Early Enteral Nutrition Tolerance in a Duodenal Fistula Patient Undergoing Open Abdomen with Vacuum-assisted Temporary Abdominal Closure
By Heng Zhang2, Junfang Zhang1, Zhilong Yang2Affiliations
doi: 10.29271/jcpsp.2022.06.811ABSTRACT
This case sought to manage a duodenal fistula patient who underwent an open abdomen with vacuum-assisted temporary abdominal closure (VAC) by evaluating his tolerance to early enteral nutrition therapy (ENT).
A review of the patient suggested that he developed an abdominal infection as a result of a high duodenal fistula, which necessitated an open abdomen and VAC.
Prior to the initiation of ENT, the patient had a patient-generated subjective global assessment (PG-SGA) score of 8 (1st day) suggesting the need for nutritional intervention. Upon ENT intervention, the patient’s PG-SGA score dropped to 2 (30th day) indicating an improvement in the nutritional status, probably due to measures such as formulation, implementation, and management of early ENT.
The improved nutritional status of the patient led to the success of duodenal fistula repair and abdominal wall defect reconstruction within a short time, thus ensuring a successful surgery.
Key Words: Duodenal fistula, Open abdomen, Enteral nutrition.
INTRODUCTION
As a treatment for severe trauma, abdominal hypertension, and serious abdominal infection, the open abdomen has been extensively used in abdominal surgery in recent years.1 However, an open abdomen can culminate in severe complications such as intestinal air fistula and intra-abdominal hemorrhage. Emerging evidence shows that vacuum-assisted closure (VAC) could significantly improve early fascial closure and reduce the incidence of complications (Figure 1).2,3 Usually, patients with intestinal fistula undergoing open abdomen have a complicated illness, while intestinal fistula with abdominal infection leads to massive loss of nutrients. In this regard, we postulated that early enteral nutrition therapy (ENT) may be used as a treatment option for such diseases. However, bowel edema and bacterial translocation have been suggested to hinder the implementation of ENT (Figure 2).
A patient with duodenal fistula undergoing open abdomen with VAC was admitted to our department in October 2019. Excellent continuous implementation effects of ENT were achieved through the evaluation and management of ENT tolerance.
CASE REPORT
A 69-year male patient was admitted with duodenal fistula and abdominal infection on the 6th day after cholecystectomy+ choledocholithotomy+ T-tube drainage on October 13th 2019. Physical examination on admission revealed body weight: 50 kg, height: 167 cm, body mass index (BMI): 17.9, nutritional risk screening 2002 (NRS 2002) score: 4, patient generated-subjective global assessment (PG-SGA) score: 8, body temperature: 38.5 °C, albumin: 27.6 g/L, prealbumin: 69 g/L, haemoglobin: 87 g/L, white blood cell count: 11.3×109/L, and C-reactive protein: 152.4 mg/L.
Irrigation of the abdominal cavity was performed on the day of admission, and was later changed to double catheterisation cannula irrigation. At the drainage near the duodenal fistula, a large amount of bile was drained. Next, an open abdomen was created on 2nd day of admission, while temporary VAC was applied in the incision dehiscence under costal margin before the negative pressure drainage suite for close trauma was applied to ensure sufficient draining of fluids. The patient was given Peptison at a dose of 500 ml/day and a constant velocity of 20 ml/L through nasointestinal tube on 6th day of admission. On 7th day, the ENT infusion velocity was increased to 20 ml/h in a gradual manner. Pertinently, the dose and velocity of ENT were gradually increased after the patient's tolerance, while a full dose was given on day 9, with a gradual increase in the velocity to 90 ml/h. Physical examination on day 14 after admission showed a body temperature of 37.3°C, albumin of 35.8g/L, prealbumin of 135 g/L, haemoglobin of 120 g/L, white blood cell count of 7.8×109/L, and C-reactive protein of 56 mg/L. Abdominal infection was controlled on 30th day of admission and general nutritional state was improved (nutritional risk score and PG-SGA decreased to 2 and 2, respectively). The body temperature was 36.8°C, albumin: 42.5g/L, prealbumin: 204 g/L, haemoglobin: 148 g/L, white blood cell count: 6.1×109/L, and C-reactive protein: 23 mg/L. Meanwhile, the duodenal fistula repair and abdominal wall defect reconstruction were conducted successfully within a short time. The patient was discharged on 45th day upon recovery.
