Karachi Cancer Registry (KCR): Consolidated Data of 5-years 2017-2021
By Shahid Pervez1, Adnan A. Jabbar2, Ghulam Haider3, Muhammad A. Qureshi4, Shamvil Ashraf5, Fouzia Lateef6, Muhammad Khurshid2, Imtiaz Bashir7, Manzoor Zaidi8, Naureen Mushtaq2, Zehra Fadoo2, Mohammed S. Quraishy9, Nausheen Yaqoob10, Ejaz Alam11, Huma Qureshi11Affiliations
doi: 10.29271/jcpsp.2023.05.560ABSTRACT
Objective: To collect and analyse epidemiologic data of all malignancies by age group and gender for the Karachi population to estimate the cancer incidence of 5-years (2017-2021) and identify major risk factors for setting priorities towards cancer control programs.
Study Design: Observational study.
Place and Duration of the Study: Karachi Cancer Registry (KCR) Secretariat, Pakistan Health Research Council (PHRC), JPMC, Karachi, from 2017-2021.
Methodology: Cancer data of seven tertiary care hospitals of Karachi submitted to KCR during the study period were analysed including age, gender, date of first contact, primary site and ICD coding. All the data was cleaned, merged, and analysed. All patients 0-14 years were classified as ‘children’, all aged 15-19 years were classified as ‘adolescents’, and those age 20-years and above as ‘adults’. Age standardised incidence rates (ASIR) were determined for both genders.
Results: During the last five years (2017-2021), a total of 65,886 malignant cases were received. The distributions seen amongst males and females were 33,510 (51%) and 32,376 (49%), respectively with 60,145 (91.3%) tumours found in adults (≥20 years), 4844 (7.3%) in children, and 897 (1.4%) in adolescents. The three most common tumour sites were oral, liver, and colorectal in males; breast, oral and ovary in females; bone, brain and connective tissue in adolescents; and leukaemia, brain and bone in children. The overall ASIR (%) in males was 89.20 for adults, 9.19 for children, and 1.61 for adolescents. The overall ASIR (%) in females was 93.44 for adults, 5.45 for children, and 1.11 for adolescents.
Conclusion: Oral cancer, a largely preventable cancer is the leading cancer in males while breast cancer is the leading cancer in females followed by oral cancer. In adolescents and children, the incidence closely matches most of the world.
Key Words: Karachi, Cancer registry, Oral cancer, Breast cancer, Age-standerdised ratio.
INTRODUCTION
Karachi is the most populous port city of Pakistan. All ethnic groups from across Pakistan are represented here making it an ideal location as a surrogate for national cancer patterns.
Karachi Cancer Registry (KCR) established at Karachi was revived on January 01, 2017, and initial results were reported in 2020.1 Since then, the registry is successfully functioning with consolidation and analyses of 5-year data to be presented here. Cancer registration in Karachi and Pakistan along with its challenges are already presented in an earlier communication.1 One silver line since the last report is the active data collection by Health Research Institute (HRI), NIH as the focal point for National Cancer Registration Program, which aims to establish a population-based National Cancer Registry (NCR) through the participation of countrywide network of hospitals and population-based cancer registries for data pooling.
Cancer incidence is increasing worldwide, and Pakistan is no exception. However, there are striking differences when local cancer incidence data of top-5 or top-10 cancers among adults are compared with the rest of the world outside the sub-continent. Major factors for this include lifestyle factors, highly prevalent viral infections like hepatitis B and C, consanguineous first cousin and early marriages along with relatively shorter median life-expectancy. In the absence of screening programs in a largely conservative society where women commonly shy away to seek medical care for two reasons, first being the fear of rejection by the spouse and family, and second being the non-availability of optimum diagnostic and treatment facilities or simply available but non-affordable for masses.
The objective of this study was to collect and analyse epidemiologic data of all malignancies by age group and gender for the Karachi population to estimate the cancer incidence of 5-years (2017-2021) and identify major risk factors for setting priorities towards cancer control programs.
METHODOLOGY
This observational study was conducted at Karachi Cancer Registry Secretariat, Pakistan Health Research Council (PHRC), JPMC, Karachi. Cancer data for the year 2017 to 2021 were received from seven tertiary care hospitals of Karachi on approved cancer notification form or on Excel sheet as a soft copy. The hospitals that shared their data in order of number of cases included the Aga Khan University Hospital, Jinnah Postgraduate Medical Center, Dow University of Medical Sciences, Indus Hospital, Ziauddin University Hospital, Zainab Punjwani Hospital, and Baqai Medical University Hospital. Variables included age, gender, date of first contact, primary tumour site and the ICD coding. All the data were cleaned, merged, and analysed.
All patients 0-14 years were classified as children while all aged 15-19 years were classified as adolescents and those 20-years and above as adults. Epidemiological data of all malignancies for 5-years (2017-2021) was analysed and classified using ICD-10.
Population census of 2017 reported the population of Karachi to be 16.1 million with 8.4 million males and 7.6 million females.2 Counts and age-standardised incidence rates (ASIR) were calculated for each of the three age groups. ASIR were computed using the World Standard of Segi3 as the standard population by applying the direct method of age-standardisation and presented as per 100,000 population by using Microsoft Excel and SPSS V.20.
RESULTS
During the last five years (2017-2021), a total of 65,886 malignant cases were received from seven participating hospitals. The distributions seen amongst males and females were 33,510 (51%) and 32,376 (49%), respectively with 91.3% tumours found in adults (≥20 years), whereas 4844 (7.3%) in children and 897 (1.4%) in adolescents. Tables I and II show the age-standardised incidence rate (ASIR) among females and males by age group (0–14, 15–19 and ≥20 years) of all cancer sites. ASIR by age group i.e., children, adolescents, and adults (0–14, 15–19 and ≥20 years) and gender are shown in Figure 1. ASIR of ten commonest tumours in children and adolescents are shown in Figure 2 while ASIR of the ten commonest tumours in adult females and males are shown in Figures 3 and 4. Figure 5 shows the ASIR of all cancers from 2017-2021 revealing a linear trend with slightly increase in females’ and decrease in males’ overtime.
