Flow-through Dorsoulnar Perforator Flap Repair of Soft-Tissue Defect of the Finger with Segmental Digital Arterial Defect
By Zonghai Jia, Gaofeng Liang, Chaopeng Duan, Zhao Zhang, Yongming Guo, Yunsheng TengAffiliations
doi: 10.29271/jcpsp.2022.05.685ABSTRACT
The aim of this study was to investigate the feasibility of transferring the free flow-through dorsoulnar perforator flap to reconstruct severely injured fingers. From January 2015 to March 2019, 16 patients, 16 thumb or fingers volar partial defects concomitant with segmental digital arterial defects, were included in this study. The flow-through dorsoulnar perforator flaps were used to repair the finger wounds and reconstruct digit arteries. Sixteen fingers in 16 patients were successfully reconstructed and all flaps survived completely. At the final follow-up, the appearance of the affected fingers was aesthetically pleasing. Two-point discrimination of the fingertips was 7.5-11.0 mm. According to the Total Active Motion (TAM) method: nine fingers were excellent, four were good, and three were fair. The free flow-through dorsoulnar perforator flap can achieve the goal of mending finger soft-tissue conditions complicated with segmental digital arterial defects with good results.
Key Words: Flow-through flaps, Perforator flap, Dorsoulnar artery, Soft-tissue defect.
Palmar digital soft-tissue defects are common injuries encountered in hand surgery that may result in disability if not managed properly.1 Finger injury can be complicated with segmental digital arterial defect, in which case it would be necessary to bridge the blood vessel to reconstruct the blood supply of the fingertip while covering the finger wound. A flow-through perforator flap, which contains a blood vessel can be anastomosed at both ends to provide a blood vessel bridge for supplying blood to the fingertip and be an optimal strategy for the treatment of soft-tissue defects of the finger complicated with segmental arterial defects.2 To the best of the authors’ knowledge, clinical reports of flow-through perforator flaps used in the repair of palmar digital soft-tissue defects concomitant with segmental digital arterial defects are rare. This study presented a single-center experience of the use of free flow-through dorsoulnar perforator flaps in the treatment of 16 patients with palmar digital soft-tissue defects complicated with segmental digital arterial defects.
This case study series was carried out at Xi’an 521 Hospital of Norinco Group, China, from January 2015 to March 2019, with the approval of the Hospital Ethics Committee. Written informed consent was also obtained from all patients. The inclusion criteria were palmar digital soft-tissue defects complicated with segmental digital arterial defects; and 14-65 years of age. The exclusion criteria were a previous history of trauma or surgery on the ulnar aspect of the distal forearm; clear mental or psychological disorders.
Preoperative examination of the perforator on the ulnar aspect of the distal forearm with a Doppler probe is vital. All operations were performed under brachial plexus block anesthesia. Under pneumatic tourniquet control, debridement, fixation of the phalanx fracture and tendon suture were performed firstly. Then the morphology and size of the palmar digital soft-tissue defects and the length of the segmental digital arterial defects were measured. Usually, two veins at the dorsal aspect of the recipient’s fingers should be dissected, because there are no comitant veins that are suitable to be anastomosed along the common digital artery. Under the supination position of the forearm, the longitudinal line between the pisiform and medial condyle of the humerous is the axis of the flap. First, the volar border of the flap was incised. The ulnar neurovascular bundle is confirmed besides the flexor carpi ulnaris. The dorsoulnar artery originates between 2 and 4 cm proximal to the pisiform as a branch of the ulnar artery. Then it gives off the ascending branch and descending branch.3 The dorsoular artery with two committing veins and two subcutaneous veins was dissected under the microscope. According to the length of the digital arterial defect of the affected finger, the trunk vessel from the beginning point of the dorsoulnar artery to the descending branch was dissected as the bridging vessel of the flow-through perforator flap (Figure 1-a). According to the morphology and size of the finger’s soft-tissue defect, the flap was harvested from the forearm. Donor sites up to 4 cm wide were closed directly. Sites wider than 4 cm are closed with skin grafting. After closing the finger defect with the flap, the microsurgical technique was used to anastomose the dissected artery and veins with 10-0 nylon suture (Figure 1-b). If complicated with the digital nerve defect, the sural nerve was transplanted from the lower limbs under block anesthesia to the digital nerve.
