Comparison of the Effectiveness of Shock Index, Modified Shock Index, and Age Shock Index in COPD Exacerbations
By Salih Kocaoglu1, Adnan Karadas2Affiliations
doi: 10.29271/jcpsp.2022.09.1187ABSTRACT
Objective: To evaluate the effectiveness and practicality of shock index (SI), modified shock index (MSI), and age-shock index (Age-SI) in predicting the prognosis, mortality, ICU and service admission, and the need for intermittent mandatory ventilation (IMV) and nasal intermittent mandatory ventilation) (NIMV in the ED patients with chronic obstructive pulmonary disease (COPD) exacerbation.
Study Design: Retrospective study.
Place and Duration of Study: Balikesir University Faculty of Medicine, Emergency Service, Balıkesir, Turkey, from January 2019 to May 2020.
Methodology: Adult patients, who were admitted to the Emergency Department with diagnosis of COPD exacerbation, were included. Patients with missing data were excluded. SI, MSI, and age-SI values were calculated by using the vital signs. ROC curve analysis was used to evaluate the diagnostic performances of SI, MSI, and age-SI.
Results: The study consisted of 201 patients, 152 (75.6%) were males. Six (3%) patients died, 26 (12%) were admitted to ICU, 112 (55.7%) were admitted to the service, 11 (5.5%) needed IMV, and 48 (23.9%) needed NIMV in ED. SI was superior to the MSI and age-SI in predicting mortality, and AUC values of 0.802, 0.727, and 0.704, respectively. SI was also superior to the MSI and age-SI in predicting hospital admissions (SI AUC=0.591, p=0.029; MSI AUC=0.572, p=0.059; and age-SI AUC=0.580, p=0.089).
Conclusion: Respectively none of the three indices was independently sufficient in predicting IMV, NIMV, and the need for ICU. SI is a valuable parameter in discriminating the COPD exacerbation. It is superior to the MSI and age-SI in predicting mortality and hospital admissions. It will be useful to evaluate SI for the severity classification, follow-up, and management of the patients with COPD.
Key Words: Age shock index, Chronic obstructive pulmonary disease, Modified shock index, mortality, Shock index.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a common preventable disorder accompanied by the persistent airflow restriction resulting from alterations in the airways and alveoli after exposure to the harmful particles or gases and associated respiratory complaints.1 COPD is an important public health problem that ranks fourth among the causes of death in the world, has high mortality and morbidity, seriously reduces the comfort of patients’ life and has a serious financial burden on the health systems of the countries.2 The guidelines published by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Committee are used in this disease, which often exacerbates and can cause hospitalisation.
However, today, the decision of hospitalisation and discharge is still made in the emergency department based on the experience of the clinician.3-5 A simpler and more memorable method that enables early detection of risky patients is necessary for the clinicians.
The shock index is calculated by dividing heart rate by systolic blood pressure (SBP). It has a normal range of 0.5 to 0.7 reported in the previous studies.6 The MSI is calculated by pulse rate/MAP and also allows diastolic blood pressure (DBP) to be assessed compared to the traditional SI. The age-SI is calculated by multiplying the patient's age with the SI. SI is used for the prognosis in patients with acute bleeding, hypovolemia, sepsis, myocardial infarction, decompensated heart failure, gastrointestinal bleeding, and pneumonia.7-10 These indices can be calculated practically and quickly in patients with COPD exacerbation presenting to the ED and may be useful in predicting critical patients. These indices can help emergency department physicians in diagnosis, treatment, and hospitalisation planning.
Shock index has previously been used for risk classification in various critical diseases, and its higher values have been found as an independent predictor of the mortality, microvascular damage, and myocardial damage.11,12 However, there is no study in the literature on the use of the index in patients with COPD. The aim of this study was to evaluate the effectiveness of shock index (SI), modified shock index (MSI), and age-shock index (age-SI) derived from the shock index in the discrimination of critically ill patients presented to the emergency department with COPD exacerbations.
