Comparison of the Conventional PNL with Ecirs in the Treatment of Complete Staghorn Kidney Stones
By Hasan Nedim Goksel Goktug, Ufuk Ozturk, Sertac Cimen, Serafettin Kaymak, Ahmet Emin Dogan, Muhammet Abdurrahim ImamogluAffiliations
doi: 10.29271/jcpsp.2023.03.346ABSTRACT
Objective: To analyse the results of conventional percutaneous nephrolithotomy (PNL) and endoscopic combined intrarenal surgery (ECIRS) in treating complete staghorn kidney calculi.
Study Design: A comparative study.
Place and Duration of the Study: Department of Urology, University of Health Sciences, Diskapi Yildirim Beyazit Training and Research Hospital, Ankara, Turkey, between January 2007 and January 2022.
Methodology: Clinical data and surgical outcomes of the adult patients who underwent conventional PNL or ECIRS were retrospectively reviewed. Two patient groups were compared regarding the fluoroscopy time, the number of access, surgical time, duration of hospitalisation, haemoglobin (Hb) reduction, complication, and stone-free rates.
Results: There were 132 renal units in the conventional PNL (Group 1) and 45 renal units in the ECIRS group (Group 2). The comparative analysis revealed that fluoroscopy time, surgical time, duration of hospital stay, number of access, and the Hb drop were significantly lower in the ECIRS group compared to the conventional PNL group. Although stone-free rates were 48.5% in Group 1 and 64.4% in Group 2, p=0.064 and p>0.05 respectively). The median value of the complication grade was 1 (1-7) in Group 1 and 1 (1-5) in Group 2, (U=2446.5, p=0.026).
Conclusion: The ECIRS is a successful and more secure surgical method for treating complete staghorn stones than PNL.
Key Words: PNL, ECIRS, Staghorn, Kidney, Stone.
INTRODUCTION
Complete staghorn stones can lead to loin pain, progressive renal dysfunction, obstructive uropathy, pyelonephritis, or urosepsis.1 Therefore, total stone clearance is essential in managing patients with complete staghorn stones to eradicate the focus of infection, relieve obstruction, prevent a future recurrence, and preserve renal function.2
Percutaneous nephrolithotomy (PNL) is the mainstay surgical method for treating complete staghorn stones. However, since all calyces may not be accessible, multiple access may be required, leading to increased morbidity. Endoscopic combined intrarenal surgery (ECIRS) is a procedure which was initially introduced in 2008, enabling the simultaneous use of combined retrograde and antegrade approaches for large or complex kidney stones using rigid and flexible endoscopes.3
In addition, this approach can decrease the requirement for another percutaneous access since a rigid nephroscope can reach stone fragments in the ureter and the renal calyces. Despite the theoretical advantages of ECIRS over PNL in the treatment of staghorn stones, there are no sufficient evidence-based comparative data. Herein, the aim of the study was to compare the results of conventional PNL with those of ECIRS in cases with complete staghorn stones.
METHODOLOGY
After obtaining approval from the Ethical Review Council of the University of Health Sciences, Diskapi Training and Research Hospital (133/6-21.03.2022), the data of the adult (i.e., age >18 years) patients treated for staghorn stones at the centre between January 2007 and January 2022 were retrospectively reviewed. Patients who had unilateral or bilateral complete staghorn stones were included. Pregnant women, paediatric patients, patients with partial staghorn stones, and those with congenital and urogenital malformations were excluded. Patients who underwent flexible ureterorenoscopy (FURS), extracorporeal shock wave lithotripsy (ESWL), or PNL to treat the same stone before enrollment in this study were omitted.
Conventional PNL was performed to treat patients with complete staghorn stones at the study centre from January 2007 to June 2019, while ECIRS was performed from June 2019 to January 2022. Therefore, patients who underwent conventional PNL were allotted to Group 1, and those who underwent ECIRS were allocated to Group 2. Both study groups were compared concerning all collected data parameters.
Medical data, including gender, age, body mass index (BMI), laterality status (unilateral vs. bilateral), laboratory results such as urinalysis, preoperative and postoperative complete blood count and renal function test results, and coagulation tests, were retrieved from the electronic patient folders. All patients had a negative preoperative urine culture since those with positive results were all given appropriate antibiotics until the urine culture turned negative.
