Complementary Feeding Pattern and Nutritional Status of Children
By Ramlah Mehmood, Khadija Nuzhat Humayun, Ali Faisal Saleem, Syeda Asma Sherazi, Nuzhat Asghar AliAffiliations
doi: 10.29271/jcpsp.2023.07.775ABSTRACT
Objective: To determine the complementary feeding patterns and their association with malnutrition.
Study Design: Prospective observational study.
Place and Duration of the Study: Outpatient clinics of Aga Khan University Hospital, Pakistan, from June to November 2019.
Methodology: A total of 207 children from age six to twenty-four months, who presented in the outdoor clinics of the study place, were enrolled. Data were recorded in a predesigned data sheet adopted from the infant and young child feeding module. Chi-square test was applied post-stratification and a p-value of <0.05 was taken as significant.
Results: Among a total of 207 children, 115 (55.6%) were males and 92 (44.4%) were females, with a mean age of 14.15 ± 5.6 months. Complementary feeding was started at an appropriate age in 124 (60%) children. Normal weight was seen in 133 (64.3%) children, while 73 (35.3%) were underweight. Stunting was presented in 44 (21.3%) children, whereas 163 (78.7%) children were of normal length. The most common reason for early initiation of complementary feeding was difficulty in continuing to breastfeed (n=50, 24.2%); the most common reason behind late complementary feeding was bottle feeding (n=45, 21.7%).
Conclusion: Only sixty percent of mothers living in an urban setting started complementary feeding at an appropriate age. Various myths are counteracting complementary feeding practices.
Key Words: Complementary feeding, Infant’s nutrition, Stunting, Wasting, Z-score.
INTRODUCTION
Optimal feeding is crucial for the growth and development of children. The World Health Organization (WHO) advises breastfeeding as an appropriate diet for the first six months, followed by adequate and nutritionally balanced solid food to complement mother feeding.1 Additionally, proper consumption of iron-rich food and a diversified diet with minimum recommended frequency is necessary. While complimentary feeding replaces mother feeding, if the food is inappropriate with low nutrient density, it leads to malnutrition, micronutrient deficiencies and increased episodes of illnesses, especially in children of ages six and twelve months.2,3 A malnourished child is more predisposed to infection which creates a potentially fatal process of worsening illness and deteriorating nutritional status. The number of deaths directly related to severe acute malnutrition ranges from 0.5 to 2 million annually.3,4
Moreover, significant neurodevelopment disabilities in the form of impaired cognitive abilities, delayed motor milestones, and language and communication problems have been reported due to improper feeding. Therefore, well-balanced complimentary feeding, including macro and micronutrients, is fundamental.5,6
The global statistics tell us that in the year 2020, 149.2 million children were stunted and wasting was seen in 45.4 million children under five years.7 According to regional estimates, South Asia has one of the highest burdens of undernutrition i.e., 31.7% stunted and 14.3% wasted.8 According to UNICEF, 36.7% of Pakistani children under five are stunted and only 48% are exclusively breastfed.9 The 2018 National Nutritional Survey reported stunting in 40.2%, wasting in 17.7%, and underweight in 28.9% of Pakistani children.10
In Pakistan, exclusive breastfeeding (48.4%), continued breastfeeding till 2 years (56.5%), and complementary feeding indicators, such as minimum dietary diversity (MDD) (14.2%), minimum meal frequency (MMF) (18.2%), and minimum acceptable diet (MAD) (3.6%), all are far below acceptable levels.10 Multiple factors influence complementary feeding in Pakistan, including maternal education, unavailability of basic health facilities, cultural practices, food folklore, traditional norms, and lack of food diversity, resulting in suboptimal feeding. Islam et al. reported family size, maternal illiteracy, and lack of breastfeeding as risk factors for malnutrition in Pakistani children.11 Similarly, a study from Karachi revealed only 13% of mothers knew the correct timing of complementary feeding, 27·5% of mothers considered <4 months to be optimal, and 57·2% considered 4–6 months.12
The issue of malnutrition is challenging and impedes the goal to reduce morbidity and mortality, particularly in lower-middle-income and resource constraint countries. The majority of the studies conducted in Pakistan primarily focus on rural communities where lack of maternal education is considered a major risk factor for malnutrition. To address the gap in evidence among urban communities, this study was conducted with the aim to assess the complementary feeding practices of mothers in an urban setting to determine the factors contributing to early or late complementary feeding and to determine its impact on the health of children in the same population in the form of wasting, underweight, and stunting so that strategies could be devised to minimize the morbidity in children, especially under five years.
