Frequency of Premenstrual Dysphoric Disorder (PMDD) and Comparison of Quality of Life between Female Medical Students with and without Premenstrual Dysphoric Disorder
By Zainab Mahmood1, Ammara Butt2, Mohsin Ali Cheema3Affiliations
doi: 10.29271/jcpsp.2023.06.638ABSTRACT
Objective: To determine the frequency of Premenstrual Dysphoric Disorder (PMDD) in female medical students, and to compare the quality of life between those with and without PMDD.
Study Design: Descriptive Study.
Place and Duration of the Study: Fatima Jinnah Medical University, Lahore, from November 2019 to April 2020.
Methodology: The study included 635 female medical students from the third year to the final year of MBBS. Quality of life was measured by using the World Health Organization Quality of Life Brief (WHOQOL-BREF) Scale and PMDD was diagnosed as per DSM-V Diagnostic criteria. Data were entered and analysed by IBM SPSS version 23.0. Scores of 4 domains of the WHOQOL‐BREF scale were compared between the female medical students with and without PMDD. A p‐value of ≤0.05 was considered statistically significant.
Results: Significant proportion i.e., 12.1% (77) out of 635 female medical students had PMDD. There was a significant difference in the physical and psychological domains scores of the WHOQOL‐BREF scale between healthy students and students with PMDD (p-value <0.001).
Conclusion: The physical and Psychological aspects of quality of life are significantly lower in female medical students with PMDD.
Key Words: WHOQOL‐BREF, Premenstrual dysphoric disorder, Female medical students.
INTRODUCTION
Premenstrual dysphoric disorder (PMDD) having a global prevalence of 1.2%, is characterised by a cyclical set of behavioural, mood, and physical symptoms. They start in the week preceding the menstrual cycle followed by their resolution within one week post menses.1 Several studies have been conducted in Pakistan exploring the impact of premenstrual syndrome (PMS) on quality of life.2,3 However, there is a scarcity of data about the effects of PMDD on quality of life. It is observed that using more stringent criteria such as the Diagnostic and Statistical Manual 5th version( DSM V) or the American College of Obstetricians and Gynaecologists (ACOG) reduces the likelihood of overestimation.4
For the evaluation of the quality of life, the World Health Organisation Quality of Life Brief (WHOQOL-BREF) scale is a reliable tool that has been used in various global studies.5
The present study may prove to be useful in extending a more comprehensive psychotherapeutic help to female medical students suffering from debilitating symptoms of PMDD while studying in a high-stress environment. There is scarcity of literature on local women as it is considered a taboo to discuss women’s health. The aim of this study was to identify the female medical students suffering from PMDD as per the DSM V(1) criteria and to compare the quality of life between female medical students with and without premenstrual dysphoric disorder using the WHOQOL-BREF scale.6
METHODOLOGY
This descriptive study was conducted from November 2019 to April 2020 at Fatima Jinnah Medical University, Lahore. After obtaining approval from the Institutional Review Board and Ethical Review Committee, a predesigned proforma including PMDD diagnostic checklist as per DSM-V (1) and WHOQOL-BREF scale was given to the 637 female medical students from 3rd-year MBBS to Final year MBBS. The sample size was calculated with the help of a computer program Power Analysis and sample size 2008 Home Version (PASS 2008). Accordingly, a minimum of 140 girls was to be included in the study. It was also estimated that group sample sizes of 70 in the PMDD group and 70 in the healthy group would achieve 90% power to detect a difference of 0.56 between the null hypothesis mean difference of 0.0 and the actual mean difference of -0.56 at the 0.050 significance level (alpha).
The principal investigator explained in detail the methodology of filling out the questionnaires during every session. After getting written informed consent, un‐married female medical students who had regular menstrual cycles (21 to 35 days duration and menstrual flow lasting from 2 to 7 days) for the last 6 months were recruited by convenience sampling. Students with any known psychiatric disorder (depressive disorder, panic disorder, personality disorder) or medical disorders such as thyroid disease, diabetes, PCOS, etc were excluded. All the received proformas were organised and assessed for completion. Two proformas were incomplete and not included. Filled proformas were allocated into two groups i.e., the PMDD group (77 students) as per DSM-V criteria and the H (healthy) group (558 students).