Preoperative kidney-ureter-bladder X-ray (KUB) and non-contrast abdominal computerised tomography (NCCT) were performed during the preoperative evaluation of all patients. The NCCT images were used for measuring the stone burden and density. The stone burden (i.e., total stone area) was calculated as square millimetres using the formula length x width x π x 1/4 (Figure 1).4
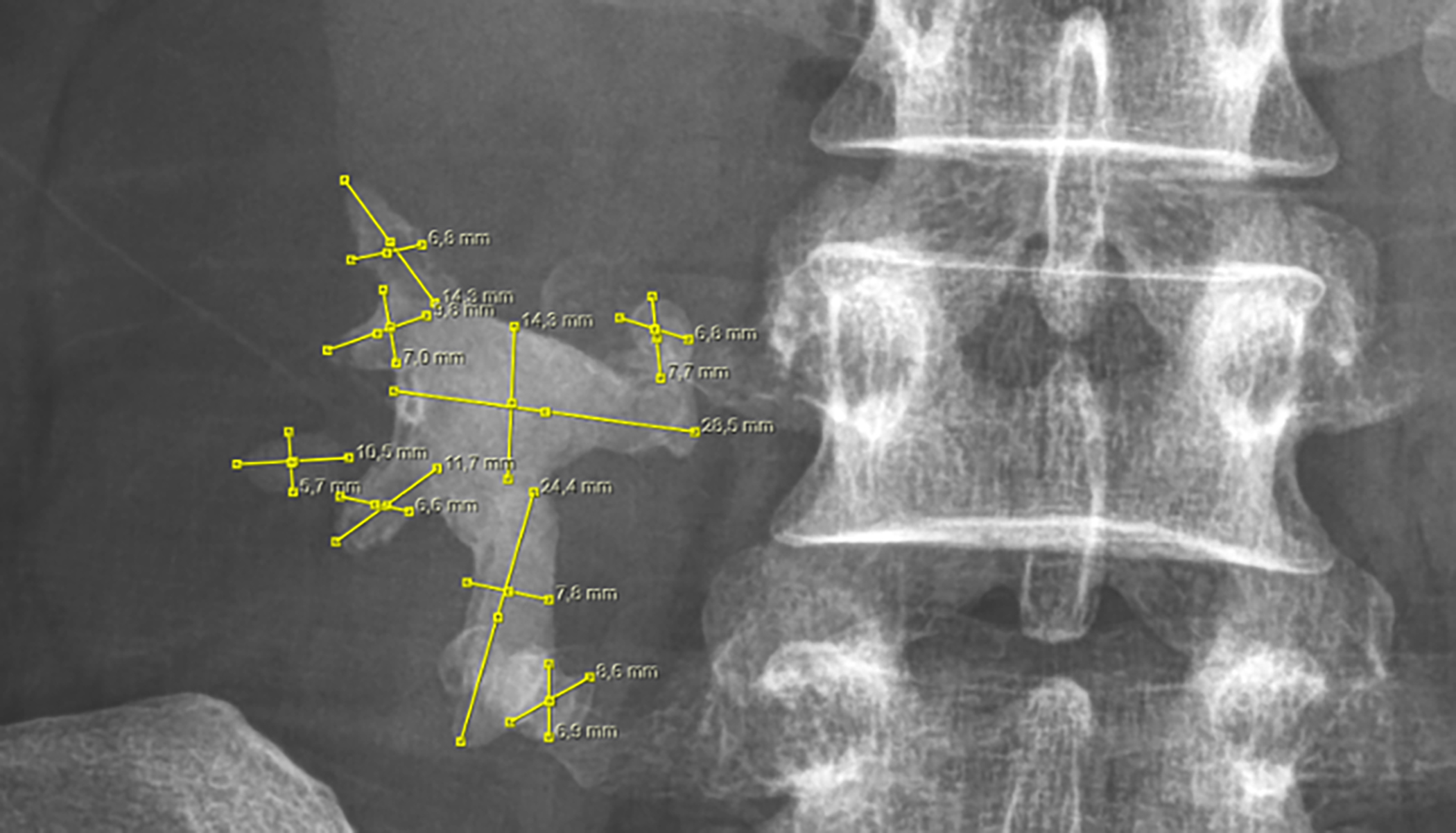 Figure 1: Piecemeal measurement of a complete staghorn kidney stone.
