin (Hb), total leucocyte count (TLC) and Platelet count (Plt).
The closer the line towards the upper left corner, the higher the area under curve (AUC) and higher is the diagnostic accuracy. (Dotted line) shows reference line, (Blue line) shows AUC for LDH 0.969.
Bone marrow involvement by non-haematologic malignancies is a sporadic finding. Advancements in imaging techniques and techniques such as fluorodeoxyglucose-positron emission tomography (FDG-PET) has revolutionised the early diagnosis of bone marrow involvement. However, bone marrow examination is the most economical and easy method for confirmation of marrow infiltration.2 Early detection of marrow involvement is significant for the staging of the tumour and overall disease prognosis. Main indications for bone marrow examination are clinical (bone pains, pathological fractures), haematologic (cytopenias, atypical cells, leucoerythroblastic blood picture), radiological (lytic/sclerotic lesions), and biochemical (elevated levels of serum calcium, alkaline phosphatase, or lactate dehydrogenase).2,3 LDH levels are used in monitoring both haematologic and non-haematologic malignancies. High levels of serum LDH are associated with poor prognosis and metastasis.4
In this study, 60/1259 bone marrow aspirates and biopsies were performed for non-haematologic malignancies with a male-to-female ratio of 1.5. Only 21/60 (35%) cases had bone marrow involvement. Peripheral blood smear showed anaemia and bicytopenia to be the most frequent findings. LDH levels were higher in positive cases (mean 750.1 U/L) as compared to negative cases (mean 265.6 U/L) and had a p-value of <0.001, thus establishing a significant difference between positive and negative cases.
Epidemiological studies have shown organ-specific patterns of bone marrow metastasis, this idea led to the formulation of the seed-and-soil hypothesis by Paget in 1889, highlighting a specific organ microenvironment that leads to the development of metastasis.5
Elevated levels of serum lactate dehydrogenase (LDH) not only indicate a suspected bone marrow infiltration but are also used for metastatic disease prognosis.3,5 Agrawal et al., showed that high serum LDH had highly significant AUC (0.9) with sensitivity (68%), specificity (90%), and likelihood ratio (6.8) at a cut-off value >452 U/L in predicting bone marrow metastasis.1 Biochemical changes other than LDH studied and shown to predict bone marrow metastasis include serum calcium, alkaline phosphatase (ALP), hypomagnesemia and hypoproteinemia.6
Limitations to this study include the small number of patients, a limited spectrum of malignancies, and only LDH included in biochemical parameters. More biochemical parameters may be included for concordance studies. The scope of study needs to be more than an institutional study.
The mean LDH value in positive cases was 750.1 U/L and 265.6 U/L in negative cases with a statistically significant p-value (<0.001). Studies of diagnostic accuracy by ROC analysis and AUC also showed serum LDH to be superior to haematological variables (haemoglobin, total leukocyte count, and platelet count) in predicting bone marrow metastasis. Early diagnosis of bone marrow metastasis is of therapeutic as well as prognostic significance and may alter the future course of the disease.
ETHICAL APPROVAL:
Ethical approval was given by the Institutional Review Board (IRB), Armed forces Institute of Pathology (AFIP) at the IRB meeting held on 03-Feb-2021. (IRB/22/875; dated: February 03, 2021)
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
NAR: Conceived and designed study along with data collection, statistical analysis and result compilation.
AM, HMR: Data collection, results, discussion, and literature review.
SZ, MBA, SR: Discussion and literature review.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Agrawal S, Bhandari R, Gowda VN, Gupta A, Singh N, Chowdhury N, et al. Haematological and biochemical predictors of bone marrow metastases in non-haematological malignancies: A clinico-pathological analysis. J Med Evidence 2022; 3(2):123-9. doi: 10.4103/ JME.JME_129_20.
- Chauhan K, Jain M, Grover S, Shukla P, Rusia U, Grover RK. Bone marrow metastasis in nonhematologic malignancies: Data from a cancer hospital. Clinical Cancer Investigation J 2016; 5(2):103. doi: 10.4103/2278-0513.177131.
- Brahmbhatt B, Parikh B, Shah M. Bone marrow involvement by metastatic solid tumours. Gujarat Med J 2014; 69(2): 54-7.
- Udristioiu A, Cojocaru M. Relationship between LDH and Mg in monitoring of hematological and non-hematological malignant diseases. Blood 2021; 138(1):4920. https:// doi.org/10.1182/blood-2021-144320.
- Wu MY, Li CJ, Yiang GT, Cheng YL, Tsai AP, Hou YT, et al. Molecular regulation of bone metastasis pathogenesis. Cell Physiol Biochem 2018; 46(4):1423-38. doi: 10.1159/000 489184.
- Kaplinsky C, Alon US. Magnesium homeostasis and hypomagnesemia in children with malignancy. Pediatr Blood Cancer 2013; 60(5):734-40. doi: 10.1002/pbc.24460.