The collected data were entered and analysed in IBM SPSS version 23.0. WHOQOL-BREF scale was analysed according to the procedure mentioned in the manual of WHOQOL-BREF - Introduction, administration, scoring, and generic version of the assessment - field trial version - December 1996(6). Cronbach alpha values for each of the 4 domains of the WHOQOL‐BREF scale were calculated for internal consistency. Frequencies and percentages are given for categorical variables such as various demographic characteristics of study subjects, responses of questions of WHOQOL-BREF scale, and responses of PMDD diagnostic checklist as per DSM-V. The normality of quantitative data i.e., Age and the Scores of the 4 domains of the WHOQOL‐BREF scale was checked by Shapiro Wilk's test. Age and scores of 4 domains of the WHOQOL‐BREF scale are expressed as median (IQR) as these were found to be non-normally distributed in both healthy and PMDD Groups. All the quantitative variables i.e., Age and Scores of 4 domains of the WHOQOL‐BREF scale were found to be non-normally distributed in both healthy and PMDD Groups as well as groups based on MBBS study year. Mann Whitney U test was used to compare the quantitative variables between the Healthy and PMDD groups. Kruskal Wallis Test was used to compare the Age and various domain scores of WHO QOL BREF scale between MBBS study years. Chi-square test was used to determine the association between PMDD and MBBS Study years. A p‐value of ≤0.05 was considered statistically significant for all purposes.
RESULTS
After a detailed analysis of 635 completely filled proformas, 558 (87.9%) girls were included in the H group and 77 (12.1%) girls were included in the PMDD group. The median (IQR) age of all study participants was 22.40 (21.50-23.27) years. A significant association (p-value=0.032, Table II) between the MBBS study year and the presence of PMDD was seen with the highest proportion (16.7%) of 5th-year girls having PMDD (Figure 1). Physical, psychological, and environmental domains of THE WHOQOL BREF scale showed good internal consistency having Cronbach alpha >0.70. The domain 1 (physical health) and domain 2(psychological) scores of the WHOQOL BREF scale for students with PMDD were significantly lesser (p-value <0.001) than healthy students (Table I). A significant proportion (40.3%, n=31) of the students in the PMDD group were dissatisfied with their work capacity compared to healthy students. Additionally, 44.2% (n=34) of students with PMDD reported hindrance from physical pain in their daily routine.
Table I: Comparison of transformed scores of various domains, and scores of two global questions of the WHOQOL-BREF scale between Healthy and PMDD Groups by Mann–Whitney U test.
|
Parameter |
PMDD Group Median (IQR) |
Healthy Group Median (IQR) |
p-value |
|
Domain 1 score (Physical health) |
56.00 (44.00-66.00) |
63.00 (54.50-75.00) |
<0.001* |
|
Domain 2 score (Psychological) |
56.00 (40.00-63.00) |
63.00 (50.00-69.00) |
<0.001* |
|
Domain 3 score (Social relationships) |
50.00 (31.00-69.00) |
56.00 (44.00-69.00) |
0.073 |
|
Domain 4 score (Environment) |
69.00 (56.00-75.00) |
69.00 (56.00-75.00) |
0.636 |
|
Score of question G1 (How would you rate |
4.00 (4.00-4.00) |
4.00 (4.00-4.00) |
0.175 |
|
Score of question G4 (How satisfied are you |
4.00 (4.00-4.00) |
4.00 (4.00-4.00) |
0.436 |
|
*p-value ≤0.05 is considered statistically significant.
|
|||
DISCUSSION
In this study, 12.1% of female medical students fulfilled the DSM-V diagnostic criteria for PMDD. Several studies determining the frequency or prevalence of PMDD in different study populations show extreme variations with a decreasing trend of prevalence of PMDD in a given population when more rigorous criteria such as DSM-V is applied.3,7
Regarding the domain 1 (physical health), a significant difference (p<0.001, Table I) in scores was found between healthy students (63.00, 54.0-25.1) and students with PMDD (median = 56.00). Delara et al. conducted a study on school-going girls,8 to assess the quality of life using the health-related quality of life Short Form Health Survey (SF 36).