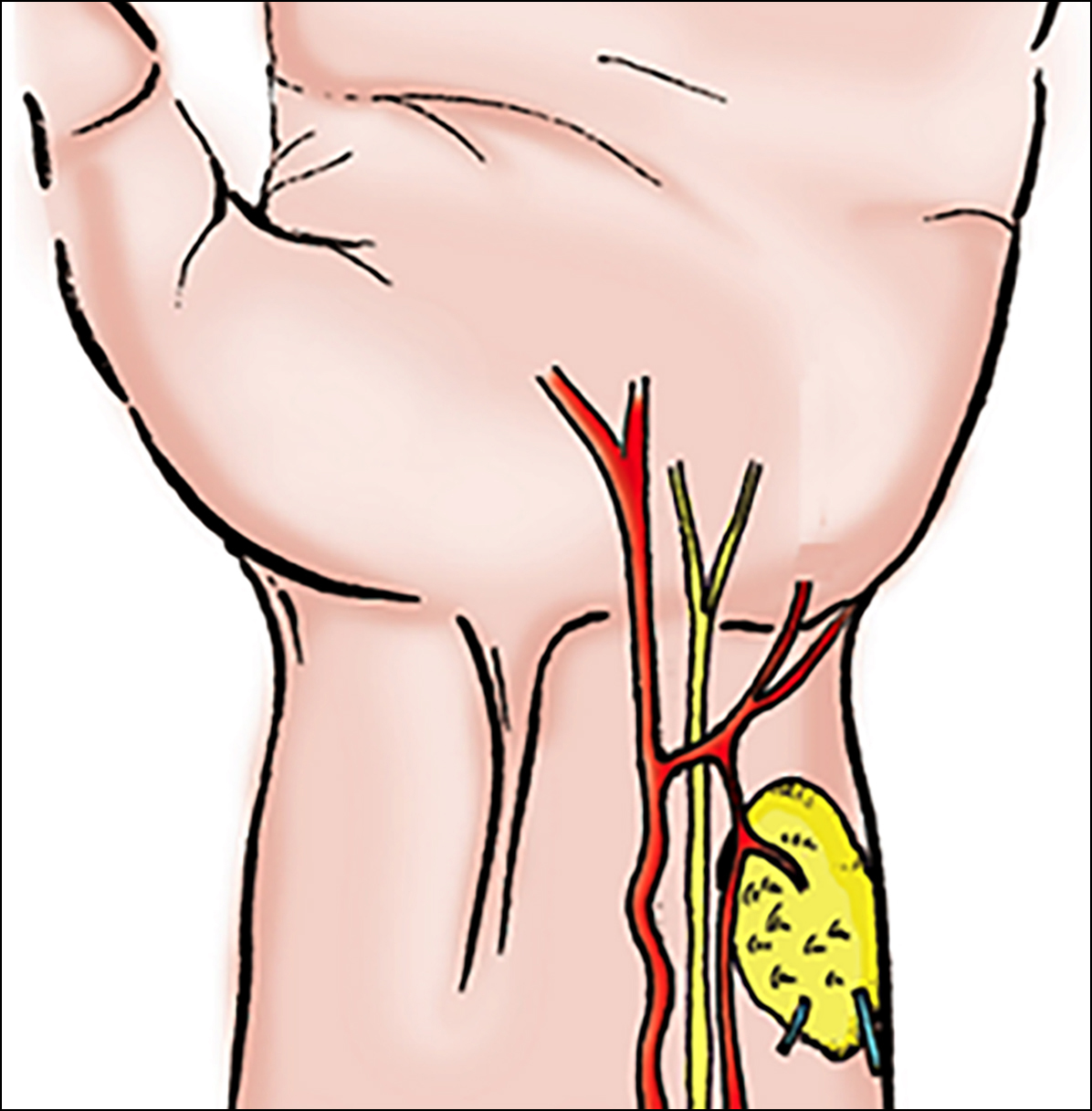 Figure 1-a: Sketch map of the free flow-through dorsoulnar perforator flap.
Figure 1-a: Sketch map of the free flow-through dorsoulnar perforator flap.