Figure 1: Piecemeal measurement of a complete staghorn kidney stone.
Data, including the duration of hospitalisation and surgery, were also retrieved from the patient folders. The latter was recorded as the number of minutes. The database also included PNL access numbers, fluoroscopy time, data regarding stone-free status, and complications categorised as per the Clavien–Dindo classification.
For Group 1, a 6F ureteral catheter was placed in the ureter using a rigid cystoscope in the lithotomy position. After the patient was placed in the prone position, the lower calyx was first targeted to reach the stone and access was achieved with an 18-gauge diamond-tipped needle. Subsequently, a guidewire was introduced to the ureter. The needle was pulled out, and the skin and fascia were incised. Then, a nephrostomy tract was established under fluoroscopic imaging using the Amplatz plastic dilators. Finally, a 30F working sheath and a 27F nephroscope were used to perform the surgery. The stones were fragmented by a pneumatic lithotripter. Stone fragments were extracted using grasping forceps. New access tracts were opened using the same method for stones that the rigid nephroscope could not reach.
In Group 2, patients were given Galdakao Modified Supine Valdivia Position (GMSVP), allowing antegrade and retrograde access (Figure 2).
 Figure 2: Galdakao Modified Supine Valdivia Position for endoscopic combined intrarenal surgery.
Figure 2: Galdakao Modified Supine Valdivia Position for endoscopic combined intrarenal surgery.
Under general anaesthesia, a 9,5–11.5F access sheath was introduced. Then, a conventional flexible ureterorenoscopy (FURS) procedure was performed by a 7.5F flexible ureteroscope. Next, the stone fragmentation was performed by a 4–12W Holmium laser using 200 or 365 μm laser fibres at 5–10 Hz. and 800–1200 mj intervals. Mainly, ureteropelvic and pelvic stones were targeted during the FURS stage of the procedure. If necessary, the fragments were taken out by a 1.9F basket catheter. Next, calyx stones were targeted to provide visually assisted percutaneous needle insertion described by Kidd et al.5 A guidewire was advanced through an 18G diamond-tipped needle into the pelvis and, if possible, the ureter. Subsequently, the percutaneous nephrostomy tract was formed using plastic Amplatz dilators. A 30F working sheath and a 27F nephroscope were employed to perform the procedure. Next, a pneumatic lithotripter was utilised for stone fragmentation, and the fragments were extracted by grasping forceps. Finally, stones that the rigid nephroscope could not reach were removed by the FURS, which was performed simultaneously. After the stone fragmentation and fragment removal procedure, a 14F re-entry nephrostomy tube was placed into the PNL access tract. The operative time was defined as the time elapsing between starting cystoscopy and inserting a 14F re-entry nephrostomy tube.
In both Group 1 and Group 2, ensuring complete stone-free status was the main criteria for ending the procedure. However, bleeding impairing vision of the operative field was also the reason for ending the procedure in some cases.
All patients were checked for residual stones on the first postoperative day with KUB and ultrasonography. Patients without residual stones or those with residual stones smaller than 4 mm during the assessment two weeks after surgery were considered stone-free, while other cases were defined as treatment failure and underwent additional treatments.
The success rate was calculated based on the number of stone-free cases that did not require another procedure, and the failure rate was calculated based on the cases requiring additional treatment.