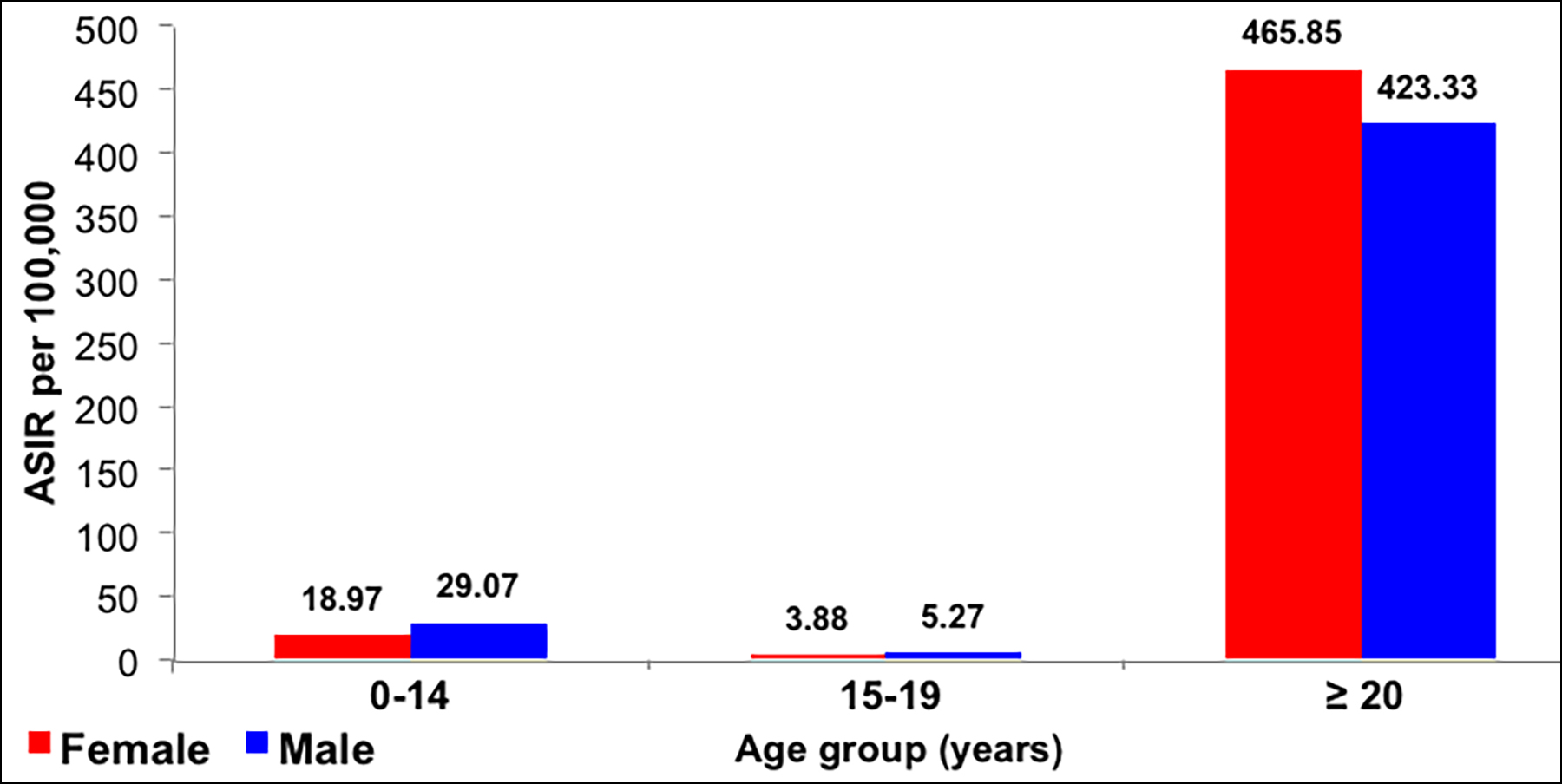 Figure 1: Age-standardised incidence rates (ASIR) by age group and gender, in the KCR, Pakistan 2017-2021.
Figure 1: Age-standardised incidence rates (ASIR) by age group and gender, in the KCR, Pakistan 2017-2021.
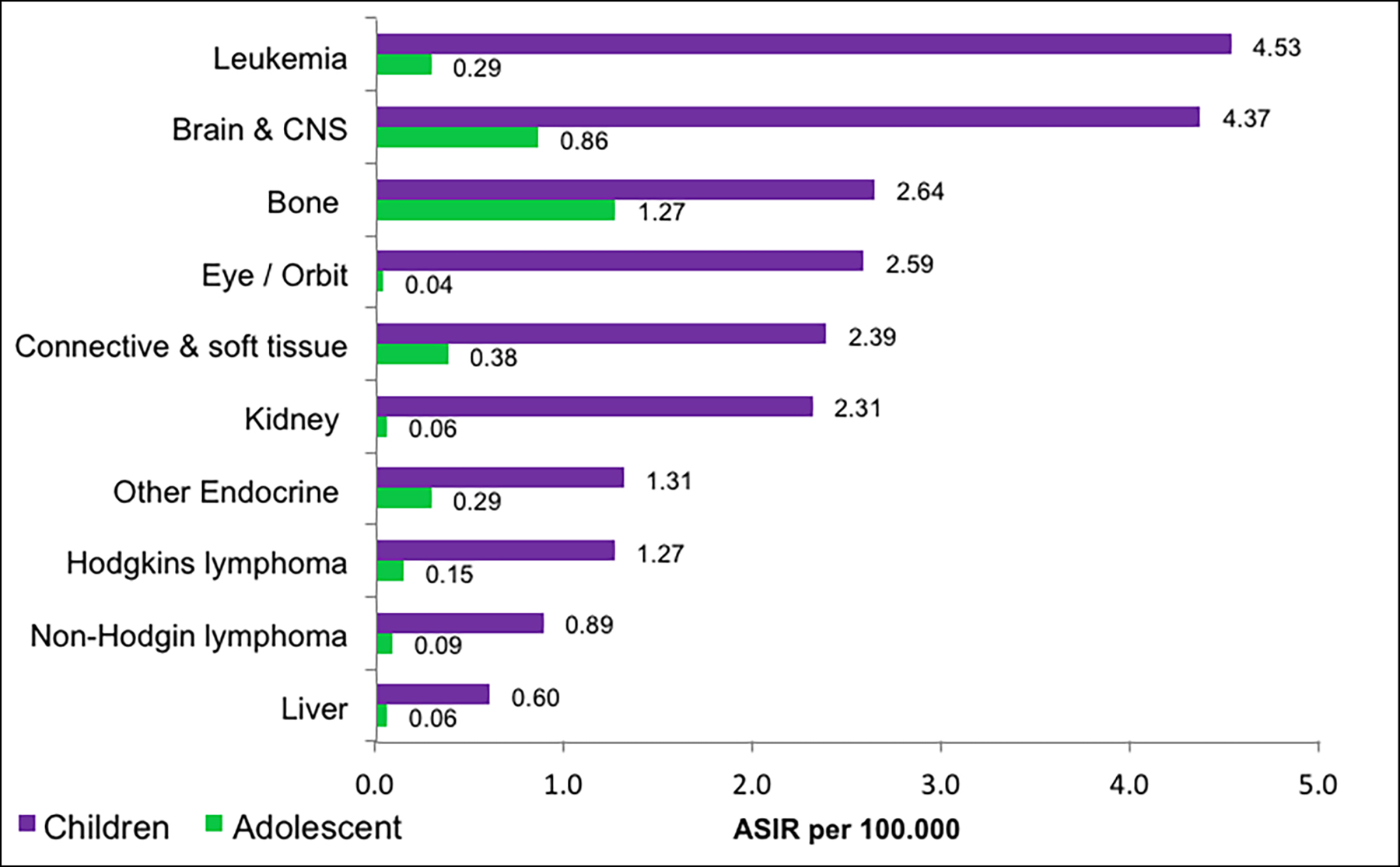 Figure 2: Age-standardised incidence rates (ASIR) of commonest tumour in children and adolescents, in the KCR, Pakistan 2017-2021.
