Effect of Local Use of Rifampicin on the Development of Surgical Site Infection after Lumbar Microdiscectomy
By Eyup Cetin1, Murat Yucel2Affiliations
doi: 10.29271/jcpsp.2022.10.1284ABSTRACT
Objective: To investigate the effect of local use of rifampicin (RIF) on the development of postoperative surgical site infection (SSI) after lumbar microdiscectomy.
Study Design: Observational study.
Place and Duration of Study: Van YuzuncuYil University Medical School Neurosurgery Clinic, between 2020 and 2022.
Methodology: This retrospective study reviewed the clinical and laboratory records of 178 patients who underwent lumbar microsurgery. After lumbar microsurgery, one ampoule of rifampicin (RIF) (250 mg) was locally injected into the surgical site in 62 patients (RIF group), while the remaining 116 patients (non-RIF group) received no injection into the surgical site after lumbar microsurgery. Normal distribution of data was analysed using Kolmogorov-Smirnov test. Continuous variables were compared using Mann-Whitney U test and categorical variables were compared using chi-square test or Fisher’s exact test as needed.
Results: In the postoperative period, local infection developed in one patient in the RIF group, while local infection developed in 11 and deep infection developed in three of the patients in the non-RIF group. Moreover, the risk of local infection development was significantly higher in the non-RIF group compared to the RIF group. The rate of superficial SSI was lower in the RIF group compared to the non-RIF group. No significant difference was observed between the two groups with regard to the rate of deep SSI.
Conclusion: Postoperative infection is an extremely important clinical condition manifesting in the form of superficial or deep SSI. The utmost care and necessary precautions should be taken to avoid postoperative infections. Intraoperative antibiotic prophylaxis is the most effective method in preventing postoperative spinal infections.
Key Words: Infection, Lumbar microdiscectomy, Rifampicin, Local infection, Deep infection.
INTRODUCTION
Surgical site infection (SSI) is an undesirable postoperative complication in patients undergoing spine surgery. Postoperative spinal infections rarely require long-term hospital treatment and may result in loss of labour.1
Conservative treatment is the primary method of choice in the treatment of lumbar disc herniation (LDH). In patients whose symptoms persist despite conservative treatment, surgical treatment can be performed for reasons such as progression of motor deficits (PMD) and cauda equina syndrome (CES). Classical microdiscectomy is the most commonly preferred surgical technique.
Common complications seen after microdiscectomy include superficial SSI, deep SSI, PMD, development of empty fistula, and LDH recurrence.2 Recent studies have shown that the incidence of SSI after spine surgery ranges from 0.7% to 11.6%.3
Spinal infections are mostly seen between three days and three months after surgery. Factors increasing the incidence of spinal infections include advanced age, intravenous drug use, long-term systemic steroid use, diabetes, organ transplantation, malnutrition, prolonged surgeries, excessive blood loss, instrumentation, and prior surgeries.4 Due to their close proximity to the neurological structures in the spine to each other, postoperative infections are likely to cause undesirable outcomes.5
The present study was designed to investigate the effect of local use of rifampicin (RIF) in the surgical site after lumbar microdiscectomy on the development of postoperative SSI.
METHODOLOGY
After lumbar microsurgery, one ampoule of rifampicin (RIF) (250 mg) was locally injected into the surgical site in 62 patients (RIF group) and the remaining 116 patients (non-RIF group) received no injection into the surgical site. The retrospective study reviewed the clinical and laboratory records of 178 patients that underwent lumbar microsurgery in Van Yuzuncu Yil University Medical School Neurosurgery Clinic, between 2020 and 2022. All patients who underwent lumbar microdiscectomy with or without RIF were included in the study regardless of age. Patients with incomplete records and who had surgery other than lumbar microdiscectomy were excluded.
Surgical data including time from surgery to the diagnosis of SSI, presence of fever, antibiogram results, comorbidity status, and the duration of intravenous (IV) or oral antibiotic use were recorded for each patient. Laboratory parameters including white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level were followed up regularly both before and after surgery.
Data were analysed using SPSS for Windows version 28.0 (Armonk, NY: IBM Corp.). Descriptives were expressed as mean, standard deviation (SD), median, minimum-maximum, frequencies (n), and percentages (%). Normal distribution of data was analysed using Kolmogorov-Smirnov test. Continuous variables were compared using Mann-Whitney U test and categorical variables were compared using chi-square test or Fisher’s exact test as needed. A p-value of <0.05 was considered significant.
