Enhancing Empathy in Medical Students by Focused Learner Centered Activities
By Nabia Tariq1, Ali Tayyab2, Tara Jaffery3, Amena Masrur1Affiliations
doi: 10.29271/jcpsp.2023.01.83ABSTRACT
Objectives: To determine the change in empathy levels of medical students during their progress in professional years internship, and to examine change in empathy after targeted empathy enhancing activities during the course of medical school.
Study Design: Longitudinal Study.
Place and Duration of Study: Shifa College of Medicine/ Shifa Tameer-e-Millat University, Islamabad, from January 2015 to December 2019.
Methodology: Student version of Jefferson Scale of Physician Empathy was administered sequentially from 2015 to 2019 which evaluated the change in empathy of medical students in a class of 2019. Targeted empathy-enhancing activities included patient-centered module in year-three and stress management workshops in the final year of medical school.
Results: Empathy scores rose from the first year of study (4.27 ±0.38) to the third year (4.52 ±0.70). It fell over the next two years of study (4.25 ±0.62 & 4.21 ±0.40) before rising again during the internship (4.39 ±0.43) with focused empathy-enhancing activities.
Conclusion: Patient-centered module which focused on activities that help develop empathy may have been a factor in the increase of empathy scores in the third year and internship. Placing recurring formal activities throughout all clinical years may help in enhancing empathy in medical students.
Key Words: Medical student empathy, Empathy enhancing targeted activities, JSPE.
INTRODUCTION
The word empathy is a complex, multidimensional concept, involving the ethical, affective (emotional), cognitive (knowledge), and behavioural (action) domains of an individual's psychology.1 Clinical empathy is however the application of this process of understanding and interaction by a physician in his/her meetings with patients and their families.2 Healthcare professional empathy contributes to positive clinical outcomes through mutual trust, shared decision making, and better compliance to management strategy. Moreover, the professional competence of a physician is strongly linked with compassion for dignity of patients and respect for human rights.3
There is a lot of interest in studying empathy development among medical students. Numerous studies have reported a declining trend in empathy during the medical school years.4-6 A systemic review from 1990-2010 also supported this declining trend in self-assessed empathy by medical students and trainees.7 Many causes contributing to declining empathy have been identified including dearth of mentors, overwhelming clinical responsibilities and social commitments.8 Some unscrupulous behaviours during medical school were held responsible for declining empathy and unprofessional attitude.9 Further, these may further lead to patient displeasure and even medical mistakes.10 Moreover, empathy is considered to be both a personal trait and an appreciable skill, therefore deliberate practice of empathy is connected with better-quality patient care and better physician’s health, well-being, and professional contentment.11
These findings are concerning and medical educationists and leaders in healthcare, need to focus on strategies for enrichment of empathy in people linked to the medical profession.
Nurturing empathy in medical training as the art of history taking and doing physical examinations are considered necessary for patient satisfaction and better therapeutic outcome.12 Many studies have supported empathy-enhancing interventions for undergraduate medical students.13 These interventions range from experiential learning exercises with simulated patients, focus on communication skill, reflective writing exercises, and role playing.1 Such approaches seemed to be effective for enhancing empathy in medical students.14 In clinical years accompanying the physicians may have an impact on emotive and cognitive dimensions of empathy, further studies are required to ascertain the long-term impact of these strategies on professional practice.
In Pakistan, a few studies on the current subject found revealed significantly low levels of empathy in medical students.15,16 Though the studies are few with small samples, however, the findings are alarming. They reflect on the need to focus on developing students’ empathy in the medical curriculum. With this background, this longitudinal interventional study was designed to examine empathy change in medical students over five years of undergraduate training and internship by introducing a patient-centered module involving small group workshops on reflective writing, communication skills, ethics and humanities at the start of their clinical training (third year) and a stress management workshop during the final year of their undergraduate training, prior to their graduation.
METHODOLOGY
Approval for this longitudinal study was taken from the Institutional Review Board. The class of 2019 (admitting session 2014) admitted by Shifa Tameer-e-Millat University in its constituent medical college; Shifa College of Medicine, Islamabad Pakistan, was selected for this study. Objectives as well as instructions on how to fill out the survey were posted on the student e-portal. There was no obligation on the students to complete the survey, nor was there any monetary benefit associated with it. All of the students who agreed to become participants were included in the study. Students who did not agree were excluded. Voluntary sampling was employed to select the cases for the study. The survey was repeated and data were collected in years 2016, 2017, 2018 (duration of MBBS program), and 2019 (internship year (house job year)) at Shifa International Hospital, Islamabad Pakistan. Targeted empathy- enhancing activities were planned in year 3 (Weekly Patient Centered Learning workshops spread over 6 weeks) and in year 5 (one-day stress management workshop aimed at identifying their stressors and practising coping strategies for relieving stress).