Figure 2: Age-standardised incidence rates (ASIR) of commonest tumour in children and adolescents, in the KCR, Pakistan 2017-2021.
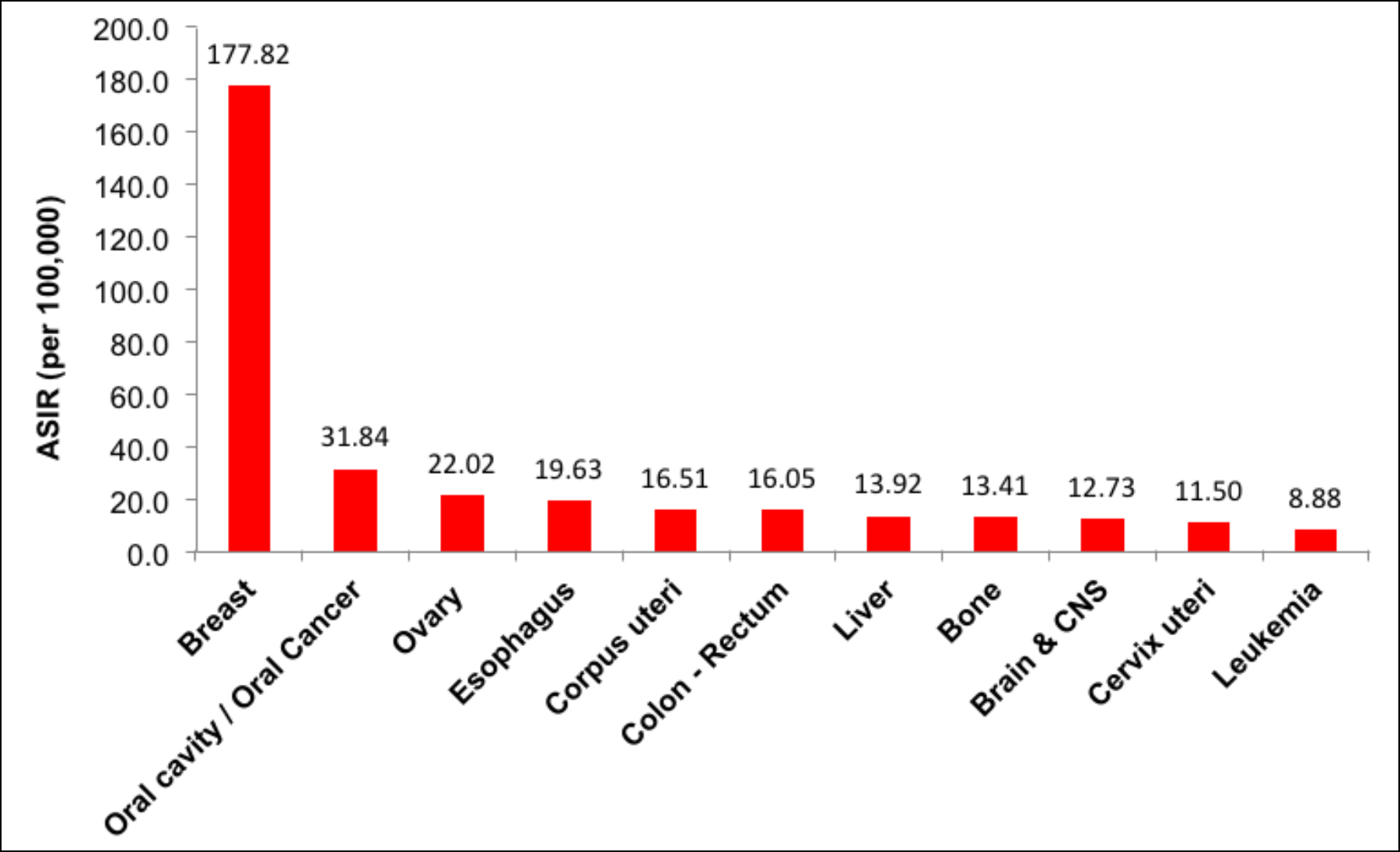 Figure 3: Age-standardised incidence rates (ASIR) of commonest tumour in adults females (≥20 years) in the KCR, Pakistan 2017-2021.
Figure 3: Age-standardised incidence rates (ASIR) of commonest tumour in adults females (≥20 years) in the KCR, Pakistan 2017-2021.