Table I: Laboratory findings of the patients.
|
Variables |
Descriptive statistics |
|
Fever* (°C) |
37(35.30-40.00) |
|
Respiratory rate* (min) |
28(3-40) |
|
SBP* (mmHg) |
140(70-225) |
|
DBP* (mmHg) |
80(50-600) |
|
MAP* (mmHg) |
100(56.67-433.33) |
|
Saturation* (%) |
85(50-100) |
|
WBC* (103/µL) |
11(2-40) |
|
Neutrophils* (%) |
77.50(6.00-97.00) |
|
Na* (mmol/L) |
137(115-155) |
|
Cl* (mmol/L) |
100(9-114) |
|
Urea* (mg/dL) |
37(14-190) |
|
Creatinine* (mg/dL) |
0.95(0.39-9.38) |
|
CRP* (mg/L) |
7.70(0.10-193) |
|
pCO2* (mmHg) |
52.10 (19-100) |
|
pH# |
7.37±0.09 |
|
pO2* (mmHg) |
57(18-194) |
|
HCO3* (mmol/L) |
26.80(2.00-49.50) |
|
Lactate* (mmol/L) |
1.40(0.30-10.10) |
|
pSO2* (%) |
86(42-99) |
|
Pulse rate# (beats/min) |
105.92±23.42 |
|
Hb# (g/dL) |
12.73±2.04 |
|
Htc# (%) |
39.64±6.13 |
|
K# (mmol/L) |
4.45±0.63 |
|
MAP: Mean arterial pressure. Data given as * median (minimum-maximum) or #mean±standard deviation.
|
|
METHODOLOGY
This study consisted of 201 patients, who presented to Balıkesir University Faculty of Medicine Emergency Service with complaints of dyspnea, between January 2019- May 2020, were found to have a COPD exacerbation as a result of the examination performed by the relevant clinician and were over the age of 18 years. The study was approved retrospectively by the Clinical Research Ethics Committee (issue: 2020/192). The data were obtained from the records of the hospital archives. Files of 587 patients, whose ‘dyspnea’ ICD code had been entered, were examined. Of these, 279 patients had been diagnosed with COPD (201 patients had COPD exacerbation) were included in the study. Patients, whose files could not be accessed or whose information was incomplete, were excluded from the study.
SBP, DBP, and pulse data were recorded from the patient files, which were recorded in ED triage. Based on these data, SI (pulse rate / SBP), MSI (pulse rate / MAP), and age-SI (age x SI) scores were calculated. In addition, patients' additional illnesses, medication usage, number of emergency service admissions in the last year, the status of smoking, vital signs, symptoms, physical examination findings, postero-anterior chest radiographs, and laboratory findings were recorded. Afterwards, patients who needed in-hospital mortality, admission to the intensive care unit (ICU), hospitalisation, need for invasive mechanical ventilation (IMV), and non-invasive mechanical ventilation (NIMV) in the emergency room were determined and the results were recorded. The primary outcome was the in-hospital mortality of the patients. The secondary outcomes were the need for admission in the ICU, the need for admission to the service, and NIMV or IMV administration in the ED.
Shapiro-Wilk test was used to test the normality of variables. Mean±standard deviation or median (minimum-maximum) values were presented for the variables which were normally distributed and not normally distributed, respectively. Categorical variables were expressed by counts and percentages. Receiver operating characteristics (ROC) curve analysis was performed to evaluate and compare the performances of diagnostic markers. The significance level was taken as α = 0.05. Statistical analyses were performed on IBM SPSS Statistics version 22.0 (IBM Corp., USA) and MedCalc 12.3.0.0.
RESULTS
There were 49 women (24.4%) and 152 men (75.6%) with a median age of 72 (47-89) years. ICU admission and mortality rates were 12.90% (n=26) and 3.00% (n=6), respectively. The median mMRC dyspnea scale value was 5.00 (1.00-5.00). There were 46 non-smokers (22.9%), 124 ex-smokers (61.70%), and 31 active smokers (15.40%). Outcome was; Discharged from ED: 66 (32.80), Non-invasive treatment: 48 (23.90), Invasive treatment: 11 (5.50), Hospitalisation in the normal service: 112 (55.70), ICU admission: 26 (12.90), In-hospital mortality: 6 (3.00).