Table I: Comparison of the study groups regarding demographic data, stone characteristics and surgical data.
|
Variables |
Group 1(PNL) |
Group 2 (ECIRS) |
p-value |
|
Number of patients |
132 |
45 |
|
|
Gender (female/male) |
72/60 (45.5%/54.5%) |
27/18(40%/60%) |
0.524c |
|
Age (years) |
56 (28-78) |
57(44-78) |
0.034 |
|
Body mass index (kg/m2) |
24.5 (17-35) |
27 (19-35) |
0.052 |
|
Side (right/left) |
80/52 (60.6%/39.4%) |
24/21(53.3%/46.7%) |
0.392c |
|
Stone size (mm2) |
915 (100-1600) |
900 (780-1500) |
0.465 |
|
Hounsfield unit (HU) |
990 (680-1350) |
990 (800-1300) |
0.996 |
|
Multiple access rates |
29.5% (39/132) |
0.0 % (0/45) |
<0.001ᶠ |
|
Fluoroscopy time (minutes) |
16 (11-24) |
12 (8-15) |
<0.001 |
|
Hb drop (gr/dl) |
2.4 (1.9-3.5) |
1.6 (1-3) |
<0.001 |
|
Surgical time (minutes) |
90 (65-120) |
70 (58-110) |
<0.001 |
|
Duration of hospital stay (days) |
2 (2-4) |
2 (1-3) |
<0.001 |
|
Stone-free rates |
48.5% (64/132) |
64.4% (29/45) |
0.064c |
|
Complication grades |
1 (1-7) |
1 (1-5) |
<0.026 |
|
Mann-Whitney U-test was used in the analysis of all data except for c and ᶠ. Chi-square test was used for ͨ and Fisher’s Exact test was used for ᶠ. PNL: Percutaneous nephrolithotomy, ECIRS: endoscopic combined intrarenal surgery, Hb: Haemoglobin. |
|||
Table II: Comparison of complication grades as per Clavien-Dindo classification.
|
|
Total (n=177) |
Group 1 (n=132) |
Group 2 (n=45) |
p-value |
Odds ratio |
Confidence interval |
|
Grade 1 |
8(4.52%) |
7(5.3%) |
1(2.2%) |
0.681 ˃0.1 |
2.464 |
0.295-20.595 |
|
Grade 2 |
23(13.0%) |
19(14.4%) |
4(8.9%) |
0.343 ˃0.1c |
1.723 |
0.55-5.367 |
|
Grade 3a |
4(2.26%) |
4(3.0%) |
0(0%) |
0.573 ˃0.1 |
NA |
NA |
|
Grade 3b |
8(4.52%) |
7(5.3%) |
1(2.2%) |
0.681 ˃0.1 |
2.464 |
0.295-20.595 |
|
Grade 4a |
4(2.26%) |
4(3.0%) |
0(0%) |
0.573 ˃0.1 |
NA |
NA |
|
Grade 4b |
4(2.26%) |
3(2.3%) |
1(2.2%) |
1.0 ˃0.99 |
1.023 |
0.104-10.093 |
|
Grade 5 |
0(0%) |
0(0%) |
0(0%) |
NA |
NA |
NA |
|
|
51(28.8%) |
44(33.3%) |
7(15.5) |
|
|
|
|
Fisher’s exact test was used in all data analyses except for c, Chi-square test was used for c. |
||||||
The data were analysed using the SPSS 24.002 program. The conformity of quantitative variables to normal distribution was evaluated by the Kolmogorov-Smirnov test. Since the variables did not fit the normal distribution, the Mann-Whitney U-test was used in the data analysis. The data were given as medians and ranges, including minimums and maximums. The chi-square and Fisher’s Exact tests were used in the qualitative data analyses, and variables were expressed as counts and percentages. The p-value was regarded as significant when it was lower than 0.05.
RESULTS
This analysis revealed that 17350 patients were diagnosed with kidney stones throughout the study period. Among these patients, 650 had staghorn stones. Complete staghorn stones were present in 165 of these patients. Twelve of these patients had bilateral complete staghorn kidney stones. Thus 165 patients with 177 renal units with complete staghorn stones were assigned to this study.
There were 132 renal units in Group 1 (i.e., PNL group) and 45 renal units in Group 2 (i.e., ECIRS group). The median BMI was 24.5 (17-35) in Group 1 and 27 (19-35) in Group 2 (U=2396, p=0.052). While the median HU was 990 (680-1350) in Group 1, it was 990 (800-1300) in Group 2, and the difference was not statistically significant (U=2968.5, p=0.996). The median total stone area (TSA) was significantly higher in Group 1 than in Group 2; while the median TSA was 915 [100-1600] in Group 1, it was 900 [780-1500] in Group 2 (U=2753, p=0.465) (Table I).