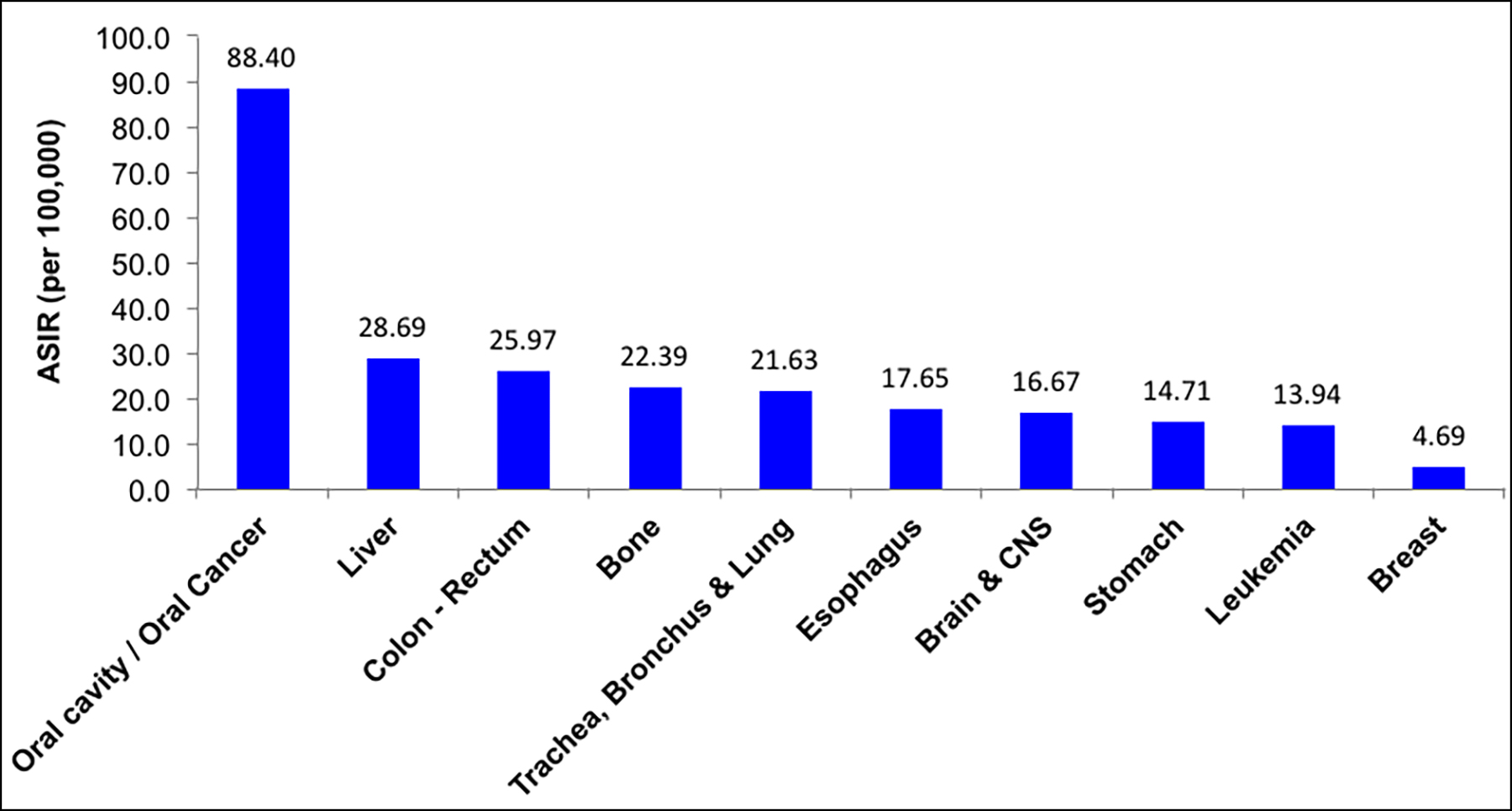 Figure 4: Age-standardised incidence rates (ASIR) commonest tumour in adults males (≥20 years) in the KCR, Pakistan 2017-2021.
Figure 4: Age-standardised incidence rates (ASIR) commonest tumour in adults males (≥20 years) in the KCR, Pakistan 2017-2021.
Table I: Age-standardised incidence rates (ASIR) among females, by age group, Pakistan 2017-2021.
|
Site (Females) |
0-14 years |
15-19 years |
≥20 years |
ICD -10 |
|||
|
Count |
ASIR |
Count |
ASIR |
Count |
ASIR |
||
|
Oral cavity / Oral cancer |
14 |
0.15 |
8 |
0.09 |
2068 |
31.84 |
C00-C06 |
|
Salivary gland |
7 |
0.08 |
0 |
0.00 |
147 |
2.26 |
C07-C08 |
|
Oropharynx |
1 |
0.01 |
0 |
0.00 |
88 |
1.36 |
C09-C10 |
|
Nasopharynx |
11 |
0.12 |
5 |
0.05 |
93 |
1.43 |
C11 |
|
Hypopharynx |
2 |
0.02 |
1 |
0.01 |
335 |
5.16 |
C12 - C14 |
|
Esophagus |
1 |
0.01 |
2 |
0.02 |
1275 |
19.63 |
C15 |
|
Stomach |
0 |
0.00 |
4 |
0.04 |
502 |
7.73 |
C16 |
|
Small intestine |
7 |
0.08 |
1 |
0.01 |
116 |
1.79 |
C17 |
|
Colon-rectum |
15 |
0.16 |
14 |
0.15 |
1042 |
16.05 |
C18-C21 |
|
Liver |
21 |
0.23 |
0 |
0.00 |
904 |
13.92 |
C22 |
|
Gall bladder and extrahepatic bile duct |
0 |
0.00 |
0 |
0.00 |
423 |
6.51 |
C23-C24 |
|
Pancreas |
3 |
0.03 |
2 |
0.02 |
272 |
4.19 |
C25 |
|
Spleen |
0 |
0.00 |
0 |
0.00 |
13 |
0.20 |
C26 |
|
Nose, sinuses, etc. |
13 |
0.14 |
2 |
0.02 |
67 |
1.03 |
C30-C31 |
|
Larynx |
1 |
0.01 |
0 |
0.00 |
175 |
2.69 |
C32 |
|
Trachea, bronchus and lung |
5 |
0.05 |
7 |
0.08 |
512 |
7.88 |
C33-C34 |
|
Thymus, heart, mediastinum and pleura |
15 |
0.16 |
8 |
0.09 |
104 |
1.60 |
C37-C38 |
|
Bone |
521 |
5.60 |
103 |
1.12 |
871 |
13.41 |
C40-C41 |
|
Skin |
13 |
0.14 |
5 |
0.05 |
479 |