The laboratory values used and examination findings are shown in Table I. ROC curve analyses were performed to evaluate the diagnostic performances of SI, age-SI, and MSI to predict in-hospital mortality, admission to intensive care unit, hospitalisation, need for IMV in the emergency department, and need for NIMV in the emergency department.
Table II: Laboratory findings of the patients.
|
|
AUC |
p-value |
cut-off value |
Sensitivity |
Specificity |
PPV |
NPV |
|
|
Non-invasive mechanical ventilation |
SI |
0.515 |
0.743 |
≤0.84 |
75.00 |
36.60 |
27.10 |
82.40 |
|
Age SI |
0.573 |
0.106 |
≤60.50 |
81.25 |
39.22 |
29.50 |
87 |
|
|
MSI |
0.538 |
0.418 |
≤1.05 |
66.67 |
51.63 |
30.20 |
83.20 |
|
|
Invasive mechanical ventilation |
SI |
0.561 |
0.505 |
>0.90 |
45.45 |
76.84 |
10.20 |
96.10 |
|
Age SI |
0.552 |
0.499 |
>49.92 |
90.91 |
45.26 |
8.80 |
98.9 |
|
|
MSI |
0.595 |
0.224 |
>0.91 |
90.91 |
32.63 |
7.20 |
98.40 |
|
|
Hospitalisation |
SI |
0.591 |
0.029 |
>0.58 |
91.96 |
29.21 |
62 |
74.30 |
|
Age SI |
0.580 |
0.059 |
>41.46 |
93.75 |
31.46 |
63.30 |
80 |
|
|
MSI |
0.572 |
0.089 |
>0.76 |
96.43 |
21.35 |
60.70 |
82.60 |
|
|
ICU admission |
SI |
0.535 |
0.560 |
>0.9 |
34.62 |
77.14 |
18.40 |
88.80 |
|
Age SI |
0.514 |
0.807 |
≤47.92 |
23.08 |
62.86 |
8.50 |
84.60 |
|
|
MSI |
0.548 |
0.393 |
>0.88 |
88.46 |
28.57 |
15.50 |
94.30 |
|
|
Mortality |
SI |
0.802 |
<0.001 |
>0.79 |
100 |
62.56 |
7.60 |
100 (97.0 – 100.0) |
|
Age SI |
0.704 |
0.008 |
>53.50 |
100 |
54.36 |
6.30 |
100 (96.5 – 100.0) |
|
|
MSI |
0.727 |
0.004 |
>0.99 |
100 |
43.59 |
5.20 |
100 (95.8 – 100.0) |
|
|
ICU: Intensive care unit, AUC: Area under the ROC curve, PPV: Positive predictive value, NPV: Negative predictive value, SI: Shock index, MSI: Modified shock index. |
||||||||
Significant diagnostic performances were obtained for all three indices in predicting in-hospital mortality. The AUC value for SI was found to be the highest (AUC=0.802, p<0.001). The threshold values for SI, age-SI and MSI are 0.79, 53.50 and 0.99, respectively. AUC values of the three indices were compared to predict in-hospital mortality. The performance of SI was significantly higher than age-SI (p=0.036) and MSI (p=0.039). However, there is no significant difference between age-SI and MSI (p=0.702) performances in predicting in-hospital mortality (Table II, Figure I).
SI showed significant performance in predicting hospitalisation (AUC=0.591, p=0.029), but the other two indices were not statistically significant. The three indices were not good at predicting ICU admission, the need for IMV in ED, and the need for NIMV in ED (Table II, Figure I).
DISCUSSION
SI is an important index that shows the general well-being of the patient. Previous studies showed that SI was closely related to patient prognosis. Significant relationships have been found between increased SI and mortality in diseases, such as heart failure, gastrointestinal bleeding, pneumonia, sepsis, and myocardial infarction.7-10 However, there are no studies in the literature on SI, and MSI and age-SI in COPD exacerbations. Although recommendations on the prevention, diagnosis, and management of COPD are published in the GOLD guidelines, the evaluation of COPD exacerbations with appropriate objective data is still a controversial issue. The decision of hospitalisation is generally made by the physician subjectively and varies among clinics.
