Comparison of the Analgesic Efficacy of Lidocaine Spray versus Tramadol and Fentanyl for Pain Control in Rib Fractures
By Ahmet Burak Erdem1, Safa Donmez1, Alp Sener2Affiliations
doi: 10.29271/jcpsp.2023.05.491ABSTRACT
Objective: To compare the analgesic efficacy of lidocaine spray with tramadol hydrochloride and fentanyl citrate in rib fractures.
Study Design: A randomised, controlled open-label study.
Place and Duration of the Study: Ministry of Health Ankara City Hospital, Turkiye, from June to November 2021.
Methodology: Patients over the age of 18 years, who applied to the Emergency Department with blunt chest trauma, were divided into three groups. Groups were created from patients who were given lidocaine 10% spray (local), i.v. 100 mg of tramadol, and i.v. fentanyl 50 mcg. A total of 48 patients, each of whom was 16, were included in the study. Numerical rating scale (NRS) pain scores of the patients at baseline, 15th, 30th and 60th minutes were compared. These scores and the number of falls at follow-up were analysed comparatively between the 3 groups.
Results: The age and gender distribution of the patients included in the study were found to be statistically similar between the groups. Although the degrees of decrease in NRS scores in the 0-15, 0-30, and 0-60 minute periods were higher in the tramadol group, these differences were not statistically significant (p=0.465/ 0.256/ 0.678, respectively). While no side effects were observed in the lidocaine group, there were 4 (25.0%) patients in the fentanyl group and 2 (12.5%) patients in the tramadol group.
Conclusion: Lidocaine spray can be used safely in the management of acute pain in rib fractures, as it has fewer side effects and is as effective as opiates.
Key Words: Analgesia, Fentanyl, Lidocaine spray, Pain, Rib fracture, Tramadol.
INTRODUCTION
Trauma is frequently encountered in emergency departments and requires a multidisciplinary approach. Blunt chest trauma is seen in a significant proportion of these patients. The most important symptom is pain and the cause is mostly a rib fracture. Rib fractures can be seen in more than half of the patients with thoracic trauma.1,2 Pain management can reduce various causes of morbidity and mortality that can occur with pulmonary complications due to rib fractures. Atelectasis, pneumonia, and hypoxemia may develop in the lungs due to reasons such as difficulty in breathing due to pain, inability to cough, and sputum discharge.3,4
Pain management in rib fractures draws a profile ranging from simple painkillers to local treatments such as kinesio tape, lidocaine patch, opiate use, and even nerve blocks.4,5 Opiates are primarily preferred in the treatment of pain in thoracic traumas. Since they are lipophilic agents, they easily cross the brain barrier. It has been shown to reduce complications related to rib fractures by acting on central and peripheral opiate receptors.6 Fentanyl is frequently preferred because of its analgesic and anaesthetic properties, especially in the treatment of cancer, trauma, and post-surgical pain treatment, because it is more potent than morphine and can be used at lower doses. It has important side effects such as nausea, vomiting, hypotension, respiratory depression, and addiction. Since it is eliminated from the liver, it can be used in renal dysfunction.7 Tramadol, on the other hand, is an atypical opiate analgesic with less respiratory depression and less addictive effects, unlike conventional opiates. It exerts its effect mostly by inhibiting the reuptake of noradrenaline and serotonin from the presynaptic terminals. It is known that it has fewer side effects than classical opiates because it has less opiate receptor effects.8
Lidocaine patches have also been used in the pain treatment of rib fractures, and results have been as successful as the analgesia control provided by opiates.5,9 Lidocaine sprays, on the other hand, is a local anaesthetic drug that is mostly used in procedures performed on mucosal surfaces. It shows the effect between 1-15 minutes. It reduces hyperalgesia by stabilising the neuronal membrane. Sodium channel blockade provides analgesia by modulating G protein-coupled receptors, calcium and potassium channels, and N-methyl-D-aspartate receptors. Lidocaine spray has many dermal applications such as chest tube removal, surgery for nasal bone fractures, and intravenous vascular access. It controlled pain well in all of these applications.10-12 However, in the literature review, there is no study on the use of lidocaine spray in the treatment of acute pain in patients with rib fractures.
The rationale of this study was to investigate whether lidocaine spray can be used to control acute pain in rib fractures and also whether it can be an alternative agent to opiate class agents such as tramadol and fentanyl in multimodal analgesia. The study aimed to compare the analgesic efficacy of lidocaine spray with tramadol hydrochloride and fentanyl citrate in rib fractures.
METHODOLOGY
This study was planned as a prospective, randomised controlled and open-label study. It was approved by the Ministry of Health Ankara City Hospital Ethics Committee (E1-21-1678) and conducted between June and November 2021 in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients. Patients who were conscious, oriented, and cooperative, who had blunt thoracic trauma, who had a computerised thoracic tomography, who had a rib fracture in their tomography, and whose pain score was 5 or higher on the numerical rating scale (NRS), were randomly distributed to the groups and included in the study. Patients who refused to participate in the study, with a detected or suspected pregnancy, with a known history of allergy or other adverse reaction to the agents used in the study, with a history of sedative agent use or drug addiction, and with analgesic use within six hours of admission to the emergency department, who needed emergency tube thoracostomy or surgical intervention, were hemodynamically unstable, and had open and/or infected wounds in the fracture area were excluded from the study.