7.38 |
C43-C44 |
|
Mesothelioma |
0 |
0.00 |
0 |
0.00 |
3 |
0.05 |
C45 |
|
Kaposi sarcoma |
0 |
0.00 |
0 |
0.00 |
2 |
0.03 |
C46 |
|
Connective and soft tissue |
104 |
1.12 |
14 |
0.15 |
320 |
4.93 |
C47,C49 |
|
Retroperitoneum |
15 |
0.16 |
1 |
0.01 |
126 |
1.94 |
C48 |
|
Breast |
6 |
0.06 |
18 |
0.20 |
11548 |
177.82 |
C50 |
|
Vulva and Vagina |
11 |
0.12 |
1 |
0.01 |
99 |
1.52 |
C51-C52 |
|
Cervix uteri |
1 |
0.01 |
0 |
0.00 |
747 |
11.50 |
C53 |
|
Corpus uteri |
0 |
0.00 |
0 |
0.00 |
1072 |
16.51 |
C54 |
|
Uterus |
1 |
0.01 |
1 |
0.01 |
249 |
3.83 |
C55 |
|
Ovary and uterine adnexa |
41 |
0.44 |
13 |
0.14 |
1430 |
22.02 |
C56-C57 |
|
Placenta |
0 |
0.00 |
1 |
0.01 |
20 |
0.31 |
C58 |
|
Kidney and other urinary organ |
111 |
1.19 |
3 |
0.03 |
237 |
3.65 |
C64-C66 |
|
Urinary bladder |
1 |
0.01 |
0 |
0.00 |
222 |
3.42 |
C67 |
|
Eye / Orbit |
121 |
1.30 |
1 |
0.01 |
63 |
0.97 |
C69 |
|
Brain and CNS |
171 |
1.84 |
44 |
0.48 |
827 |
12.73 |
C70-C72 |
|
Thyroid gland |
1 |
0.01 |
10 |
0.11 |
490 |
7.55 |
C73 |
|
Endocrine gland and related structure |
66 |
0.71 |
10 |
0.11 |
144 |
2.22 |
C74-C75 |
|
Hodgkin’s lymphoma |
28 |
0.30 |
8 |
0.09 |
120 |
1.85 |
C81 |
|
Non-Hodgkin lymphoma |
20 |
0.21 |
3 |
0.03 |
250 |
3.85 |
C82-85 |
|
Multiple myeloma |
0 |
0.00 |
0 |
0.00 |
33 |
0.51 |
C90 |
|
Leukaemia |
188 |
2.02 |
8 |
0.09 |
577 |
8.88 |
C91-95 |
|
Others and unspecified |
228 |
2.45 |
60 |
0.65 |
2188 |
33.69 |
|
|
All sites |
1765 |
18.97 |
358 |
3.88 |
30253 |
465.85 |
|
|
All sites n (%) |
1765 (5.45) |
358 (1.11) |
30253 (93.44) |
|
|||
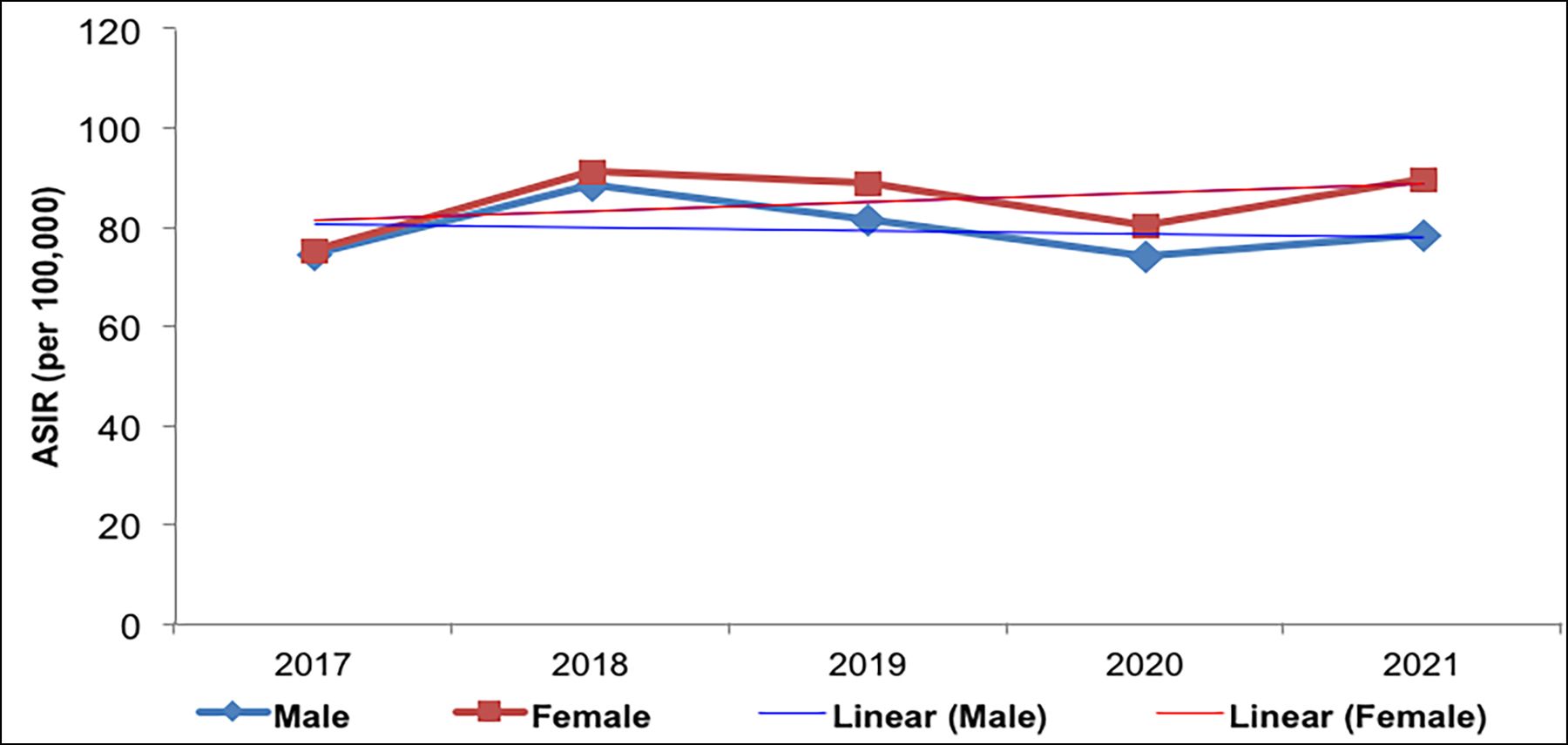 Figure 5: Age-standardised incidence rates (ASIR) of cancers among KCR by year, 2017–2021.