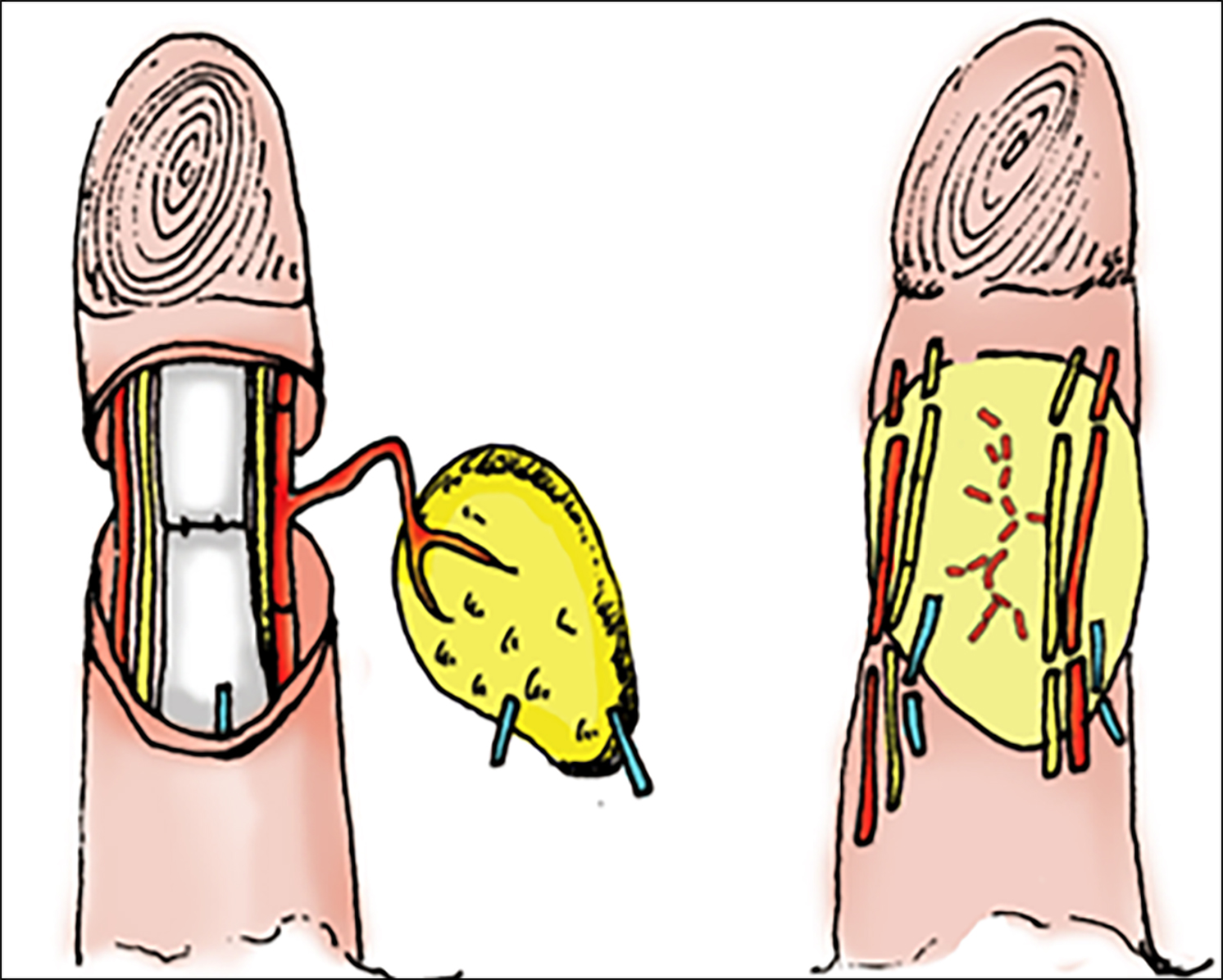 Figure 1-b: Sketch map of the flow-through dorsoulnar perforator flap to be transplanted to the recipient site.
Figure 1-b: Sketch map of the flow-through dorsoulnar perforator flap to be transplanted to the recipient site.