The comparative analysis also revealed that the two groups were similar regarding stone-free rates (48.5% in Group 1 vs.. 64.4% in Group 2, p=0.064). On the other hand, a comparison concerning multiple access rates elucidated that this figure was significantly higher in Group 1 than in Group 2 (29.5% vs. 0%, p<0.05). Also, there was a significant difference between both groups regarding median fluoroscopy times; while the median fluoroscopy time was 16 [11-24] in Group 1, it was 12 (8-15) in Group 2 (U=270, p=0.000). As such, the median surgical time was significantly higher in Group 1 compared to Group 2 (90 [65-120] vs. 70 [58-110], U=1610.5, p<0.001).
The two groups were also compared concerning the decrease in haemoglobin (Hb) levels (i.e., postoperative Hb-preoperative Hb). This analysis revealed that the median Hb decrease was 2.4 [1.9-3.5] in Group 1 and 1.6 [1.0-3.0] in Group 2. The two groups were also significantly different in this regard (U=881, p<0.001).
The median duration of hospitalisation was two days in both Group 1 [2-4] and Group 2 [1-3]; nevertheless, the difference was statistically significant (U=2059, p<0.001, Table I).
For complication analysis regarding Clavien-Dindo classification, complications were scaled from `no complication` to Grade 5 complications between 1 and 8. The median value was 1 (1-7) for Group 1 and 1 (1-5) in Group 2. The difference between the two groups was statistically significant (U=2446.5, p=0.026). However, there was no statistically significant difference between the two groups concerning complication rates when a one-by-one comparison was performed for Clavien-Dindo grade 1, 2, 3a, 3b, 4a, 4b, and 5 complications using the chi-square test, odds ratios, and confidence intervals. The most common complications were Grade 2 in both groups (Table II).
DISCUSSION
Urinary system stone disease is a significant health problem.6 Its frequency is affected by factors such as age, race, and gender and varies between 1% to 20%, depending on the geographical region.
A kidney stone filling the renal pelvis and a calyx group is called a partial staghorn stone, while one occupying the entire collecting system is defined as a complete staghorn stone disease. Complete staghorn stones can cause progressive renal deterioration, obstruction, and urosepsis.1 Therefore, total stone clearance is crucial for saving renal function, relieving obstruction, and eliminating the source of infection.2
The European Association of Urology (EAU) guidelines recommended PNL as the gold standard for treating renal stones larger than 2 cm.7 In addition, both EAU and American Association of Urology (AUA) guidelines suggest PNL as the first line treatment method for treating staghorn stones.7,8
There are several published studies regarding the effective use of the PNL method in treating staghorn kidney stones.9,10 For example, El-Nahas et al. performed PNL in 251 renal units and achieved a stone-free rate of 73% in the third postoperative month.9 However, these authors noted a complication rate of 27% in the study. In another study, Soucy et al. performed 509 PNL procedures and reported a stone-free rate of 78%.10 However, they noted that a second-look nephroscopy was needed in 45 patients to remove the residual stone fragments. It is also widely accepted that conventional PNL has some limitations in treating staghorn stones.11,12 One of these limitations is the technical challenge of reaching the stones with a rigid nephroscope and removing the stone fragments migrated to the ureter.11 Another limitation is the possible need for multiple percutaneous access.12 It is widely accepted that multiple access is associated with a higher risk of morbidity, including adjacent organ injuries, thoracic complications, and haemorrhagic events. In addition, it may prolong surgical time, fluoroscopy time, duration of hospital stay, and increase treatment costs.12
In a study analysing the data of the multi-tract (i.e., multiple access) PNL procedures performed on 164 renal units, the authors stated that they achieved a 70% stone-free rate13. However, they also reported complications, including bleeding requiring blood transfusion (n=46), urosepsis (n=8), thoracic injury (n=8), renal pseudoaneurysm (n=4), and perinephric collection (n=1).13 In another study, Aron et al. performed PNL in 121 units and achieved an 84% stone-free rate.14 Nevertheless, they reported that 18 patients had bleeding requiring blood transfusion, while three developed hydrothorax, two had renal pseudoaneurysms, and one had urosepsis. They also noted that 22 patients had a postoperative fever.