Three groups were designed for the study. Group A received lidocaine 10% spray, Group B received tramadol hydrochloride 100 milligrams intravenously, and Group C received 50 microgram fentanyl citrate intravenously.
For this study, sample size analysis was performed using the data of the study of Ingalls et al.5 with lidocaine patch. According to this analysis, it was calculated that at least 16 cases should be included in each group with 80% power and 5% type-1 error. In total, 48 patients were included in the study, 16 patients for each group.
The patient who met the inclusion criteria in the study was randomly assigned to the treatment groups by the emergency department doctor. After the patient's consent was obtained, the treatment protocol was initiated by the doctor. Before starting the treatment (0th minute), the patient marked the NRS pain score on the form and blood pressure, pulse, respiratory rate, fever, and oxygen saturation were measured. For group A, 10% lidocaine spray was applied on the broken rib from a distance of 10 cm, 1-2 puffs. Each puff contains 10 mg of lidocaine. For group B, 100 mg of tramadol hydrochloride was placed in 150 cc isotonic saline and given as a 15-minute intravenous infusion. For Group C, 50 mcg of fentanyl citrate was given as a 15-minute intravenous infusion in 150 cc isotonic. NRS pain score and vital measurements were made again at the 15-30-60th minute of the patients. Side effects that occurred during the treatment process were determined. All data were recorded on a form. Patients were excluded from the study as soon as they wanted to withdraw from the study or in case of an unexpected complication.
In the study, 48 sealed envelopes were prepared in accordance with the treatment protocol to ensure treatment randomisation. There were 3 treatment protocols in the envelopes, consisting of 16 for each group. When the patient suitable for the study arrived, the doctor chose one of these envelopes from the box. The treatment protocol in the selected envelope was applied to that patient.
If lidocaine 10% spray failed to treat pain, tramadol hydrochloride 100 mg was given as an infusion in 150 cc isotonic saline over 15 minutes. If pain control was unsuccessful in narcotic analgesic treatments; intercostal nerve block was used with the view of thoracic surgery.
Three to four mL of 2% prilocaine to be used for the block. The upper and lower segments are blocked for each level from the lateral/posterior axillary line 5-8 cm from the midline. The NRS pain score (0-10) of the patients included in the study was marked at the 0,15,30 and 60th minutes. The higher the score, the higher the severity of the pain.
Patients' age, gender, trauma mechanism, comorbid diseases, vital signs (arterial blood pressure, pulse, fever, respiratory rate, oxygen saturation), symptom, rib fracture side (right-left), number and level, analgesic intake status, emergency department how it came (outpatient-emergency medical service), NRS pain score, need for additional treatment and side effects were recorded. The form was recorded by the emergency medicine assistant or emergency medicine specialist who followed the patient. The investigator was checked by emergency medicine specialists. The main outcome criteria for all three groups are the NRS pain score reduction in the 0-15, 0-30 and 0-60 minute periods. Other main consequences are the need for rescue therapy and side effects.
Data were analysed with SPSS for Windows 16.0. First of all, descriptive statistics are included. Ratio comparisons in tables with 2x2, 3x2, etc. sections were made with Pearson Chi-Square and Fisher's Exact tests. The normality analysis of continuous data was performed with the Shapiro-Wilk test, and it was accepted that the data with a p-value of <0.05 as a result of the test were not normally distributed. In the comparisons between two independent groups, independent Samples-t test was used for normally distributed data and Mann Whitney-U test was used for data that did not show normal distribution. Comparison of more than two consecutive measurements was performed with the rm-ANOVA test for normally distributed data and the Friedman test for non-normally distributed data. For paired subgroup analyses of these tests, Paired Samples-t test was used for normally distributed data, Wilcoxon sign test was used for data that was not normally distributed, and Bonferroni correction was applied for the p-value used in these analyses. The p- value were used for statistical significance and the results with p<0.05 were considered statistically significant.
RESULTS
A total of 48 patients, 16 (33.3%) in all three groups, were included in the study. Although the mean age (58.9/ 56.7/ 51.3 years) and female gender ratio (31.2/ 31.2/ 25.0) in the tramadol and fentanyl groups were higher than the lidocaine group, these differences were not statistically significant (Table I). The distribution of comorbid diseases and admission symptoms are also shown in Table I. Measurements of vital signs (systolic (SBP) and diastolic (DBP) blood pressure, heart rate (HR), respiratory rate, body temperature and oxygen saturation) at admission, at 15-30-60 minutes, were analysed comparatively between the three groups. There was no statistically significant difference between the groups in any of these parameters. The median number of rib fractures was low in the Lidocaine group, the difference was not statistically significant (2.0/ 3.0/ 3.0; p = 0.082). The distributions of trauma mechanism and fracture side parameters in the three groups were found to be statistically similar. Although the rate of patients using analgesics before admission was higher in the Fentanyl group, this difference was not statistically significant (18.8/ 6.2/ 6.2; p = 0.596).