Figure 5: Age-standardised incidence rates (ASIR) of cancers among KCR by year, 2017–2021.
DISCUSSION
In 5-years from 2017 – 2021, 65,886 cancer cases were received from seven major participating Karachi hospitals. If this is compared to 2nd most populous city of Pakistan i.e., Lahore, a total of 58,394 cases were reported during 10-year period i.e., 2010-2019 with a population of 11.1 million as compared to Karachi population of 16.1 million.4 Pakistan is a young nation and as per 2017 census 40.3% of the population was between 0-14 years2 while only 3.7% were 65-years and above. Both in Karachi and Lahore highest incidence rates were recorded for breast cancer in adults, bone malignancies in adolescents and leukaemia in children.
KCR cancer statistics of children and adolescent groups show a higher proportion of male patients which is consistent with the findings of the 18-registries included in the Surveillance, Epidemiology, and End Results (SEER) program and the 162 out of 183 national registries evaluated by Globocan 2018. This disparity may be attributed to hormonal variations, particularly in the case of bone tumours, although a combination of genetic, immune-related, and social factors may also play a role.5,6
Table II: Age-standardised incidence rates (ASIR) among males, by age group, in the KCR, Pakistan 2017-2021.
|
Site (Males) |
0-14 years |
15-19 years |
≥20 years |
ICD -10 |
|||
|
Count |
ASIR |
Count |
ASIR |
Count |
ASIR |
||
|
Oral cavity / Oral cancer |
9 |
0.08 |
2 |
0.02 |
6224 |
88.14 |
C00-C06 |
|
Salivary gland |
12 |
0.11 |
3 |
0.03 |
207 |
2.93 |
C07-C08 |
|
Oropharynx |
3 |
0.03 |
0 |
0.00 |
192 |
2.72 |
C09-C10 |
|
Nasopharynx |
18 |
0.17 |
8 |
0.08 |
245 |
3.47 |
C11 |
|
Hypopharynx |
2 |
0.02 |
1 |
0.01 |
720 |
10.20 |
C12-C14 |
|
Esophagus |
1 |
0.01 |
2 |
0.02 |
1246 |
17.65 |
C15 |
|
Stomach |
2 |
0.02 |
3 |
0.03 |
1039 |
14.71 |
C16 |
|
Small intestine |
12 |
0.11 |
2 |
0.02 |
126 |
1.78 |
C17 |
|
Colon-rectum |
32 |
0.30 |
21 |
0.21 |
1834 |
25.97 |
C18-C21 |
|
Liver |
43 |
0.41 |
6 |
0.06 |
2026 |
28.69 |
C22 |
|
Gall bladder and extrahepatic bile duct |
0 |
0.00 |
0 |
0.00 |
349 |
4.94 |
C23-C24 |
|
Pancreas |
4 |
0.04 |
2 |
0.02 |
418 |
5.92 |
C25 |
|
Spleen |
2 |
0.02 |
0 |
0.00 |
7 |
0.10 |
C26 |
|
Nose, sinuses, etc. |
20 |
0.19 |
4 |
0.04 |
119 |
1.69 |
C30-C31 |
|
Larynx |
3 |
0.03 |
0 |
0.00 |
752 |
10.65 |
C32 |
|
Trachea, bronchus and lung |
9 |
0.08 |
1 |
0.01 |
1527 |
21.63 |
C33-C34 |
|
Thymus, heart, mediastinum and pleura |
44 |
0.42 |
7 |
0.07 |
149 |
2.11 |
C37-C38 |
|
Bone |
907 |
8.56 |
202 |
1.98 |
1581 |
22.39 |
C40-C42 |
|
Skin |
20 |
0.19 |
11 |
0.11 |
738 |
10.45 |
C43-C44 |
|
Mesothelioma |
0 |
0.00 |
0 |
0.00 |
17 |
0.24 |
C45 |
|
Connective and soft tissue |
149 |
1.41 |
25 |
0.24 |
534 |
7.56 |
C47,C49 |
|
Retroperitoneum |
15 |
0.14 |
1 |
0.01 |
73 |
1.03 |
C48 |
|
Breast |
0 |
0.00 |
0 |
0.00 |
331 |
4.69 |
C50 |
|
Penis |
0 |
0.00 |
0 |
0.00 |
10 |
0.14 |
C60 |
|
Prostate |
4 |
0.04 |
0 |
0.00 |
1276 |
18.07 |
C61 |
|
Testis |
56 |
0.53 |
18 |
0.18 |
278 |
3.94 |
C62 |
|
Other and unspecified male genital organs |
0 |
0.00 |
0 |
0.00 |
6 |
0.08 |
C63 |
|
Kidney and other urinary organ |
134 |
1.27 |
3 |
0.03 |
551 |
7.80 |
C64-C66 |
|
Urinary bladder |
12 |
0.11 |
0 |
0.00 |
813 |
11.51 |
C67 |
|
Other and unspecified urinary organs |
3 |
0.03 |
0 |
0.00 |
5 |
0.07 |
C68 |
|
Eye / Orbit |
153 |
1.44 |
3 |
0.03 |
118 |
1.67 |
C69 |
|
Brain and CNS |
292 |
2.76 |
44 |
0.43 |
1177 |
16.67 |
C70-C72 |
|
Thyroid gland |
2 |
0.02 |
7 |
0.07 |
239 |
3.38 |
C73 |
|
Endocrine gland and related structure |
73 |
0.69 |
20 |
0.20 |
241 |
3.41 |
C74-C75 |
|
Hodgkin’s lymphoma |
106 |
1.00 |
7 |
0.07 |
264 |
3.74 |
C81 |
|
Non-Hodgkin lymphoma |
74 |
0.70 |
6 |
0.06 |
539 |
7.63 |
C82-85 |
|
Multiple myeloma |
0 |
0.00 |
0 |
0.00 |
76 |
1.08 |
C89, C90 |
|
Leukaemia |
292 |
2.76 |
22 |
0.22 |
984 |
13.94 |
C91-C95 |
|
Others and unspecified |
571 |
5.39 |
108 |
1.06 |
2861 |
40.52 |
|
|
All Sites |
3079 |
29.07 |
539 |
5.27 |
29892 |
423.33 |
|
|
All sites n (%) |
3079 (9.19) |
539 (1.61) |
29892 (89.20) |
|
|||
During the study period, the most frequently diagnosed pediatric cancers were leukaemias (ASIR in children: 4.53 and 0.29 in adolescents), followed by Brain/CNS (ASIR in children: 4.37 and 0.86 in adolescents) and bone tumours (ASIR in children: 2.64 and 1.27 in adolescents). These proportions are in line with the estimates provided by Globocan, which indicate that leukaemia and brain/CNS tumours accounted for 45% of cases and 57% of deaths among children with cancer in 2018.5 The pattern of site-specific case distribution in Karachi is like another study results of pediatric cancer cases from three centres of Pakistan between 2016 and 2018 i.e., male predominance and leukaemias, lymphomas, and retinoblastomas being the top three cancers.7 Punjab Cancer Registry (PCR), which collects data on cancer incidence from collaborating centres in the Punjab province of Pakistan covering Lahore and adjoining regions, also reported acute lymphoblastic leukaemia, glioma, and Hodgkin's lymphoma as the most frequently occurring childhood cancers in 2020.8