Considering the limitations of the conventional PNL, efforts have been made to strengthen this method to increase the stone-free rates and lower the complication rates.15-17 The introduction of the PNL-anterograde FURS combination is the result of these efforts. In this procedure, stones that the rigid nephroscope could not reach during PNL or the stone fragments migrating to the ureter can be reached via antegrade FURS and fragmented by laser lithotripsy. Therefore, stone-free rates and the need for additional interventions can be reduced.15 A study comparing conventional PNL with PNL-anterograde FURS reported that the stone-free rates could be increased from 80.9% to 86.9% on the postoperative first day and from 87.6% to 95% at the end of the third month after surgery by this approach.15 Furthermore, a randomised prospective study comparing PNL with and without simultaneous flexible nephroscopy demonstrated that the stone-free rate was higher (92.5% vs. 70%) in the former group.16
Another method developed to improve the outcomes of conventional PNL is endoscopic combined intrarenal surgery (ECIRS).17 In this approach, FURS is simultaneously used during PNL to treat large and complicated kidney stones. Moreover, it can be performed in both supine and prone positions. The Galdakao Modified Supine Valdivia Position (GMSVP) was preferred for ECIRS procedures in the present study.
Zhong et al. compared ECIRS with standard PNL in the prone position for treating staghorn calculi.18 They reported a significantly higher stone-free rate (91% vs. 65%, p=0.038), a significantly shorter surgical time (110 vs. 129 min, p<0.001), and a significantly lower Hb drop (2.1 g/L vs. 3.5 g/L, p<0.001) in favour of ECIRS. However, in this study, the stone-free rates were analysed at the end of the first month after surgery, and some patients underwent additional treatments before this analysis. Furthermore, all patients did not have complete staghorn stones. On the other hand, all patients had complete staghorn stones in this present cohort, and the stone-free rates were analysed on the first postoperative day. Thus, a bias was prevented.
Staged FURS is another approach for treating staghorn stones or stones larger than 2 cm.19 However, this approach is preferred only in patients with anatomical obstacles, history of anticoagulant use, morbid obesity, or pregnancy for whom PNL is contraindicated. Karakoyunlu et al. compared staged FURS to PNL in cases with renal pelvis stones larger than 2 cm.19 Although they did not find a significant difference in stone-free rates, they reported that PNL had an advantage over staged FURS due to the necessity of multiple treatments and more extended treatment time associated with staged FURS. On the other hand, it was reported that single or staged FURS could be effective and safe in patients with renal stones between 2 and 4 cm, and the stone-free rate was mainly impacted by stone location and size.20 Of note, these studies did not include patients with complete staghorn stones.
The present study compared the conventional PNL to ECIRS in treating complete staghorn stones and determined that ECIRS was superior concerning fluoroscopy time, surgical time, duration of hospitalisation, and Hb decrease. It is comprehended that a relatively shorter fluoroscopy time implies less radiation exposure. The surgical time is affected by the position of the patient, the stone burden, the efficiency of the energy sources, and the surgeon's experience. The length of hospital stay is one of the most important determiners of treatment costs and the return to work and social life. The findings of the present study indicated that ECIRS was beneficial regarding these parameters.
In the present cohort, the stone-free rate was slightly higher in the ECIRS group; however, no statistically significant difference was detected. This finding can be ascribed to the excessive stone load in both groups, and that stone-free rates were analysed two weeks after surgery. In addition, the Hb reduction was more significant in the standard PNL group than in the ECIRS group, probably due to the higher multiple access requirements.