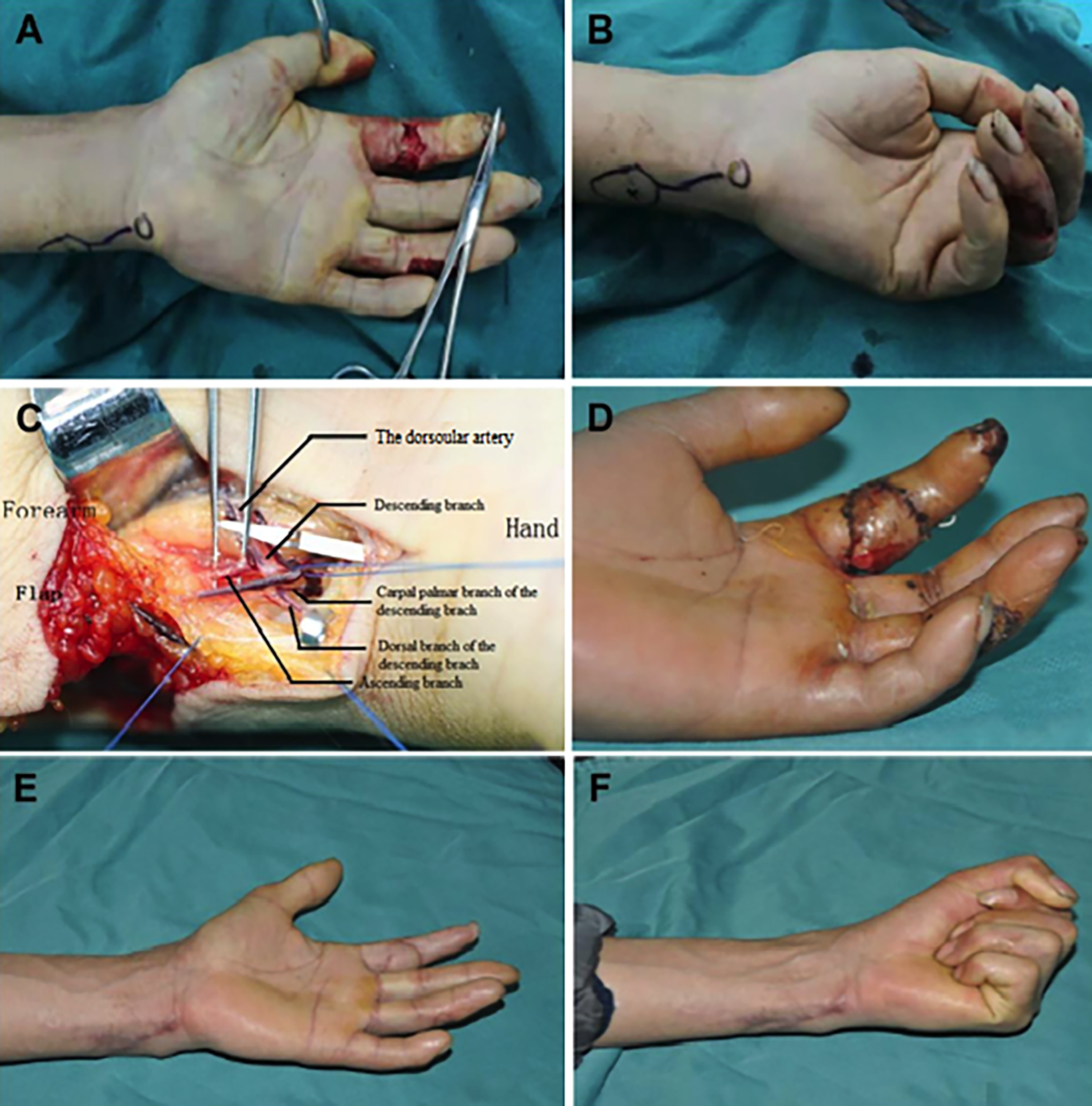 Figure 2: A typical case: A 46-year old male patient presented with soft tissue defect and segmental digital arterial defect in his left index finger caused by chainsaw injury. (a) Pre-operation appearance. (b) Intraoperative design of the free flow-through dorsoulnar perforator flap. (c) Exposure of the flap pedicle and bridging vessel. (d) Flap survival at two weeks after surgery. (e-f) One year after surgery, the affected finger and the donor site were satisfactory in appearance, and hand function recovered well.
Figure 2: A typical case: A 46-year old male patient presented with soft tissue defect and segmental digital arterial defect in his left index finger caused by chainsaw injury. (a) Pre-operation appearance. (b) Intraoperative design of the free flow-through dorsoulnar perforator flap. (c) Exposure of the flap pedicle and bridging vessel. (d) Flap survival at two weeks after surgery. (e-f) One year after surgery, the affected finger and the donor site were satisfactory in appearance, and hand function recovered well.