The student version of the Jefferson Scale of Physician Empathy (JSPE) was used and made available to the students electronically via their portal. JSPE is a self-reported standardised questionnaire for empathy assessment, made up of 20 questions that are replied to using a 7-point Likert Scale.4 The questionnaire consists of both positive and negative items, which are equally phrased to reduce bias (response and acquiescent). In addition to the JSPE scores, the student demographic data were also collected (gender and age).
Data were analysed using SPSS V20. Response rate in each year was reported as percentage. JSPE scores were reported as mean with standard deviation (out of a maximum possible score of 7). To test whether there was a significant change in empathy levels over the period of study (taking into account only the students who had completed all of the questionnaires from year 1 to internship year) Repeated Measures ANOVA was employed. A p-value of <0.05 was taken as significant.
In addition, a comparison of responses to individual question of the JSPE through all five years was also looked at to note any change in the pattern of their responses.
RESULTS
The number of participants in the class of 2019 was 99. Completed surveys and their score distribution are shown in Table I. There were 43 (43.43%) male students and 56 (56.57%) female students in the class.
The mean empathy scores, per question, over the period of study are graphically represented in Figure 1.
Table I: Response rate and score distribution of all participants.
|
Year |
Respondents |
Total Participants in Class |
Response Rate (%) |
Mean Score (±SD) |
|
1 |
83 |
99 |
83.83 |
4.27 (±0.38) |
|
3 |
81 |
81.81 |
4.52 (±0.70) |
|
|
4 |
99 |
100 |
4.25 (±0.62) |
|
|
5 |
99 |
100 |
4.21 (±0.40) |
|
|
Internship |
71 |
71.71 |
4.39 (±0.43) |
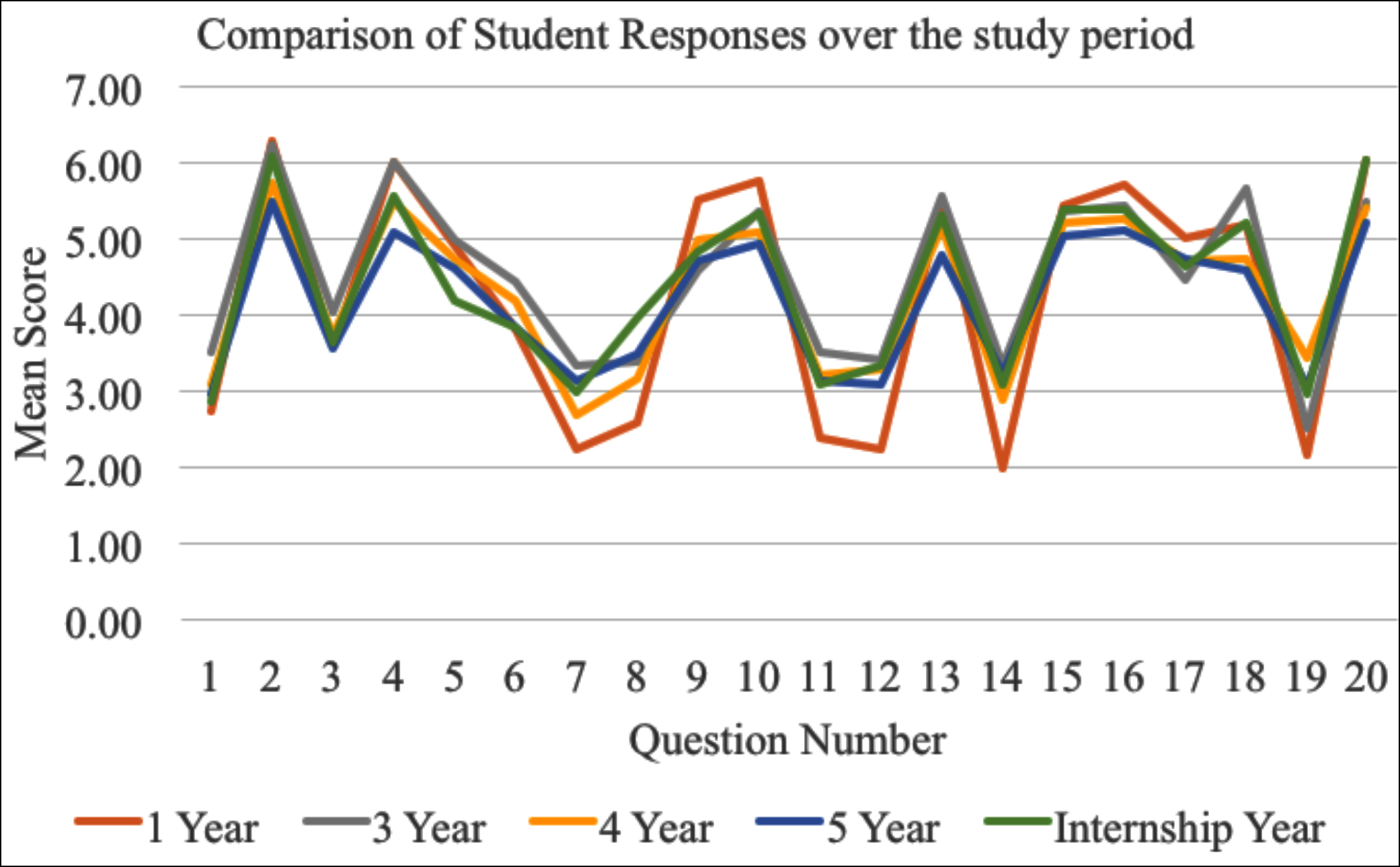 Figure 1: Mean empathy scores, per question, of participants over the course of the study period.
Figure 1: Mean empathy scores, per question, of participants over the course of the study period.
Only the participants (n = 70) who had completed all the questionnaires every year, from year 1 to internship year were taken into account to explore the change in empathy (if any) over this period of time.
The empathy scores of students rise when comparing the first year of study to the third. It falls off over the next two years of study (years 4 and 5) before rising during the internship. To elucidate whether there were significant differences in the scores over the period of the investigations, the scores were paired as preceding-proceeding for comparison.
Repeated Measures ANOVA showed a statistically significant difference in empathy scores over the span of the study [F (3.04, 209.85) = 4.63, p=0.004]. The difference lies between scores of Years 1 and 3 (p = 0.04), no significant difference was seen in any of the other comparisons (Table II).
The comparison of mean score of student responses to individual question was consistent throughout the 5 years and is shown in Figure 2.
Table II: Repeated Measures ANOVA (Bonferroni post hoc test) for comparison of scores of participants who completed the questionnaire across their years of study and internship (n = 70).
|
Comparison |