Table II: Association of PMDD with MBBS study year and comparison of age and various domain scores of WHOQOL-BREF scale between students in 3rd, 4th and 5th years of MBBS.
|
MBBS Study Year |
n |
Students with PMDD n (%) |
Age Median (IQR) |
WHOQOL-BREF scores |
|||
|
Domain 1 (Physical) |
Domain 2 (Psychological) |
Domain 3 (Social) |
Domain 4 (Environmental) |
||||
|
3rd Year MBBS |
203 |
17 (8.4%) |
21.30 (20.65-21.95) |
63.00 (56.00-75.00) |
63.00 (50.00-69.00) |
69.00 (50.00-75.00) |
69.00 (56.00-75.00) |
|
4th Year MBBS |
229 |
26 (11.4%) |
22.40 (21.60-23.00) |
63.00 (44.00-69.00) |
56.00 (44.00-69.00) |
56.00 (31.00-69.00) |
69.00 (56.00-75.00) |
|
5th Year MBBS |
203 |
34 (16.7%) |
23.40 (22.80-23.90) |
63.00 (50.00-69.00) |
56.00 (50.00-69.00) |
50.00 (44.00-69.00) |
69.00 (56.00-75.00) |
|
P-value |
0.032*b |
<0.001*a |
0.007*a |
0.003*a |
<0.001*a |
0.603a |
|
|
*p-value ≤0.05 is considered statistically significant, ap-value is calculated by Kruskal Wallis test, bP-value is calculated by Chi-square test. |
|||||||
Health-related quality of life was found to be significantly disturbed (p <0.001) in the domains of physical pain in girls having PMS/PMDD. These results are consistent with the results of this study in which a different tool i.e., WHOQOL-BREF scale was used to assess the quality of life.
In this study, almost half (47.5%) of the healthy female medical students had no complaint of physical pain leading to difficulty performing daily tasks. On the contrary, 44.2% of the female medical students with PMDD reported hindrance from physical pain in their daily routine. This association of PMDD with difficulty performing daily tasks due to physical pain was found to be statistically significant (p = 0.001). It was also found that 80.4% of the students in the healthy group required very little medical treatment for daily functioning, however, 50.7% of the students with PMMD required a moderate amount of medication to carry out daily tasks (p-value = 0.001). This shows that trend of using medication to cope with physical pain is prevalent in medical students suffering from PMDD. Similar findings were observed in a cross-sectional survey from multiple European countries using the Activities of Daily Life (ADL) scoring checklist.9
In the present study, work capacity was found to be significantly associated with the presence of PMDD (p=0.02). The majority (40.3%) of the students having PMDD were dissatisfied with their work capacity compared to healthy students, half of whom reported adequate satisfaction with their work capacity. These findings were also mirrored in a study conducted at another Medical College,10 where a very high percentage (76%) of students reported that premenstrual symptoms interfered significantly with their academic activities. Similar results were reported by Mohib et al.4 Similar findings were also observed in Jordanian students who reported decrease in academic performance due to PMDD.11 Hence physical symptoms of PMDD along with a reduction in work capacity are a point of concern for medical students suffering from PMDD due to the gruelling academic requirements in medical college, also demonstrated by studies conducted in India in 2021 and Ethiopia in 2017.12,13
In the present study, students with PMDD have significantly lower (p<0.001) psychological domain scores when compared with healthy students. The majority (41.2%) of healthy students find life to be meaningful whereas 14.3% of the students with PMDD report life to be of little meaning. This association of perception of meaningful life with PMDD is statistically significant (p=0.018). Similarly, around 60% of healthy students were very satisfied with themselves whereas more than a quarter (27.3%) of students with PMDD reported dissatisfaction with themselves (p=0.004). A significant association (p-value=0.001) between the occurrence of negative feelings with the presence of PMDD is also seen in this study. Only a quarter of the healthy students (26.8%) report having negative thoughts while almost half (46.1%) of the students in the PMDD group regularly have pessimistic ideas.
Similar results were reported by Shamnani et al. who found that the most frequent mood symptom in medical students with PMS was irritability (50%).14 A similar study conducted in Brazil by Victor et al. also showed a significant difference in psychological domain scores between females with and without PMDD.15 Considering the results of this study as well as the studies cited, it can be observed that mood symptoms are of considerable importance as they significantly affect the quality of life. Recent evidence suggests that premenstrual dysphoric disorder in itself is a risk factor for the development of postpartum depression.16,17 Therefore, the female students screened for PMDD should be vigilantly tracked and guided regarding the emergence of other psychiatric morbidities, such as Major Depressive Disorder.
This study was conducted in a single Medical College with a relatively smaller sample size. Future studies may be planned involving various educational institutes, regarding the impact of PMDD on the functional efficiency of female students while studying in a high-stress environment.
CONCLUSION
The proportion of female medical students suffering from PMDD is substantially high i.e., 12.1%. PMDD has not only affected the physical health of these students but has also led to a significant decline in their work capacity as well as deterioration in their psychological health. To facilitate and improve the mental health of female medical students, who are already enrolled in a grueling study program, special attention should be given to the debilitating effects of PMDD.