In the present, it was found that SI was an important parameter in predicting in-hospital mortality in patients admitted to the emergency department with COPD exacerbation. In the ROC analysis, the AUC value of SI was 0.802 for mortality (p <0.001). For cut-off value at 0.79, its sensitivity was 100% and specificity was 62%. In addition, SI was a good predictor of hospitalization of patients with COPD (AUC = 0.591, p = 0.029). The most important decision in the management of COPD is to predict mortality and to decide on hospitalisation in a high-risk patient.1 The CRSI-65 score, which includes SI, can be a useful and practical test tool in the ED without laboratory testing to predict mortality, and thus can accelerate the initiation of treatment.13 SI, can provide a practical approach for outpatient management in ED triage, pre-hospital, and primary care. It can reduce the rate of referral of patients with COPD exacerbations from primary care hospitals.
In this study, the relationship between patient outcomes and MSI and age-SI, along with SI, was examined. MSI is an important predictor of mortality in patients presenting to the ED.14 Unlike complex scoring systems, age-SI is thought to be used in patients with GIS bleeding because it can be easily calculated and is superior to SI and MSI in critically ill patients in the ED.15 It was observed that MSI and age-SI gave significant results for in-hospital mortality. The AUC values of MSI and age-SI were 0.727 and 0.704, respectively (MSI-p = 0.004, age-SI-p = 0.008). However, we think that SI is the ideal parameter for predicting mortality because it shows the best performance among the three indices and can be calculated more easily. MSI and age-SI were not as significant as SI for predicting hospitalisation (MSI-p = 0.089, age SI-p = 0.059). None of the three indices was good at determining the need for NIMV in the emergency department, the need for IMV in the ED, and the patient in need of ICU (Table II).
This study was single-centred and designed retrospectively. Information was obtained from patient files and the hospital database. Therefore, these results need to be supported by larger, multicenter prospective studies.
CONCLUSION
SI is a valuable parameter in discriminating critical patients among those who present to the emergency department with COPD exacerbation. It can be used in the evaluation of patients with COPD exacerbation because it is superior to MSI and age-SI and is an easily calculated parameter. SI can be included in new scoring systems to be developed.
ETHICAL APPROVAL:
Ethics committee approval was obtained from Balikesir University Clinical Ethics on 21.10.2020 with permission numbered 2020/192.
PATIENTS’ CONSENT:
The study is a retrospective study. For this reason, patient consent is not available.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SK: Proposed the study.
AK: Wrote the paper.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- The global ınitiative for chronic obstructive lung diseases (Gold). Global strategy for diagnosis, management and prevention of COPD. 2020 report, 2020. goldcopd.org/gold-reports/. (Citation Date: 01 05 2021).
- Raherison C, Girodet PO. Epidemiology of COPD. Eur Respir Rev 2009; 18(114):213-21. doi: 10.1183/09059180.0000 3609.
- Echevarria C, Steer J, Heslop-Marshall K, Stenton S.C, Hickey P.M, Hughes R, et al. The pearl score predicts 90-day readmission or death after hospitalisation for acute exacerbation of COPD. Thorax 2017; 72(8):686-93. doı: 10.1136/thoraxjnl-2016- 209298.
- Ertan Yazar E. Acute exacerbation of COPD. Güncel Göğüs Hastaliklari Serisi 2018; 6(2):44-9. doi: 10.5152/gghs. 2018.016.
- Mohan A, Chandra S, Agarwal D, Guleria R, Broor S, Gaur B, et al. Prevalence of viral infection detected by PCR and RT-PCR in patients with acute exacerbation of COPD: A systematic review. Respirology 2010; 15:536-42. DOI: 10.1111/j. 1440-1843.2010.01722.x
- Otero R, Nguyen B. Soktaki hastaya yaklasim. In: Judith Tintinalli Eds. [cev.] Cem Ertan Acil tip Kapsamli Bir Calısma klavuzu. ed.7th, Istanbul; Nobel Tip Kitapevi; 2013: p.65-172.
- Sankaran P, Kamath AV, Tariq SM, Ruffell H, Smith AC, Prentice P, et al. Are shock index and adjusted shock index useful in predicting mortality and length of stay in community-acquired pneumonia? Eur J Intern Med 2011; 22(3): 282-5. doı: 10.1016/j.ejim.2010.12.009.