Mean Score (±SD) |
p-value |
|
Years 1 & 3 |
Year 1: 4.24 (±0.35) Year 3: 4.54 (±0.75) |
0.04 |
|
Years 3 & 4 |
Year 3: 4.54 (±0.75) Year 4: 4.21 (±0.65) |
0.11 |
|
Years 4 & 5 |
Year 4: 4.21 (±0.65) Year 5: 4.22 (±0.42) |
>0.99 |
|
Years 5 & Internship |
Year 5: 4.22 (±0.42) Internship: 4.39 (±0.44) |
0.27 |
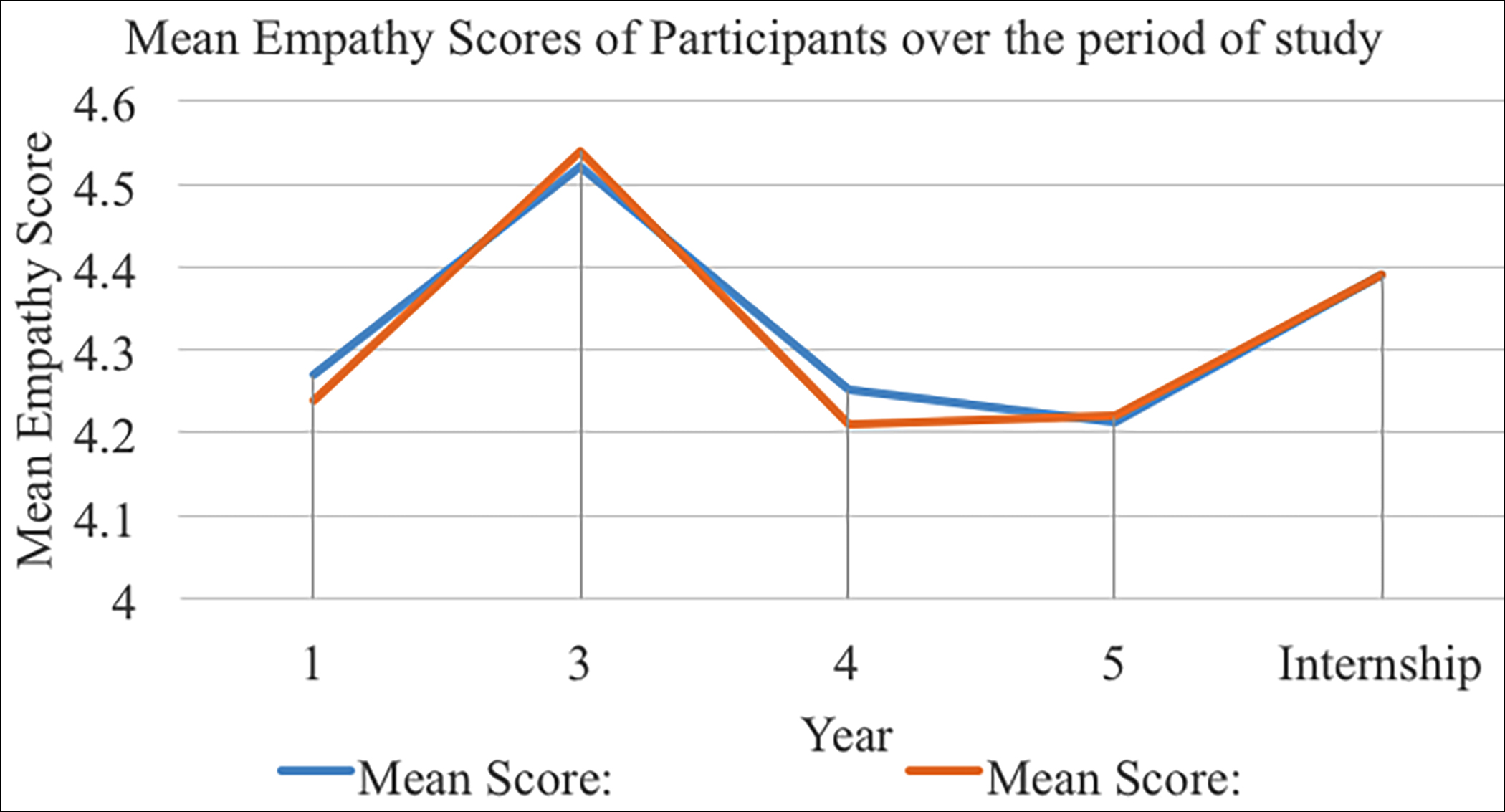 Figure 2: Comparison of student responses to questions over the period of study. Arrowheads indicate curricular interventions relating to empathy training of participants.
Figure 2: Comparison of student responses to questions over the period of study. Arrowheads indicate curricular interventions relating to empathy training of participants.
DISCUSSION
The current study looks at the changes in empathy in a cohort of students through their 5 years of MBBS and their mandatory internship year. The authors looked at the possible- impact of patient-centered module at the start of their clinical exposure in year three and a stress management workshop in year five on students’ empathy scores.
Medical students entering the medical school in this study did not score high comparing to the mean value documented in different studies.4,17
That is possible because students are not answering on extremes of the Likert scale. However, the trends graph in Figure 2 is showing that the study participants are consistently giving the appropriate answer to all the questions. This maybe due to the reason that the scores are actually more cultural, meaning they do not like to give extreme answers in Likert? The trends graph is showing their responses are all in the “appropriate” direction in all years.