ETHICAL APPROVAL:
Approval from the Ethics Review Committee of Fatima Jinnah Medical University/Sir Ganga Ram Hospital Lahore was obtained prior to initiation of the research work.
PATIENTS’ CONSENT:
Informed written consent was taken from all the participants for inclusion in the study and publication of results maintaining confidentiality.
COMPETING INTEREST:
All the authors declare no competing interest.
AUTHORS’ CONTRIBUTION:
ZM: concept and study design, data collection, drafting of discussion, and literature review.
AB: concept and study design, data collection, and critical review of intellectual content.
MAC: concept and study design, conducted statistical analysis, and drafting of results.
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-5-TR. American Psychiatric Association Publishing; 2022 doi:10.1176/appi. books. 9780890425787.
- Mushtaq A, Arif S, Sabih F. Premenstrual symptoms as predictor of quality of life in reproductive-aged women of Rawalakot, Azad Kashmir: A cross sectional study. J Pak Med Assoc 2020; 70(12):2394-7. doi. 417. 10.47391/JPMA. 417.
- Majeed S, Moin H, Shafi R, Irshad K, Ashraf I, Janjua K. Prevalence, knowledge, attitude and practices towards premenstrual syndrome among university students in Islamabad and its impact on their daily life. Rawal Med J 2019; 44(3): 588.
- Mohib A, Zafar A, Najam A, Tanveer H, Rehman R. Premenstrual syndrome: Existence, knowledge, and attitude among female university students in Karachi. Cureus 2018; 10(3). doi:10.7759/cureus.2290.
- Aboshaiqah AE, Cruz JP. Quality of life and its predictors among nursing students in Saudi Arabia. J Holist Nurs Off J Am Holist Nurses Assoc 2019; 37(2):200-8. doi.10.1177/ 0898010118784147.
- The WHOQOL group. Development of the world health organization WHOQOL-BREF quality of life assessment. Psychol Med 1998; 28(3):551-8. doi.10.1017/s003329179 8006667.
- Takeda T. Premenstrual disorders: Premenstrual syndrome and premenstrual dysphoric disorder. J Obstet Gynaecol Res 2023; 49(2):510-8. doi.10.1111/jog.15484.
- Delara M, Ghofranipour F, Azadfallah P, Tavafian SS, Kazemnejad A, Montazeri A. Health related quality of life among adolescents with premenstrual disorders: A cross sectional study. Health Qual Life Outcomes 2012; 10:1. doi:10.1186/ 1477-7525-10-1.
- Dennerstein L, Lehert P, Backström TC, Heinemann K. The effect of premenstrual symptoms on activities of daily life. Fertil Steril 2010; 94(3):1059-64. doi:10.1016/j.fertnstert 2009.04.023.
- Hashim R, Ayyub A, Hameed S, Qamar K, Ali S, Raza G. Premenstrual syndrome: Messes with my academic performance. Pak Armed Forces Med J 2014; 64(2):199- 203.
- Hussein Shehadeh J, Hamdan-Mansour AM. Prevalence and association of premenstrual syndrome and premenstrual dysphoric disorder with academic performance among female university students. Perspect Psychiatr Care 2018; 54(2):176-84. doi:10.1111/ppc.12219.
- Thakrar P, Bhukar K, Oswal R. Premenstrual dysphoric disorder: Prevalence, quality of life and disability due to illness among medical and paramedical students. J Affect Disord Rep 2021; 4:100112. doi:10.1016/j.jadr.2021.100 112.
- Tsegaye D, Getachew Y. Premenstrual dysphoric disorder and associated factors among female health science students in Wollo University, Ethiopia, 2017/18. Matern Health Neonatol Perinatol 2019; 5:8. doi:10.1186/ s40748-019-0102-z.
- Shamnani G, Gupta V, Jiwane R, Singh S, Tiwari S, Bhartiy SS. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among medical students and its impact on their academic and social performance. Natl J Physiol Pharm Pharmacol 2018; 8(8):1205-8. doi:10.5455/njppp.2018.8.0415728042018
- Victor FF, Souza AI, Barreiros CDT, Barros JLN de, Silva FAC da, Ferreira ALCG, et al. Quality of life among university students with premenstrual syndrome. Rev Bras Ginecol E Obstetrícia 2019; 41(5):312-7. doi:10.1055/s-0039-1688 709.
- Pereira D, Pessoa AR, Madeira N, Macedo A, Pereira AT. Association between premenstrual dysphoric disorder and perinatal depression: A systematic review. Arch Womens Ment Health 2022; 25(1):61-70. doi:10.1007/s00737-021- 01177-6.