METHODOLOGY
This prospective observational study was carried out in pediatric outpatient clinics of the Aga Khan University Hospital from June till November 30, 2019. The sample size was calculated by keeping the anticipated proportion of late weaning as 16%13 while taking a confidence level of 95% and absolute precision of 0.05, the sample size was 207. The non-probable consecutive sampling technique was used.
The healthy children of either gender from age six months to twenty-four months, who presented to the outpatient clinics of Aga Khan University Hospital Karachi for vaccination or for routine follow-up and whose mothers consented to the study were enrolled. Children whose parents refused to participate in the study or children with chronic diseases (i.e., celiac disease, congenital heart disease, and cystic fibrosis), syndromic diseases, and neurological problems like Cerebral Palsy were excluded from the study.
Early feeding was taken as the initiation of complementary food before six months and late feeding after six months of age. Wasting was defined as per WHO criteria weight for height ≤2 SD; underweight as a weight for age ≤2 standard deviations of the WHO child growth standards median and stunting was defined as height/length for age ≤2 SD of the WHO child growth standards median. Complementary feeding was defined as the procedure of starting and providing other feeds and fluids to the child when breast milk is no longer sufficient to meet the nutritional requirement of infants.14 Complementary food was any solid, semi-solid or soft food, whether manufactured or locally prepared, suitable as a complement to breast milk or infant formula when either becomes insufficient to satisfy the nutritional requirements of the infant.14 Insufficient milk was defined as the perception of the mother of less milk and of child being hungry after feeds. Difficult feeding was defined as issues faced by mother such as sore nipples or increased feeding demand of child, especially in night hours. Formula milk was defined as initiation of complementary food due to cost of formula milk. Working mother was defined as discontinuation of breastfeeding due to job/ employment. Interest in other foods was defined as subjective feeling of mother that baby is taking food items more easily than milk. Child growth was defined as mother’s feeling that her baby is not gaining proper weight with milk only and needs other food items early. Lack of knowledge was defined as uneducated mothers or with primary education having no knowledge about the correct timing of complementary feeding. Food myths was defined as subjective feeling of mother that baby cannot chew and digest food, certain foods are hot or cold for the baby and baby falls ill by certain food items. Pregnancy interval was defined as the age difference between two siblings. Bottle feeding was defined as using bottle for feeding children and subjective feeling of mother that baby is taking enough calories from bottle feeding. Family size was defined as number of households. Advice of family member was defined as pressure/restrictions faced by the mother from other family members or relatives in terms of timing of complementary feeding. Poverty was defined as having less resources to buy extra food items for the baby and take care of her/his needs.
The data were collected after taking approval from the Ethical Review Committee of Aga Khan Hospital (ERC No. 1170) and the Research Evaluation Unit of the College of Physicians and Surgeons of Pakistan. All the children aged six to twenty-four months, meeting the inclusion criteria were registered on a structured data collection sheet adopted from infant and young child feeding questionnaire. The questionnaire was also translated into Urdu. Verbal and written consent was obtained. The primary researcher filled out the datasheet. The study participants were assigned a unique identification number to maintain confidentiality. Children were weighed wearing one layer of clothing (extra clothing was removed). The length was taken by putting the infantometer on a flat surface and placing the infant barefoot and head in a recumbent position. These values were then plotted on standard WHO growth charts.