In a previous study regarding measuring empathy scores in Pakistani students, it was found that these low baseline empathy scores further drop down during the medical school progression.16
Comparing with the international literature, there seems to be no uniform pattern of self-rating of empathy during medical school in the majority of the studies, some show slight enhancement in empathy while a very few reports decline in empathy during the course of medical school.18 In an Indian study, a progressive drop in empathy was noted with the increasing medical school years.19 Whereas, in two American studies an apparent decline in empathy was documented during the medical school years.4,20 Statistically insignificant deviations are reported from European Countries.21,22
To look at the possible impact of interventions on students’ empathy scores, authors’ first intervention was introducing patient-centered module at the beginning of clinical exposure i.e., year three (Figure 2, left arrowhead). This module included components which have been shown in the literature to enhance empathy i.e.; reflective writing, role play, humanities, and communication skills.23 Therefore, a significant rise of empathy scores was noted in the third year after exposure to the patient-centered module. Similar results were documented by Schweller et al. where the skill of reflection in medical students helped in enhancing short- term empathy.24 In contrast Hojat et al. showed the targeted activities to help in the sustainability of enhancing empathy.25
However, this rise of empathy in the current study was not found sustainable during the next two years of clerkship. When a steady decline in empathy scores in years four and five were noted which is consistent with the previous studies supporting decline and gradual fading away of empathy during medical students’ clinical years.4,5,22
In analysing the basis of the deterioration in empathy among medical students, researchers speculate that it could be due to, brief community associations, hassled and sparse doctor-patient interactions, and evasion of understanding while getting trained in Medicine. Stress is also suspected of affecting at least some undergraduates badly. Studies on western graduates generally reveal a decline during the medical school years.4,7
The evidence supports the view that exposure to stressful patient conditions, prolonged job hours and sleep deprivation may result in a decline in empathy. Failure to timely address these issues may result in the development of maladaptive solutions, with a consequential diminution of empathy.
In continuation to patient-centered module stress management workshop was planned when the class was in the final year specifically aimed at enlightening them to diagnose stress and practising small targeted stress-relieving activities (right arrowhead). This activity did not immediately help in enhancing empathy, however, after a few months when JSPE was administered for the last time in internship it showed better empathy which may be partly from learning coping mechanisms for relieving stress or feeling of more empowerment in handling stressful patient conditions.
Therefore, this activity may help in enhancing empathy scores by learning coping strategies based on emotional distancing.13,20
From a student’s perspective, their perception was that their empathy did not worsen, instead, increased workload and dealing with the grief of patients and their families reduced the display of empathy. This study helps demonstrate that incorporating recurring empathy enhancing activities into the medical school curriculum longitudinally across the course of training may help in the development of empathy in students. These activities will also reduce students’ distress and promote student well-being and professionalism along with enhancing empathy.
Since the survey was entirely voluntary the students were under no obligation to complete it. Nor was there any financial or other reward attached to completing the survey. This led to variable attrition rates over the years the survey was repeated. The initial survey was completed by 83 students in year 1 out of a class of 99. This remained largely unchanged when the survey was repeated in year 3 (completed surveys 81). During the clinical years (years 4 and 5) the entire class returned the survey most likely due to exposure to an environment where practical demonstration (or lack thereof) of empathy was evident. Since all students did not complete their internship at Shifa International Hospital, the number of returned surveys dropped to 70.
This was a six-year longitudinal study of a single medical school of Pakistan. Therefore, the results of this study may not represent all the medical students of Pakistan.
It was attempted to incorporate a few empathy-enhancing activities in the curriculum to look at its impact on the curriculum and the same questionnaire was repeated every year so familiarity with the questions might affect the results. Since participation in the study was voluntary therefore less sample size might purge the data.
CONCLUSION
Students demonstrated positive empathy trends which were consistent with the three subcomponents of the JSPE student questionnaire throughout their years of MBBS education. There was a statistically significant increase in empathy between years one and three. A patient-centered module which focused on activities that help develop empathy may have been a factor in the increase of empathy scores in the third year. Placing recurring formal activities throughout all clinical years may help in enhancing empathy in medical students.
ACKNOWLEDGEMENTS:
The authors are greatly indebted to Jefferson University for permitting them to use Empathy Scale Questionnaire Student Version.
ETHITCAL APPROVAL:
Approval for this longitudinal study was taken from the Institutional Review Board.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
NT: Study concept, design, questionnaire review, research proposal for ethics committee review, and first draft. The author over-saw the work done by other authors in the study.|
AT: Responsible for review of study design, and general management of the study as it progressed including management of statistical database, and ensuring timelines were being met.
TJ: Responsible for reviewing the first draft, cross-checking and finalisation of references and statistics, and finalisation of the manuscript.
AM: Responsible for literature review and editing of the manuscript and responsible for updating and maintaining the database for this study.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Tan L, Le MK, Yu CC, Liaw S Y, Tierney T, Ho YY, et al. Defining clinical empathy: A grounded theory approach from the perspective of healthcare workers and patients in a multicultural setting. BMJ Open 2021; 11(9):e045224. doi: 10.1136/bmjopen-2020-045224.