Zeng et al. used single-tract (18F) minimally invasive PNL to avoid multi-tract PNL in 102 patients with staghorn stones.21 These researchers performed semi-rigid or flexible nephroscopy through the same tract during the same session and performed RIRS in 56 patients with residual stones. Finally, 89% of these cases were stone-free. In addition, they reported that the complication rate was 10.7% after PNL. It is important to note that a second procedure and the mean duration of hospital stay was 9 days. The fact that the stone-free rate was higher in this study than in the present study is probably due to the inclusion of partial staghorn stones and additional procedures. In the present study, the complication rate was 33.3% in the PNL group and 15.5% in the ECIRS group. Considering the surgical times and complication rates, it can be suggested that using a 30F Amplatz working sheath facilitates the procedure but increases the complication risk.
Wen et al. compared single-session mini-PNL with single-session ECIRS to treat partial staghorn stones.22 They denoted that the stone-free rate and surgical time were higher in the latter group than in the former group. In the present study, the stone-free rate was higher in the ECIRS group than in the conventional PNL group; however, the difference was not statistically significant. Furthermore, contrary to Wen et al.'s study, the surgical times and complication rates were lower in the ECIRS group compared to the PNL group in the present cohort.22 Since the present study worked on complete staghorn stones, surgical times and complication rates were higher in the conventional PNL group, probably due to a higher rate of multiple access.
To the authors’ knowledge, this study is the first to compare the outcomes of conventional PNL with ECIRS in patients with complete staghorn kidney stones. However, it has some limitations that must be considered while evaluating its findings. First, it has a retrospective design. Second, the analysis did not include the need for additional interventions and long-term outcomes. Therefore, it can be suggested that prospective, randomised studies with relatively larger sample sizes, including these data, will be valuable to the literature.
CONCLUSION
ECIRS is a practical and secure surgical method for treating complete staghorn stones.
ETHICAL APPROVAL:
The study was conducted after obtaining approval from the Ethical Review Council of the University of Health Sciences, Diskapi Training and Research Hospital (133/6-21.03.2022).
PATIENTS’ CONSENT:
Informed consent was obtained from the patients to publish the data concerning this study.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
HNGG, AED: Designed and drafted the manuscript.
SK, SC: Collected the data.
UO, MAI: Involved in the analysis of the data.
UO, AED, SC, SK, MAI: Contributed significantly in writing and critical revision of the manuscript
All the authors have read and approved the final version of the manuscript to be published.
REFERENCES
- Nemoy NJ, Stamey TA. Surgical, bacteriological, and biochemical management of "infection Stones." JAMA 1971; 215:1470-6.
- Ganpule AP, Naveen Kumar Reddy M, Sudharsan SB, Shah SB, Sabnis RB, Desai MR. Multitract percutaneous nephrolithotomy in staghorn calculus. Asian J Urol 2020; 7(2):94-101. doi: 10.1016/j.ajur.2019.10.001.
- Scoffone CM, Cracco CM, Cossu M, Grande S, Poggio M, Scarpa RM. Endoscopic combined intrarenal surgery in Galdakao-modified supine Valdivia position: A new standard for percutaneous nephrolithotomy? Eur Urol 2008; 54(6):1393-403. doi: 10.1016/j.eururo.2008.07.073.
- Tiselius HG, Andersson A. Stone burden in an average Swedish population of stone formers requiring active stone removal: How can the stone size be estimated in the clinical routine? Eur Urol 2003; 43(3):275-81. doi: 10.1016/s0302- 2838(03)00006-x.
- Kidd CF, Conlin MJ. Ureteroscopically assisted percutaneousrenal access. Urology 2003; 61(6):1244-5. doi: 10.1016/ s0090-4295(03)00006-2.
- Medina-Escobedo M, Sánchez-Pozos K, Gutiérrez-Solis AL, Avila-Nava A, González-Rocha L, Lugo R. Recurrence of nephrolithiasis and surgical events are associated with chronic kidney disease in adult patients. Medicina (Kaunas) 2022; 58(3):420. doi: 10.3390/medicina58030420.
- Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. European Urology 2016; 69(3):475-82. doi: 10.1016/ j.eururo.2015.07.041.
- Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: American urological association/endourological society guideline, PART I. J Urol 2016; 196(4):1153-60. doi: 10.1016/j.juro. 2016.05.090.
- El-Nahas AR, Eraky I, Shokeir AA, Shoma AM, El-Assmy AM, El-Tabey, et al. Factors affecting stone-free rate and complications of percutaneous nephrolithotomy for treatment of staghorn stone. Urology 2012; 79(6):1236-41. doi: 10.1016/ j.urology.2012.01.026.