The data were analysed by using Statistical Package for Social Sciences version 23. The mean and standard deviation were calculated for the patient’s age, weight, and length. Frequency and percentages were calculated for gender, age at initiation of complementary feeding, early or late feeding and frequency of underweight, wasting, and stunting. The effect of modifiers like age, gender, number of siblings, maternal education, and marital status were controlled through stratification. The Chi-square test was applied post-stratification by taking a p-value <0.05 as significant.
RESULTS
Out of 207 children, 115 (55.6%) were males and 92 (44.4%) females. The mean age of participants was 14.15 ± 5.6 months, mean weight was 9.08 ±2.03 kg, and mean length was 76.24 ± 7.22 cm, respectively. Among the malnutrition parameters, underweight and stunting were observed in 35.3% and 21.3% of children respectively, whereas 64.3% of children were of normal weight and 78.7% were of normal length. Complementary feeding was started at an appropriate age in 60% of children; 19% received complementary feeding at less than six months, while 21.2% of children after six months. The demographic parameters of study participants are presented in Table I.
When complementary feeding age was compared with underweight in children, underweight was more common in children who started feeding after six months of age, with a p-value of 0.01. Similarly, complementary feeding age was significantly associated with stunting in children, with a p-value of <0.001, Table II.
When the gender of children was compared to underweight and stunting. Underweight and stunting were both common in boys but the results were not statistically significant (Table III).
The most common cause for early feeding was difficulty in continuing to mother feed, which was seen in 50 (24.2%) children, whereas the most common reason behind late feeding was bottle feeding which was present in 45 (21.7%) children (Figures 1 and 2, respectively). Birth weight was not statistically significant with malnutrition.
Table I: Demographic parameters of study participants (n=207).
|
Age Mean ± SD |
14.15±5.6 months |
|
Weight Mean ± SD |
9.08 ± 2.03 kg |
|
Length Mean ± SD |
76.24 ± 7.22 cm |
|
Male |
115 (55.6%) |
|
Female |
92 (44.4%) |
|
Weaning at six months |
124 (60%) |
|
Weaning <6 months |
39 (19%) |
|
Weaning >6 months |
44 (21%) |
|
Underweight |
73 (35.3%) |
|
Stunting |
44 (21.3%) |
Table II: Association of weaning and malnutrition.
|
Age of weaning |
Underweight |
p-value |
Stunting |
p-value |
|
<6 months |
28.2% |
0.014 |
7.7% |
0.002 |
|
Six months |
31.4% |
18.5% |
||
|
>6 months |
52.2% |
40.9% |
Table III: Association of gender with malnutrition in children.
|
Gender |
Underweight |
p-value |
Stunting |
p-value |
|
Male |
43% |
0.013 |
23.4% |
0.399 |
|
Female |
26% |
18.5% |
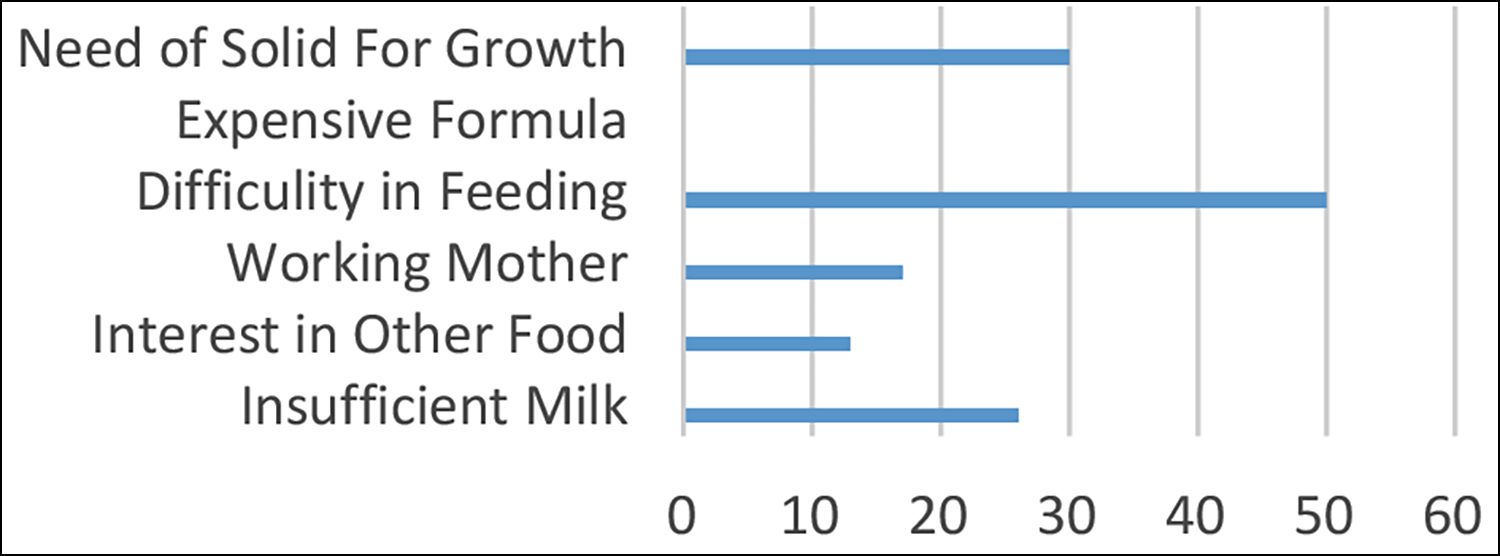 Figure 1: Reasons for early weaning.
Figure 1: Reasons for early weaning.
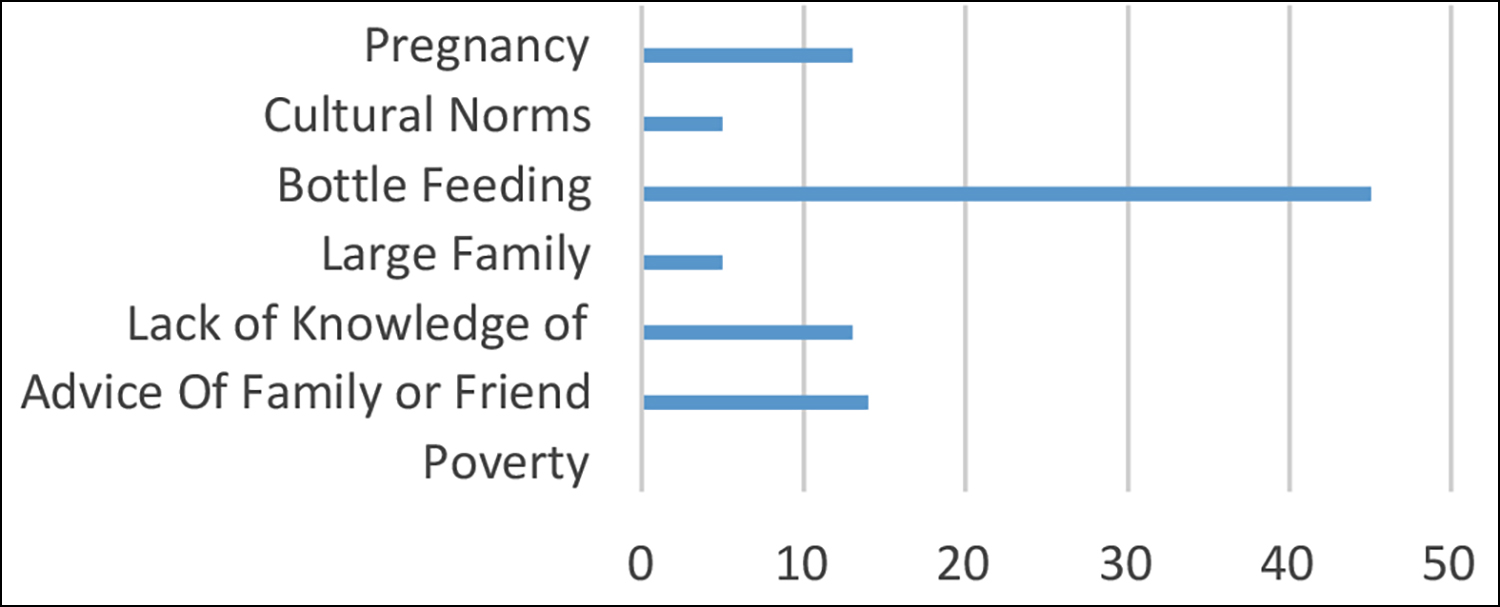 Figure 2: Reasons for late weaning.