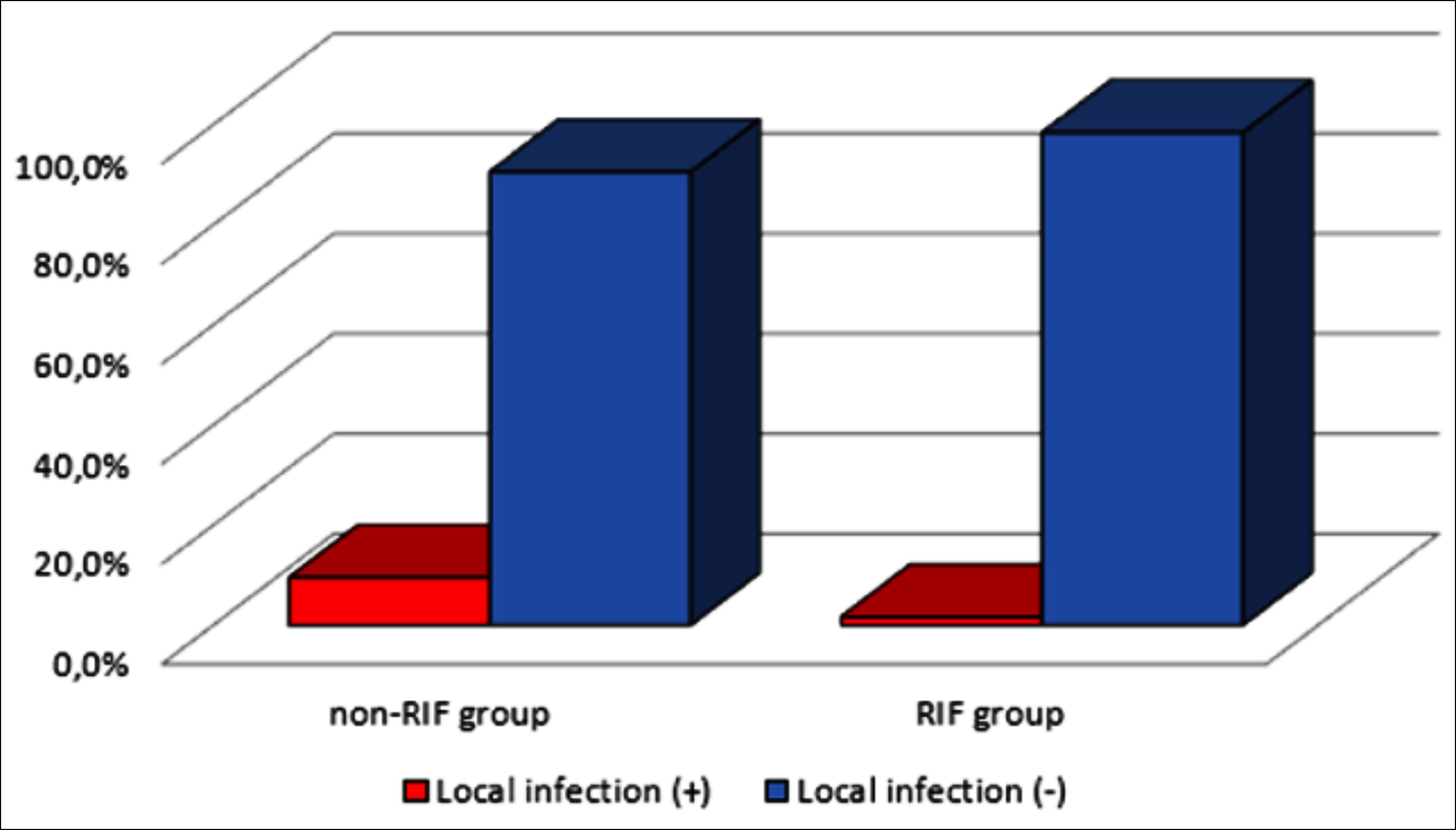 Figure 1: Rates of local infection.
Figure 1: Rates of local infection.
RESULTS
No significant difference was observed between the RIF and non-RIF groups with regard to age and gender distribution and the rate of dural injury (p>0.05 for all). However, the duration of surgery was significantly lower in the RIF group compared to the non-RIF group (p<0.05, Table I).
No significant difference was observed between the two groups with regard to the prevalence of diabetes, hyperthyroidism, and asthma (p>0.05 for all), while the prevalence of hypertension was significantly lower in the RIF group compared to the non-RIF group (p<0.05, Table I).
The rate of superficial SSI was significantly lower in the RIF group compared to the non-RIF group (p<0.05). By contrast, no significant difference was observed between the two groups with regard to the rate of deep SSI (Table I and Figure 1).