Between January 2015 and March 2019, 16 free flow-through dorsoulnar perforator flaps were used in 16 patients. There were nine men and seven women ranging from the age of 23 to 57 years, with an average age of 41 years. The affected digits included one thumb, seven index fingers, five middle fingers, and three ring fingers. The affected side was the right side in six patients and the left side in ten patients. Among them, twelve patients had bilateral segmental digital arteries defects and four patients had unilateral defects. The length of the vascular defect ranged from 1.0 to 2.5 cm, with an average length of 1.6 cm. The flap size ranged from 4.5 cm ×2.5 cm to 5.0 cm ×3.5cm and was transferred from the same forearm of the injured finger. All flaps survived and no complications related to the anastomosis were encountered in this study. Donor sites healed uneventfully. Follow-ups were conducted on all patients for at least 12 months. At the end of the follow-up period, the appearance of the affected fingers was aesthetic and cold intolerance did not appear in any of the patients. The surviving flaps were ruddy in color and soft in texture. The two-point discrimination of the fingertip was 7.5-11.0 mm, with an average of 9.0 mm. The hand function was evaluated by the TAM method: nine fingers were excellent, four were good, and three were fair. Linear scars were left at the donor site of the wrist, but all patients could resume their daily activities (Figure 2).
Flow-through flaps appear to be the best choice in extremity defects associated with common artery damage, because it can provide arterial reconstruction and soft-tissue coverage at the same stage.4 In this work, we presented our experience of using free flow-through dorso-ulnar perforator flaps in the reconstruction of sixteen cases of finger soft-tissue defects complicated with segmental digital arterial defects. Compared with other free flaps, the advantages of the flow-through dorsoulnar perforator flap are multifold. The position of the perforating vessel is relatively constant and easy to dissect. The arteriovenous diameter of the flap vessels is similar to that of the vessel in the recipient site, which is convenient for anastomosis. It does not injure the main trunk arteries. The donor and recipient sites are at the same operative field, which is convenient for anesthesia and operative procedures. The flap texture is close to the finger, and color matching is suitable for resurfacing a volar and lateral defect of the finger. The flap donor site is in a concealed area, and direct suture or skin grafting in the donor site can be performed.5 However, there are some disadvantages of such a flap technique as well. The length of the bridging vessel available for incision is limited. The maximum length in this study was about 2.5 cm. Scaring at the donor site of the wrist may result. An ultramicrosurgical technique will be required.
The following points should be noted in the procedures. First, the vascular pedicle should be dissected under the microscope. Second, the subcutaneous veins should be obtained in the flap as the main return vein to avoid postoperative flap edema. Third, a Doppler ultrasound must be used to locate the perforating branch before surgery to determine whether there is vascular variation.6 If the perforating branch cannot be confirmed, other flaps need to be used.
In summary, this study showed that the free flow-through dorsoulnar perforator flap procedure may be a valuable option to consider when repairing volar digital soft-tissue defects complicated with segmental arterial defects.
ETHICAL APPROVAL:
The study was conducted with the approval of the Hospital Ethics Committee.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
ZJ, GL: Drafted the work; analysed and interpretated date for the work.
CD, ZZ: Drafted the work, and revised critically.
YG: Contributed to the conception/design of the work and revised it critically.
YT: Drafted the work and finally approved to be published.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Rehim SA, Chung KC. Local flaps of the hand. Hand Clin 2014; 30(2):137-51, v. doi: 10.1016/j.hcl.2013.12.004.
- Xie H, Fang Q, Zhang D. Flow-through flap with wrist epithelial brach of ulnar artery for repair of finger soft tissue defect: A cases series. Am J Transl Res 2021; 13 (8):9826-30.
- Zhao M, Tian D, Shao X, Li D, Li J, Liu J, et al. Anatomic study on micro transverse flap pedicled with superfical palmar branch of radial artery from palmar wrist. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013; 27(7):864-8.
- Inada Y, Tamai S, Kawanishi K, Omokawa S, Akahane M, Shimobayashi M, et al. Free dorsoulnar perforator flap transfers for the reconstruction of severely injured digits. Plast Reconstr Surg 2004; 114(2): 411-20. doi: 10.1097/01. prs.0000131881.42438.93.
- Pan XP, Wang M, Shi W. Application of flap with supra-carpal cutaneous branch of ulnar artery in severe mutilating hand injury. Chin J Microsurg 2018; 41:264-5.
- Ju JH, Jin GZ, Li L. Blood vessel variation and treatment during the transferring of skin flap pedicled with dorsal carpal branch of ulnar artery. Chin J Clin Anat 2008; 26:341-3.