Figure 2: Reasons for late weaning.
DISCUSSION
Malnutrition is a threatening condition. It increases the case fatality of common childhood infections, thus increasing infant and childhood mortality rates. Feeding practices in infancy profoundly affect health in later years and thus contribute to malnutrition. The understanding and practices of complementary feeding depend on multiple facets and vary in different cultures and regions.
In this study, 60% of children received complementary feeding at six months. In a study done in the residential colony of Lahore, 44% of children received complementary feeding at less than six months, 38% at six months, and 16% after six months.13 Manzoor et al. carried out a study in a peri-urban area in Lahore and found that 42% of infants were weaned at the age of five to six months whereas 32% after the period of six months.15
Malnutrition was observed in our study in the form of underweight and stunting, though acute malnutrition in the form of wasting was not seen. This shows the high vulnerability of children in similar geographical and social regions to both acute and chronic conditions of malnutrition. Parallel results were observed in the community-based nutritional survey done in rural areas of district Malir, which demonstrated 52.36% underweight children, 36.49% stunted and 20.61% wasted. Of these children, 17.55% had weaning at an inappropriate age, i.e., before four months or after six months.16
The most common reason for early feeding in our study was difficulty in feeding, seen in 24.2% children. Maternal perception of inadequate feeding as a reason for the early start of complementary feeding has been reported in different studies.15,17,18 In a focused group discussion conducted on mothers having children between six months to two years of age in slum areas of Lahore, common causes for early initiation of complementary feeding were insufficient milk, need of food for the development of the baby, elders in the house suggested the time to begin semi-solids and subsequent pregnancy. Mothers mainly opposed delayed weaning and knew this could hamper the child’s growth. The baby did not like the taste of food, the incapability of the child to eat everyday homemade foods, and the difficulty of cooking separately for the baby were some other reasons.13
Early introduction of food and bottle feeding exposes the child to the risks of infections whereas the impacts of late weaning include faltered growth and compromised nutritional status. Proper weaning time needs to be followed to assure the good health of the younger children. Early or delayed weaning is a problem that must be embarked on wisely.18
Besides that, maternal knowledge about different components like quality, quantity, and frequency is crucial to address in decreasing malnutrition. Lack of familiarity with complementary foods can result in a deficiency of nutrients directed to impoverished infants.19 There is a massive gap between the knowledge and practice of mothers in weaning their babies. Exploration of perceptions will help design effective interventions for improving complementary feeding practices as appropriate timing carries a substantial impact.
CONCLUSION
The present study indicated inappropriate complementary feeding practices in mothers living in an urban setting, contributing to malnutrition in children. Moreover, various myths in the population are counteracting infant feeding practices.
DISCLOSURE:
It is a dissertation-based article written as a part of FCPS II training.
ETHICAL APPROVAL:
Ethical Review Committee of the Aga Khan Hospital (ERC No. 1170) and Research Evaluation Unit of the College of Physicians and Surgeons of Pakistan.
PATIENTS’ CONSENT:
Informed written consent was taken from parents/guardians to publish the data.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
RM: Contribution to the concept, design, and analysis of data.
KNH: Contribution to the analysis of important intellectual content.
AFS: Contributing to the concept, design, and final revision of the work.
SAS: Contribution to data interpretation and analysis.