Although no significant difference was found between the two groups with regard to the prevalence of SSI, wound culture positivity, and LDH recurrence (p>0.05 for all), the length of hospital stay was significantly shorter in the RIF group compared to the non-RIF group (p<0.05, Table I).
DISCUSSION
Literature indicates that the postoperative infection rate is less than 2% after minimally invasive surgical interventions such as laminectomy and discectomy, while it can be as high as 10% after complex spinal surgical interventions.6
Rifampicin (RIF) is an antibacterial agent with activity against many gram-positive cocci, mycobacteria, clostridium difficile, and selected gram-negative organisms found on the skin.7 RIF inhibits DNA-directed RNA synthesis by interacting with the β-subunit of RNA polymerase.8 Topical therapy generally allows the use of antimicrobials in relatively high concentrations at wound sites compared to systemic therapy.9 However, high antimicrobial concentrations can cause cytotoxic effects on skin cells and inhibit rapid wound healing.10
In a study by Fang et al., significant risk factors for infection after spinal surgery were reported at age over 60 years, diabetes mellitus, high body mass index, smoking, alcohol abuse, duration of surgery, wound size, retraction strength and time, use of monopolar cautery, cerebrospinal fluid (CSF) leakage, and previous surgical interventions.11
The effect of intraoperative use of antibacterial washing solutions on the postoperative infection has not been fully elucidated. However, irrigation of the surgical site with saline solution during the surgery is recommended as it reduces the infection rate.5
A study by Tronnier et al. reported that disc space infection was observed in 0.2-1.2% of the cases that underwent disc space irrigation with bacitracin or neomycin after discectomy.12 Tas et al. evaluated the effect of locally used silver nanoparticles on the development of infection in a rat model of spinal stabilisation and infection and reported that the nanoparticles reduced the risk of infection development.13
In the present study, one ampoule of RIF (250 mg) was locally injected into the surgical site in 62 patients (RIF group), while the remaining 116 patients (non-RIF group) received no injection into the surgical site after lumbar microsurgery. In the postoperative period, local infection developed in one patient in the RIF group, while local infection developed in 11 and deep infection developed in three of the patients in the non-RIF group. Moreover, the risk of local infection development was significantly higher in the non-RIF group compared to the RIF group. Pre- and intra-operative antibiotic prophylaxis is the most effective factor in preventing postoperative spinal infections.14 A study by Diren et al. showed that a single dose of prophylactic antibiotic administered only during the induction of anaesthesia did not increase the rate of spondylodiscitis when compared to the rates reported in the literature.15
Table I. Demographic and clinical characteristics.
|
|
Use of rifampicin |
||||||||||||||||||||||
|
Non-RIF group |
|
RIF group |
|||||||||||||||||||||
|
Ort.±ss/n-% |
Medyan |
Min-Mak |
I.Q-3.Q |
|
Ort.±ss/n-% |
Medyan |
Min-Mak |
I.Q-3.Q |
p |
||||||||||||||
|
Age (years) |
47.9 |
± |
13.7 |
46.0 |
17.0 |
- |
85.0 |
38.0 |
- |
54.8 |
46.8 |
± |
14.0 |
45.0 |
16.0 |
- |
81.0 |
36.0 |
- |
56.0 |
0.687m |
||
|
Gender |
Famale |
50 |
|
43.1% |
|
|
|
|
|
|
|
|
35 |
|
56.5% |
|
|
|
|
|
|
|