- Semerci E, Durukan P, Yıldırım S, Baykan N, Yakar S, Ipekten F. Gastrointestinal sistem kanamali hastalarda sok indeksi ve hematokrit duzeylerinin mortalite uzerine etkisi. Akademik Gastroenteroloji Dergisi 2018; 17(2):85-9. doi.org/10.17941/agd.440452.
- Cakır E, Bindal A, Ozciftci Yılmaz P, Dogu C, Ozkoçak Turan I. Sepsisli hastaların hemodinamik destek ihtiyaci. harran üniversitesi tıp fakültesi dergisi 2020; 17(2);172-6. doi.org/10.35440/hutfd.722382.
- Cetinkaya HB, Gunes H. Use of shock ındex and lactate to predict mortality in acute heart failure patients in emergency department. J Coll Physicians Surg Pak 2021; 31(3):262-6. doı: 10.29271/jcpsp.2021.03.262.
- El-Menyar A, Goyal P, Tilley E, Latifi R. The clinical utility of shock index to predict the need for blood transfusion and outcomes in trauma. J Surg Res 2018; 227:52-59. doı: 10.1016/j.jss.2018.02.013.
- Ozsu S, Erbay M, Durmuş ZG, Ozlu T. Classification of high-risk with cardiac troponin and shock index in normotensive patients with pulmonary embolism. J Thromb Thrombolysis 2017; 43(2):179-183. doı: 10.1007/s11239-016-1443-3.
- Beliz Tekten O, Temrel TA, Sahin S. Confusion, respiratory rate, shock index (CRSI-65) score in the emergency department triage may be a new severity scoring method for community-acquired pneumonia. Saudi Medical J 2020; 41(5):473-8. doi:10.15537/smj.2020.5.25069.
- Liu YC, Liu JH, Fang ZA, Shan GL, Xu J, Qi ZW, et al. Modified shock index and mortality rate of emergency patients. World J Emerg Med 2012; 3(2):114-7. doi:10.5847/wjem. j.issn. 1920-8642.2012.02.006.
- Kocaoglu S, Cetinkaya HB. Use of age shock index in determining severity of illness in patients presenting to the emergency department with gastrointestinal bleeding. Am J Emergency Med 2021; 47:274-8. doi.org/10.1016/j.ajem.2021.05. 008.
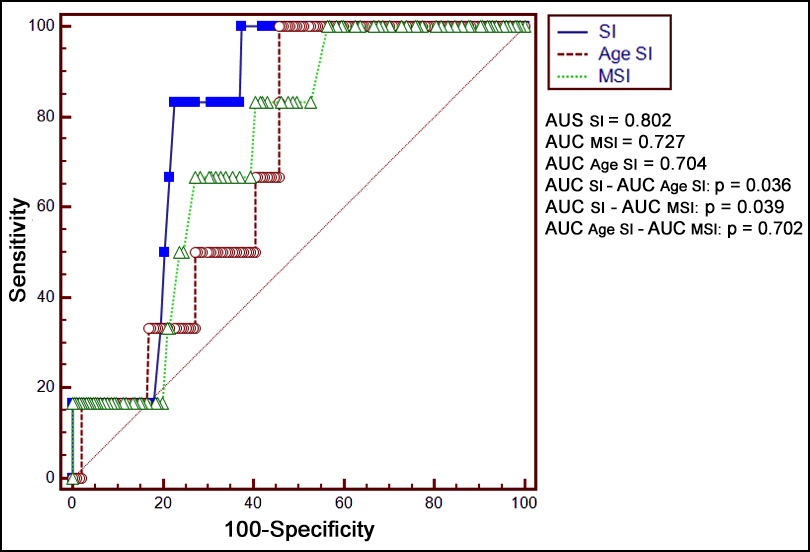 Figure I: AUC values for the scoring indices, the SI, age SI and the MSI in predicting in-hospital mortality (SI: shock index, MSI: modified shock index).
Figure I: AUC values for the scoring indices, the SI, age SI and the MSI in predicting in-hospital mortality (SI: shock index, MSI: modified shock index).