- Soucy F, Ko R, Duvdevani M, Nott L, Denstedt JD, Razvi H. Percutaneous nephrolithotomy for staghorn calculi: A single center's experience over 15 years. J Endourol 2009; 23(10):1669-73. doi: 10.1089/end.2009.1534.
- Cracco CM, Knoll T, Liatsikos EN, Osther PJ, Smith AD, Scarpa RM, et al. Rigid-only versus combined rigid and flexible percutaneous nephrolithotomy: A systematic review. Minerva Urol Nefrol 2017; 69(4):330-41. doi: 10.23736/S0393-2249.17.02841-7.
- Ruhayel Y, Tepeler A, Dabestani S, MacLennan S, Petřík A, Sarica K, et al. Tract sizes in miniaturised percutaneous nephrolithotomy: A systematic review from the European association of urology urolithiasis guidelines panel. Eur Urol 2017; 72(2): 220-35. doi: 10.1016/j.eururo.2017.01.046.
- Singla M, Srivastava A, Kapoor R, Gupta N, Ansari MS, Dubey D, et al. Aggressive approach to staghorn calculi—safety and efficacy of multiple tracts percutaneous nephrolithotomy. Urology 2008; 71(6):1039-42. doi: 10. 1016/j.urology.2007.11.072.
- Aron M, Yadav R, Goel R, Kolla SB, Gautam G, Hemal AK, et al. Multi-tract percutaneous nephrolithotomy for large complete staghorn calculi. Urol Int 2005; 75(4):327-32. doi: 10.1159/000089168.
- Goktug G, Karakoyunlu N, Sener NC, Zengin K, Nalbant I, Karabacak O, et al. Standard percutaneous nephrolithotomy alone versus in combination with intraoperative anterograde flexible nephroscopy for staghorn stones: A retrospective study. Kaohsiung J Medical Sciences 2015; 31(11): 568-71. doi: 10.1016/j.kjms.2015.08.004.
- Gucuk A, Kemahlı E, Uyeturk U, Tuygun C, Yıldız M, Metin A. Routine flexible nephroscopy for percutaneous nephrolithotomy for renal stones with low density: A prospective, randomised study. J Urology 2013; 190(1):144-8. doi: 10.1016/j.juro.2013.01.009.
- Turk C, Neisius A, Petrik A, Seitz C, Skolarikos A, Thomas K, et al. EAU guidelines on urolithiasis. uroweb.org/guidelines/urolithiasis/chapter/guidelines.
- Zhong W, Zhao Z, Wang L, Swami S, Zeng G. Percutaneous-based management of Staghorn calculi in solitary kidney: Combined mini percutaneous nephrolithotomy versus retrograde intrarenal surgery. Urol Int 2015; 94(1): 70-3. doi: 10.1159/000360708.
- Karakoyunlu N, Goktug G, Sener NC, Zengin K, Nalbant I, Ozturk U, et al. A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: A prospective randomised study. Urolithiasis 2015; 43(3): 283-7. doi: 10.1007/s00240-015-0768-2.
- Huang JS, Xie J, Huang XJ, Yuan Q, Jiang HT, Xiao KF. Flexible ureteroscopy and laser lithotripsy for renal stones 2 cm or greater: A single institutional experience. Medicine (Baltimore) 2020; 99(43):e22704. doi: 10.1097/MD.000000000 0022704.
- Zeng G, Zhao Z, Wu W, Zhong Wen. Combination of debulking single-tract percutaneous nephrolithotomy followed by retrograde intrarenal surgery for staghorn stones in solitary kidneys. Scandinavian J Urology 2014; 48(3):295-300. doi: 10.3109/21681805.2013.852621.
- Wen J, Xu G, Du C, Wang B. Minimally invasive percutaneous nephrolithotomy versus endoscopic combined intrarenal surgery with flexible ureteroscope for partial staghorn calculi: A randomised controlled trial. International J Surgery 2016, 28:22-7. doi: 10.1016/j.ijsu.2016.02.056.