Additionally, it is important to note that low-income and middle-income countries have a younger demographic and therefore a larger proportion of children with cancer compared to high-income countries.9 Unfortunately, many of these children do not survive the disease. Chronic infections, which are the leading cause of disease-related deaths in all countries except for high-income ones, can also significantly increase the risk of childhood cancer in regions with lower socio-economic status.10
Adult malignancies constituted the bulk of cases i.e., 91.3% of all cases. Oral cancer (OC) stands out as the most common cancer in males and second most common cancer in females of Karachi. As discussed earlier, an overwhelming majority were chronic chewers using betel-nut and tobacco in various forms and combinations readily and relatively economically available.1,11 With each passing day, more and more are attracted for its use for two reasons of being relatively less costly and more socially acceptable than smoking, which is largely prohibited at most public places. Production of various ingredients and packing in readymade sachets is a multimillion-rupee industry and business albeit illegal across length and breadth of Karachi employing hundreds of thousands of workers at various levels of this supply chain.1,12 In contrast to OC, oropharyngeal cancer (OPC) involving base of tongue, tonsils, and soft palate is uncommon while laryngeal cancer which has strong association with smoking is dwarfed on the face of OC.
Breast cancer in females is touching alarming proportions with added disadvantage of being diagnosed in younger females in their fourth, third, and even second decade of life. This is further compounded by lack of awareness, social taboo in a conservative society resulting in late diagnosis, higher stage with associated high morbidity and mortality. This in the absence of any screening program is a major cause of concern. Some well-established risk factors in developed countries like nulliparity are nullified here as most women are multiparous.13,14 A significant role of genetics is likely as cousin marriages are very common in Pakistan. As this is a hormone-dependent cancer the role of dairy products remains a dilemma, as in Pakistan it is buffalo milk which is predominantly consumed by masses and indiscriminate use of hormones to increase milk production and profits is believed to be rampant.
Other preventable cancers frequently diagnosed and are included in top-5 or top-10 cancers include liver cancer, colonic cancer, and lung cancer. Pakistan now has the highest number of people living with hepatitis C while hepatitis B is also common.15-17 Most liver cancers in Pakistan arise as a complication of cirrhosis in people who are infected with chronic hepatitis B and C. Large bowel cancer is on the rise at an alarming rate and increasing consumption of junk food along with genetic predisposition seems to be the triggering factor.18,19 Incidentally in younger patients most adenocarcinomas of the large bowel show signet ring morphology indistinguishable from more common gastric signet-ring type adenocarcinoma. Lung cancer though no more leading cancer in males of Karachi, however, still poses a significant burden of cancer among Karachiites. Cigarette smoking is strongly associated with lung cancer, but recent trend shows switching from cigarettes to gutka (taken orally and kept in the mouth for hours to allow slow absorption). This shift might be due to higher cost of the cigarettes or high unrefined content of tobacco in the gutka. Air pollution could also be contributing to the cause because it sometimes touches dangerous proportions as Karachi is among the few most polluted cities of the world along with some others in the sub-continent like Lahore, Delhi, Mumbai, Dhaka, and Kolkata.20 Esophageal cancer is another cancer which is highly prevalent in both genders and is largely attributed to lifestyle.21
In females, after breast cancer, ovarian uterine, and cervical cancers are more prevalent. The role of Human Papillomavirus in cervical cancer is well known but the data from Pakistan is limited in the absence of cervical screening.
Reliable data acquisition is an uphill task in most developing countries as reporting of new cancer cases is not mandatory by law, hence all cancer data are obtained on voluntary basis resulting in missing of cases on one hand and duplication on the other. Although all Pakistani citizens are required to have a unique Central National Identity Number (CNIC), however, record keeping using this unique identity is not uniformly practised by all cancer diagnosing and treating hospitals. A significant effort was made to minimise duplication by matching available data, however, its entire elimination may only be guaranteed if all data is received with CNIC. This is the next most important goal of KCR.