- Shamim MS. Clinical empathy in graduate medical education. J Dow Uni Health Sci 2018; 12:30-2.
- Stebletsova, A., Torubarova, I. Empathy development through ESP: A pilot study. J Educational Cultural Psychological Studies 2017; 0(16):237-49. doi.org/10. 7358/ecps-2017-016-steb.
- Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad Med 2009; 84(9):1182-91. doi: 10.1097/ACM. 0b013e3181b17e55.
- Neumann M, Edelhauser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad Med 2011; 86(8):996-1009. doi: 10. 1097/ACM.0b013e318221e615.
- Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: A systematic review. Medical Education 2016; 50(3):300-10. doi: 10.1111/medu.12806.
- Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the "nature" and "specific effectiveness" of clinical empathy: A theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns 2009; 74(3):339-46. doi: 10.1016/j.pec.2008.11.013.
- Dyrbye LN, Massie FS, Eacker A, Harper W, Power D, Durning SJ, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA 2010; 304(11):1173-80. doi: 10.1001/jama. 2010.1318.
- Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One 2013; 8(4). doi: 10.1371/journal. pone.0061526.
- Kliszcz J, Nowicka-Sauer K, Trzeciak B, Nowak P, Sadowska A. Empathy in healthcare providers-validation study of the polish version of the Jefferson Scale of Empathy. Adv Med Sci 2006; 51:219-25.
- Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: An updated, systematic review. Acad Med 2013; 88(8):1171-7. doi: 10.1097/ACM.0b013e318299f3e3.
- Jani BD, Blane DN, Mercer SW. The role of empathy in therapy and the physician-patient relationship. Forsch Komplementmed 2012; 19(5):252-7. doi: 10.1159/ 000342998.
- Garden R. Expanding clinical empathy: An activist perspective. J Gen Intern Med 2009; 24(1):122-5. doi: 10.1007/s11606-008-0849-9.
- Stepien KA, Baernstein A. Educating for empathy. A review. J Gen Intern Med 2006; 21(5):524-30. doi: 10.1111/j. 1525-1497.2006.00443.x.
- Tariq N, Rasheed T, Tavakol M. A Quantitative study of empathy in pakistani medical students: A multicentered approach. J Prim Care Community Health 2017; 8(4):294-9. doi: 10.1177/2150131917716233.
- Tariq N, Tayyab A, Jaffery T. Differences in empathy levels of medical students based on gender, year of medical school and career choice. J Coll Physicians Surg Pak 2018; 28(4):310-3. doi: 10.29271/jcpsp.2018.04.310.
- LoSasso AA, Lamberton CE, Sammon M, Berg KT, Caruso JW, Cass J, et al. Enhancing student empathetic engagement, history-taking, and communication skills during electronic medical record use in patient care. Acad Med 2017; 92(7):1022-7. doi: 10.1097/ACM.000000000 0001476.
- Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: A scoping review. Adv Health Sci Educ Theory Pract 2017; 22(5):1293-1313. doi: 10.1007/s10459-016-9704-7.
- Shashikumar R, Chaudhary R, Ryali VS, Bhat PS, Srivastava K, Prakash J, et al. Cross sectional assessment of empathy among undergraduates from a medical college. Med J Armed Forces India 2014; 70(2):179-85. doi: 10.1016/j. mjafi.2014.02.005.
- Chen DC, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school. Med Teach 2012; 34(4):305-11. doi: 10.3109/0142159X.2012.644600.
- Costa P, Magalhaes E, Costa MJ. A latent growth model suggests that empathy of medical students does not decline over time. Adv Health Sci Educ Theory Pract 2013; 18(3):509-22. doi: 10.1007/s10459-012-9390-z.
- Quince TA, Parker RA, Wood DF, Benson JA. Stability of empathy among undergraduate medical students: A longitudinal study at one UK medical school. BMC Med Educ 2011; 11:90. doi: 10.1186/1472-6920-11-90.
- Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: A systematic review. BMC Med Educ 2014; 14:219. doi: 10.1186/1472-6920-14-219.
- Schweller M, Costa FO, Antônio MÂ, Amaral EM, de Carvalho-Filho MA. The impact of simulated medical consultations on the empathy levels of students at one medical school. Acad Med 2014; 89(4):632-7. doi: 10. 1097/ACM.0000000000000175.
- Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach 2013; 35(12):996-1001. doi: 10.3109/0142159X.2013.802 300.