0.089X2 |
|
Male |
66 |
|
56.9% |
|
|
|
|
|
|
|
|
27 |
|
43.5% |
|
|
|
|
|
|
|
||
|
Duration of surgery (min) |
132.5 |
± |
38.95 |
120.0 |
60.0 |
- |
300.0 |
120.0 |
- |
144.5 |
102.7 |
± |
34.6 |
120.0 |
50.0 |
- |
180.0 |
60.0 |
- |
120.0 |
<0.001m |
||
|
Length of hospital stay (days) |
2.54 |
± |
1.70 |
2.0 |
1 |
- |
13 |
1.00 |
- |
3.00 |
|
1.59 |
± |
1.70 |
1.00 |
1 |
- |
10 |
1.00 |
- |
1.00 |
<0.001m |
|
|
Dural injury |
Yok |
111 |
|
95.7% |
|
|
|
|
|
|
|
|
56 |
|
90.3% |
|
|
|
|
|
|
|
0.157X2 |
|
Var |
5 |
|
4.3% |
|
|
|
|
|
|
|
|
6 |
|
9.7% |
|
|
|
|
|
|
|
||
|
Systemic diseas |
Yok |
106 |
|
91.4% |
|
|
|
|
|
|
|
|
54 |
|
87.1% |
|
|
|
|
|
|
|
0.367X2 |
|
Var |
10 |
|
8.6% |
|
|
|
|
|
|
|
|
8 |
|
12.9% |
|
|
|
|
|
|
|
||
|
Asthma |
Var |
1 |
|
10.0% |
|
|
|
|
|
|
|
|
0 |
|
0.0% |
|
|
|
|
|
|
|
>0.99X2 |
|
Yok |
9 |
90.0% |
8 |
100.0% |
|||||||||||||||||||
|
HT |
Var |
8 |
|
80.0% |
|
|
|
|
|
|
|
|
1 |
|
12.5% |
|
|
|
|
|
|
|
0.004X2 |
|
Yok |
2 |
|
20.0% |
|
|
|
|
|
|
|
|
7 |
|
87.5% |
|
|
|
|
|
|
|
||
|
DM |
Var |
2 |
|
20.0% |
|
|
|
|
|
|
|
|
5 |
|
62.5% |
|
|
|
|
|
|
|
0.145X2 |
|
Yok |
8 |
|
80.0% |
|
|
|
|
|
|
|
|
3 |
|
37.5% |
|
|
|
|
|
|
|
||
|
Hypothyroidism |
Var |
0 |
0.0% |
2 |
25.0% |
0.183X2 |
|||||||||||||||||
|
Yok |
10 |
100.0% |
6 |
75.0% |
|||||||||||||||||||
|
Local infection |
Var |
11 |
|
9.5% |
|
|
|
|
|
|
|
|
1 |
|
1.6% |
|
|
|
|
|
|
|
0.046X2 |
|
Yok |
105 |
|
90.5% |
|
|
|
|
|
|
|
|
61 |
|
98.4% |
|
|
|
|
|
|
|
||
|
Deep infection |
Var |
3 |
|
2.6% |
|
|
|
|
|
|
|
|
0 |
|
0.0% |
|
|
|
|
|
|
|
0.553X2 |
|
Yok |
113 |
|
97.4% |
|
|
|
|
|
|
|
|
62 |
|
100.0% |
|
|
|
|
|
|
|
||
|
Surgical site |
Sağ |
32 |
|
27.6% |
|
|
|
|
|
|
|
|
15 |
|
24.2% |
|
|
|
|
|
|
|
0.273X2 |
|
Sol |
71 |
61.2% |
44 |
71.0% |
|||||||||||||||||||
|
Bilateral |
13 |
|
11.2% |
|
|
|
|
|
|
|
|
3 |
|
4.8% |
|
|
|
|
|
|
|
||
|
Antibiogram result |
(-) |
110 |
|
94.8% |
|
|
|
|
|
|
|
|
61 |
|
98.4% |
|
|
|
|
|
|
|
0.244X2 |
|
(+) |
6 |
|
5.2% |
|
|
|
|
|
|
|
|
1 |
|
1.6% |
|
|
|
|
|
|
|
||
|
LDH recurrence |
(-) |
108 |
|
93.1% |
|
|
|
|
|
|
|
|
53 |
|
85.5% |
|
|
|
|
|
|
|
0.099X2 |
|
(+) |
8 |
|
6.9% |
|
|
|
|
|
|
|
|
9 |
|
14.5% |
|
|
|
|
|
|
|
||
|
m Mann-whitney U test / X² Chi-square test or Fischer's test exact test. RIF:Rifampicin, SD:Standard deviation, HT hypertension, DM: Diabetes Mellitus, LDH: Lumbar disc herniation. |
|||||||||||||||||||||||
Accumulating evidence suggests that the rate of postoperative spinal infection has decreased after the introduction of prophylactic antibiotics. Nevertheless, it has been observed that this rate has increased again due to the use of the administration of instrumentation in recent years.8
Etiological factors, the clinical condition of the patient, and risk factors should be well examined to ensure the definitive diagnosis and treatment of postoperative infections including superficial and deep SSIs. It should also be recognised that deep SSI is difficult to treat and that postoperative spinal infections can develop within days or weeks and may convert to a chronic condition.5
In patients with SSI, an appropriate antibiotic therapy is initiated based on antibiogram results. However, when no agent is detected in the antibiogram test, broad-spectrum antibiotics should be administered for approximately 6-8 weeks.16 The most important limitation of the present study was its retrospective nature. Another limitation was its small number of patients. However, this study is of high value in terms of inspiring other studies.