- Health MC for WM. Essential reads: Is PMDD a risk factor for postpartum depression? MGH center for women’s mental health. 2021. Available from: https://womensmentalhealth. org/posts/pmdd-postpartum-depression.
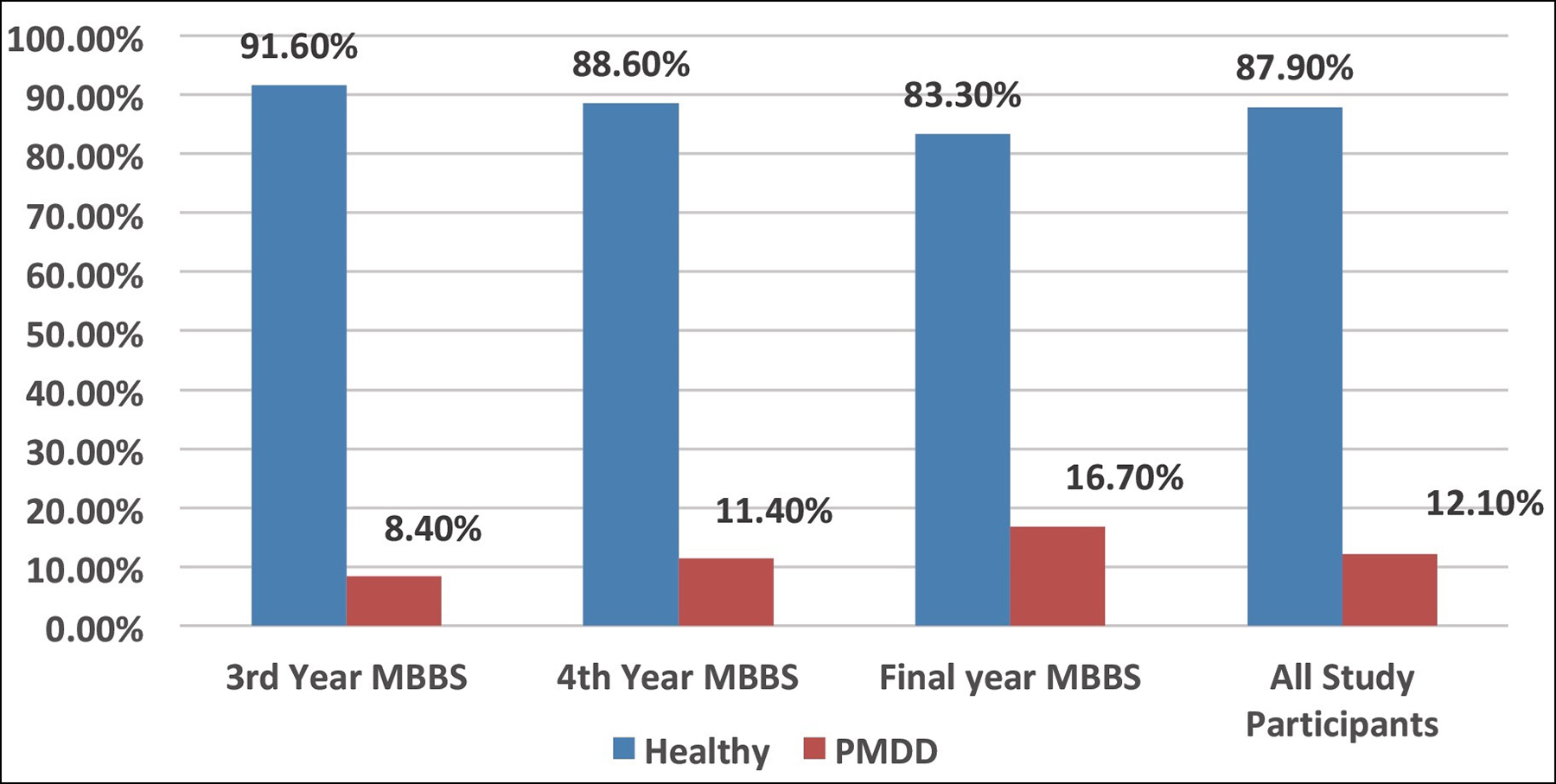 Figure 1: Distribution (%) of female medical students with and without PMDD in the last 3 years of MBBS.
Figure 1: Distribution (%) of female medical students with and without PMDD in the last 3 years of MBBS.