Over 95% cases of cancer recorded in the registry were microscopically verified. Exceptions include a subset of liver cancers where other parameters including hepatitis profile, radiology, and serum AFP levels were good enough to make a confident diagnosis. The occurrence, morbidity and mortality associated with these cancers may be minimised to a great extent by early detection and screening on one hand and by curbing sale and availability of highly carcinogenic stuff on the other.
CONCLUSION
Based on the 5-year cancer incidence data of KCR, breast cancer incidence is touching alarming proportions not only in frequency but presentation at early age (pre-menopausal) with higher grade and stage in females. Oral Cancer, the most common cancer in males and second most common in females is also showing significant increase despite being easily preventable. This is followed by liver Cancer, lung cancer, colorectal cancer and esophageal cancer.
ACKNOWLEDGEMENT:
KCR duly acknowledges all participating hospitals of Karachi for their voluntary contribution of cancer data to KCR. KCR also sincerely thank Meximp Technologies, Karachi, Pakistan for their support.
ETHICAL APPROVAL AND PATIENTS' CONSENT:
Ethical approval and individual patient consent for cancer registries was taken by the respective hospitals sharing data and was almost always exempted by the respective Ethical Committees as identity of the individual patients was never revealed at any stage and it became part of a large cohort where only ASIR of various cancers were calculated within Karachi.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SP: Manuscript write-up.
AAJ, GH, MAQ, SA, FL, MK, IB, MZ, NM: Contribution of data.
ZF, NY: Contribution in write-up, editing of the manuscript, and contribution of adult cancer data.
MSQ, EA, HQ: Significant contribution in the manuscript write-up.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Pervez S, Jabbar AA, Haider G, Ashraf S, Qureshi MA, Lateef F, et al. Karachi cancer registry: Age-standardised incidence rate by age-group and gender in a mega city of Pakistan. Asian Pac J Cancer Prev 2020; 21(11):3251-8. doi: 10.31557/APJCP.2020.21.11.3251.
- Census of Pakistan, 2017: http://www.pbs.gov.pk/content/ population-census Pakistan Bureau of Statistics.
- Bray F and Ferlay F 2023. Age Standardization - Inter-national Agency: https://ci5.iarc.fr/CI5-XI/ Pages/Chapter7. aspx
- Badar F, Mahmood S, Mahmood MT, Masood M, Tanvir I, Chughtai OR, et al. Cancer Epidemiology in Lahore, Pakistan - 2010-2015. J Coll Physicians Surg Pak 2020; 30(2):113-22. doi: 10.29271/jcpsp.2020.02.113.
- Sharma R. A Systematic examination of burden of childhood cancers in 183 countries: Estimates from GLOBOCAN 2018. Eur J Cancer Care (Engl) 2021; 30(5): e13438. doi: 10.1111/ecc.13438.
- Williams LA, Richardson M, Marcotte EL, Poynter JN, Spector LG. Sex ratio among childhood cancers by single year of age. Pediatr Blood Cancer 2019; 66(6):e27620. doi: 10.1002/pbc.27620.
- Hamid M, Raza M, Ashraf S, Maqsood S. Establishing childhood cancer registry status in 3 pediatric oncology units of Pakistan - A low middle-income country. Sci World J Cancer Sci Ther 2021; 1(2);1-4.
- Punjab Cancer Registry: Available from: http://punjab cancerregistry.org.pk/downloads.php.
- Gupta S, Rivera-Luna R, Ribeiro RC, Howard SC. Pediatric oncology as the next global child health priority: The need for national childhood cancer strategies in low- and middle-income countries. PLOS Med 2014; 11(6): e1001656. doi: 10.1371/journal.pmed.1001656.
- Magrath I, Steliarova-Foucher E, Epelman S, Ribeiro RC, Harif M, Li CK, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol 2013; 14(3): e104-16. doi: 10.1016/S1470-2045(13)70008-1.
- Pervez S, Abro A. Oral cancer and chewing habits. In ‘development of oral cancer’ Al Moustafa ed’. Springer 2017; 115-32. Doi.10.1007/978-3-319-48054-1_8.
- Anwar N, Pervez S, Chundriger Q, Awan S, Moatter T, Ali TS. Oral cancer: Clinicopathological features and associated risk factors in a high-risk population presenting to a major tertiary care center in Pakistan. PLoS One 2020; 15(8):e0236359. doi: 10.1371/journal.pone.023 6359.
- Begum N. Breast cancer in Pakistan: A Looming epidemic. J Coll Physicians Surg Pak 2018; 28(2):87-8. doi: 10. 29271/jcpsp.2018.02.87.
- Saeed S, Asim M, Sohail MM. Fears and barriers: Problems in breast cancer diagnosis and treatment in Pakistan. BMC Women's Health 2021; 21(1):151 doi.org/10.1186/ s12905-021-01293-6.
- Hafeez Bhatti AB, Dar FS, Waheed A, Shafique K, Sultan F, Shah NH. Hepatocellular carcinoma in Pakistan: National trends and global perspective. Gastroenterol Res Pract 2016; 2016:5942306. doi: 10.1155/2016/5942306.
- Pakistan health research center and world health organisation. National hepatitis strategic framework (NHSF) for Pakistan 2017-21. www.globalhep.org/sites/ default/files/content/action_plan_article/files/2020/04/Pakistan--national-hepatitisstrategic-framework--09-01- 2018.pdf.
- Global, regional, and national burden of hepatitis B, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol Hepatol 2022; 7(9):796-829. https://doi.org/10.1016/S2468-1253(22)001 24-8.
- Abid M, Parvez A. Colorectal cancer in Pakistan: Is prevention possible? J Pak Med Assoc 2022; 72(9):1899. doi: 10.47391/JPMA.5402.
- Muhammad SZ, Fatima N. Realizing the need for colorectal cancer screening in Pakistan. J Pak Med Assoc 2020; 70(7):1309. doi: 10.5455/JPMA.65781.
- Majeed FA, Azeem AR, Farhan N. Lung cancer in Pakistan, where do we stand? J Pak Med Assoc 2019; 69(3):405-8.
- Bhurgri Y, Faridi N, Kazi LA, Ali SK, Bhurgri H, Usman A, et al. Cancer esophagus Karachi 1995-2002: Epidemiology, risk factors and trends. J Pak Med Assoc 2004; 54(7): 345-8. PMID: 15449914.