CONCLUSION
The utmost care and necessary precautions should be taken to avoid postoperative infections. Intra-operative local antibiotic prophylaxis is the most effective method in preventing postoperative spinal infections. The use of RIF, which is an inexpensive drug with a wide spectrum of action, can be used locally after lumbar discectomy due to its effect in reducing spinal infections.
ETHICAL APPROVAL:
The study was approved by the Institutional Ethics Committee of Van Yuzuncu Yil University (Date: 21.01.2022; No. 2022/01-01).
PATIENTS’ CONSENT:
Informed consent was obtained from all the patients / relatives before the study began.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
EC: Conception, design, data acquisition, critical revision of the manuscript, and supervision.
MY: Data analysis, interpretation, statistical analysis, and manuscript drafting.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: Eliminating the controversies in the diagnosis. Front Med 2014; 1:7. doi: 10.3389/FMED.2014. 00007/FULL.
- Yildizhan S, Boyaci MG. Operation lomber discontinuous vertebral osteomyelite late incident: Case report. Kocatepe Med J 2019; 121-5/July/2018. doi.org/10.18229/koca tepetip. 446871.
- Talu U, Göksan SB, Şar C, Hamzaoglu A, Domaniç U. Early deep postoperative wound posterior instrumentation of the spine and its treatment. Acta Orthop Traumatol Turc 2000; 34:14-22.
- Yaltırık K, Atalay B. Diagnosis/differential diagnosis in specific spinal infections. Diagnostic handbook in spine and spinal cord surgery. Turkish Neurosurg Society Publications, Ankara, 2017: S: 335-43.
- Açıkbaş SC. Postoperative spinal infections. Complication and revision in spine surgery. Turkish Neurosurgery Society Publications, Ankara, 2010: S: 229-35. Turkish.
- Vollmer DG, Nitin Tandon N. Infections of the spine. Youmans neurological surgery. 6 th edt, Elsevier Saunders, New York 2011; pp: 2831-47.
- Suresh AB, Rosani A, Wadhwa R. Rifampin. Encycl Toxicol Third Ed., pp. 134-6, doi: 10.1016/B978-0-12-386454-3. 00781-8.
- Somoskovi A, Parsons LM, Salfinger M. The molecular basis of resistance to isoniazid, rifampin, and pyrazinamide in Mycobacterium tuberculosis. Respir Res 2001; 2(3):164-8. doi: 10.1186/RR54.
- Punjataewakupt A, Napavichayanun S, Aramwit P. The downside of antimicrobial agents for wound healing. Eur J Clin Microbiol Infect Dis 2019; 38(1):39-54. doi.org/10. 1007/s10096-018-3393-5.
- Hoffmann JP, Friedman JK, Wang Y, McLachlan JB, Sammarco MC, Morici LA, et al. In Situ treatment with novel microbiocide inhibits methicillin resistant staphylococcus aureus in a murine wound infection model. Front Microbiol 2019; 10:3106. doi.org/10.3389/fmicb.2019.03106.
- Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005; 30(12):1460-5. doi: 10.1097/01.brs.0000166532.58227.4f.
- Tronnier V, Schneider R, Kunz U, Albert F, Oldenkott P. Postoperative spondylodiscitis: Results of a prospective study about the aetiology of spondylodiscitis after operation for lumbar disc herniation. Acta Neurochir 1992; 117(3-4):149-52. doi: 10.1007/BF01400612.
- Tas A, Karagoz Guzey F, Tufan A, Kuvat N, Aktas OY, Yucel M, et al. Prophylactic effects of silver nanoparticles in a rat model of spinal stabilisation and infection. East J Med 2022; 27(1):126-32. doi: 10.5505/ejm.2022.56254.
- Rohde V, Meyer B, Schaller C, Hassler WE. Spondylodiscitis after lumbar discectomy: Incidence and a proposal for prophylaxis. Spine (Phila Pa 1976) 1998; 23(5):615-620. doi: 10.1097/00007632-199803010-00016.
- Diren F, Onal MB, Can H, AKırcelli A. The rate of spondylodiscitis in patients with lomber discectomy using single dose prophylactic antibiotics. JAREM 2019; 9(Suppl 1): S1-6. doi.org/10.5152/jarem.2018.2333.
- Slowinski S, Lucasti C, Maraschiello M, Kluczynski MA, Kowalski J, Hamill C. Minimally invasive spine surgery as treatment for persistent infectious lumbar spondylodiscitis: A systematic review and meta-analysis. J Spine Surg 2022; 8(1):1-8: doi: 10.21037/JSS-21-50/COIF.