 Figure 1: Vacuum-assisted closure (VAC).
Figure 1: Vacuum-assisted closure (VAC).
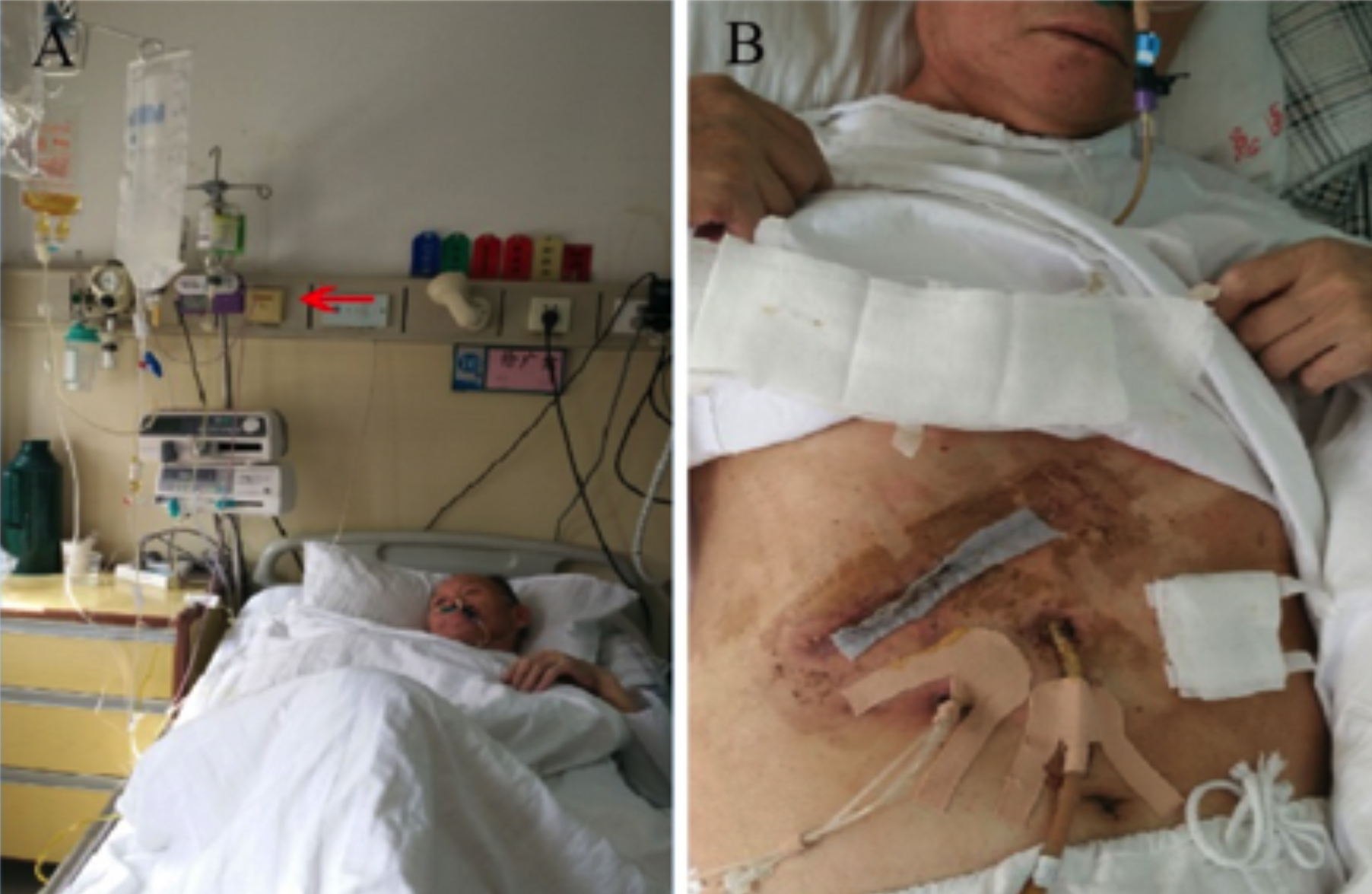 Figure 2: (A) Enteral nutrition therapy (ENT); (B) recovery.