NAA: Contribution to the literature search and data entry.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- World Health Organization. Indicators for assessing infant and young child feeding practices part 3: Country profiles. World Health Organization; 2010.
- Fewtrell M, Bronsky J, Campoy C, Domellöf M, Embleton N, Mis NF, et al. Complementary feeding: A position paper by the European society for paediatric gastroenterology, hepatology, and nutrition (ESPGHAN) committee on nutrition. J Pediatric Gastroenterol Nutr 2017; 64(1): 119-32. doi: 10.1097/MPG.0000000000001454.
- WHO. Essential nutrition actions: Improving maternal, newborn, infant and young child health and nutrition. World Health Organization; 2013.
- Uauy R, Desjeux JF, Ahmed T, Hossain M, Brewster D, Forbes D, et al. Global efforts to address severe acute malnutrition. J Pediatr Gastroenterol Nutr 2012; 55(5): 476–81. doi: 10.1097/MPG.0b013e318272af06.
- Aemro M, Mesele M, Birhanu Z, Atenafu A. Dietary diversity and meal frequency practices among infant and young children aged 6–23 months in Ethiopia: A secondary analysis of Ethiopian demographic and health survey 2011. J Nutr Metab 2013; 2013. doi: 10.1155/2013/782931.
- Nyaradi A, Li J, Foster JK, Hickling S, Jacques A, O'Sullivan TA, Oddy WH. Good‐quality diet in the early years may have a positive effect on academic achievement. Acta Paediatr 2016; 105(5):e209-18. doi: 10.1111/apa.13324.
- World Health Organization. Levels and trends in child malnutrition: Key findings of the 2021 edition. World Health Organization; 2021.
- United Nations Children’s Fund, World Health Organization, The World Bank. UNICEF-WHO-World Bank joint child malnutrition estimates. New York; Geneva; Washington, DC: UNICEF; WHO; The World Bank; 2020.
- UNICEF. Key demographic indicators–Pakistan. UNICEF Data: Monitoring the situation of children and women. data. unicef. org/country/pak. 2018.
- NIPS NI of PS, ICF. Pakistan Demographic and Health Survey 2017–18. NIPS and ICF; 2018.
- Nisar MU, Anwar-ul-Haq MM, Tariq S, Anwar M, Khawar A, Waqas A, Nisar A. Feeding patterns and predictors of malnutrition in infants from poor socioeconomic areas in Pakistan: A cross-sectional survey. Cureus 2016; 8(1):452. doi: 10.7759/cureus.452.
- Mohsin SS, Shaikh AS, Shaikh R, Haider N, Parkash A. Knowledge attitude and practices of mothers regarding complementary feeding. J Dow Uni Health Sci 2014; 8(1): 21-5.
- Salim S, Kalsoom S, Humayun A. Weaning practices and perceptions of mothers residing in urban slums of Lahore, Pakistan: A focus group design. Ann King Edward Med Uni 2016; 22(4).
- World Health Organization. Complementary feeding: report of the global consultation, and summary of guiding principles for complementary feeding of the breastfed child.
- Manzoor I, Bukhari A, Daud S, Munir MK, Hashmi NR, Shaharyar S, et al. Weaning. Prof Med J 2009; 16(02): 27984.
- Shamim S, Naz F, Jamalvi SW, Ali SS. Effect of weaning period on nutritional status of children. J Coll Physicians Surg Pak 2006; 16(8):529-31.
- Marandi A, Afzali HM, Hossaini AF. The reasons for early weaning among mothers in Teheran. Bulletin World Health Organization 1993; 71(5):561. PMC2393482.
- Kulsoom U, Saeed A. Breast feeding practices and beliefs about weaning among mothers of infants aged 0 – 12 months. J Pak Med Assoc 1997; 47(2).
- Liaqat P, Rizvi MA, Qayyum A, Ahmed H, Ishtiaq N. Maternal education and complementary feeding. Pakistan J Nutrition 2006; 5(6):563-8. PMID: 9071862.