Figure 2: (A) Enteral nutrition therapy (ENT); (B) recovery.
DISCUSSION
The presented patient might have lost a lot of nutrients as a result of intestinal fistula combined with abdominal infection. Meanwhile, increased catabolism and stress state may lead to changes like fluid, electrolyte disturbance, and hypoproteinemia. In this case, infection control is the first step in the management of the patient, while effective nutritional support may be the cornerstone for his recovery.4 Therefore, ENT should be applied as early as possible on the premise that the patient has stable hemodynamics. This could improve the nutritional status of the patient, maintain the barrier function of the intestinal mucosa, and reduce the incidence of gut-derived infection.5 Research shows that early enteral nutrition support can reduce the severity of disease and risk of complications, shorten intensive care unit (ICU) hospitalisation time, and improve the outcome of critically ill patients.6
The patient in this case report had duodenal fistula with abdominal infection, and received VAC with abdominal double-cannula drainage. In line with proper treatment standards of the medical team, evaluation and management scheme of the ENT tolerance was formulated. Also, individualized nutritional support nursing was performed, while nutritional indices were monitored dynamically in order to timely adjust the nutritional support scheme. All the above-mentioned measures resulted in marked improvement in the nutritional status of the patient, which eventually led to the success of the duodenal fistula repair and abdominal wall defect reconstruction within a short time.
FUNDING:
Medical clinical science and technology development fund of Jiangsu University (JLY2021167, JLY20180033).
PATIENT’S CONSENT:
The informed consent is obtained from patients to publish the data concerning this case.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
JZ, ZY: Data acquisition, analysis, design, drafting.HZ: Design, analysis, and final approval.All authors approved the final version of the manuscript to be published.
REFERENCES
- Fitzpatrick ER. Open abdomen in trauma and critical care. Crit Care Nurse 2017; 37(5): 22-45. doi: 10.4037/ccn 2017294.
- Beltzer C, Eisenacher A, Badendieck S, Doll D, Kuper M, Lenz S, et al. Retrospective analysis of a VACM (vacuum-assisted closure and mesh-mediated fascial traction) treatment manual for temporary abdominal wall closure - results of 58 consecutive patients. GMS Interdiscip Plast Reconstr Surg DGPW 2016; 5:Doc19. doi: 10.3205/iprs 000098.
- Bleszynski MS, Chan T, Buczkowski AK. Open abdomen with negative pressure device vs primary abdominal closure for the management of surgical abdominal sepsis: A retrospective review. Am J Surg 2016; 211(5):926-32. doi: 10.1016/j.amjsurg.2016.01.012.
- Babu BI, Finch JG. Current status in the multidisciplinary management of duodenal fistula. Surgeon 2013; 11(3): 158-64. doi: 10.1016/j.surge.2012.12.006.
- Reintam BA, Starkopf J, Alhazzani W, Berger MM, Casaer PM, Deane MA, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med 2017; 43(3):380-98. doi: 10.1007/s00134-016-4665-0.
- Li Q, Zhang Z, Xie B, Ji X, Lu J, Jiang R, et al. Effectiveness of enteral feeding protocol on clinical outcomes in critically ill patients: A before and after study. PLoS One 2017; 12(8):e0182393. doi: 10.1371/journal.pone.