The primary outcome findings are summarised in Table II. Accordingly, the median NRS score at the time of admission was the highest in the Tramadol hydrochloride group and the lowest in the Fentanyl citrate group (8.0/ 7.5/ 7.0). NRS scores at the 15th and 30th minutes were the lowest in the Tramadol hydrochloride group. However, the lowest score at the 60th minute was seen in the Fentanyl citrate group. However, none of these differences were found to be statistically significant. It was observed that there was no need for rescue medication or intervention in any group of patients. No drug side effects were detected in the lidocaine 10% spray group. While hypotension developed in 1 patient (6.2%) in the tramadol hydrochloride and fentanyl citrate groups, nausea-vomiting and/or dizziness were observed in 3 patients (18.8%) in the fentanyl citrate group. Tongue paresthesia was also observed in 1 (6.2%) patient in the tramadol hydrochloride group. When the amount of decrease in pain score between 0-15, 0-30 and 0-60 minutes was analysed, the median of the highest decrease in all 3 periods was found in the Tramadol hydrochloride group. Fentanyl citrate group came second in the 0-15 and 0-30 periods, while the median decrease in the Lidocaine 10% spray group in the 0-60 period was higher than the Fentanyl citrate group. However, it is seen that the difference in all three parameters here is not statistically significant. NRS scores and the graph of the differences in these scores over the periods are shown in Figure 1. The first hour of NRS pain score reduction of the patients was followed up. Again, the increase in pain intensity was in the range of 4-6 hours. In this case, the doctor who followed the patient applied his treatment protocol.
When the course of vital signs was analysed (Table III), a statistically significant decrease was found for SBP in the Tramadol hydrochloride and Fentanyl citrate groups. This significant decrease was detected within the 15-60 period in the Tramadol hydrochloride group and within the 0-60 period in the Fentanyl citrate group. No significant change was detected in the follow-up for DBP. There was a statistically significant decrease in HR in the Tramadol hydrochloride group. It was observed that this decrease was especially in the 15-60 period. However, the quartile values and confidence intervals of 25-75% for both SBP and HR were found to be within clinically normal limits during the entire follow-up.
DISCUSSION
The aim of this study was to achieve successful results in acute pain control in rib fractures with lidocaine 10% spray, which is easily applicable, inexpensive, and has a very low side-effect profile. In addition, this study is important because it is the first study conducted with lidocaine 10% spray in patients with rib fractures. As the number of rib fractures increases in most studies, it causes an increase in the mortality rate along with the complications it causes. In fact, it is an important cause of late post-traumatic death. For this reason, it has been shown that mortality rates are reduced with a care model in the approach to rib fractures. Multimodal effective pain therapy has a healing feature in the performance of pulmonary functions.13 The effectiveness of the analgesic treatment methods to be chosen against each other was investigated, and similar efficacy was found mostly in pain control. However, the side-effect profile and the easy applicability of the method provided superiority among treatment protocols. Although nonsteroidal anti-inflammatory analgesics and opiate analgesic treatments are the most preferred ones, spinal epidural analgesia and intercostal nerve blockade are also preferred depending on the situation.14,15
In this study, no statistically significant difference was found between the groups in terms of age, gender distribution, presence of additional disease, emergency admission symptoms, vital signs, and trauma mechanisms. There was no significant difference between the groups in the distribution of the number of rib fractures and between the right-left side fractures. This shows that there is a balanced distribution between the groups. Due to the subjective nature of pain, balance between groups was an important value for the endpoint of the study.
Table I: Demographics and vital signs.
|
Parameters |
Drug groups |
p-value |
|||
|
Lidocaine |
Tramadol |
Fentanyl |
|||
|
Age (year) |
51.3±15.7 |
58.9±16.4 |
56.7±16.0 |
0.391 |
|
|
Gender- n (%) |
Male |
12 (75.0) |
11 (68.8) |
11 (68.8) |
1.000 |
|
Female |
4 (25.0) |
5 (31.2) |
5 (31.2) |
||
|
Comorbidity- n (%) |
8 (50.0) |
12 (75.0) |
6 (37.5) |
0.095 |
|
|
Comorbidities- n (%) |
HT |
7 (43.8) |
7 (43.8) |
5 (31.2) |
0.706 |
|
DM |
2 (12.5) |
6 (37.5) |
2 (12.5) |
0.170 |
|
|
COPD / asthma |
0 (0.0) |
3 (18.8) |
1 (6.2) |
0.304 |
|
|
CAD |
0 (0.0) |
3 (18.8) |
1 (6.2) |
0.304 |
|
|
Other |
3 (18.8) |
3 (18.8) |
3 (18.8) |
- |
|
|
Symptoms- n (%) |
Chest pain |
12 (75.0) |
11 (68.8) |
13 (81.2) |
0.913 |
|
Dyspnea |
1 (6.2) |
1 (6.2) |
0 (0.0) |
1.000 |
|
|
Back pain |
1 (6.2) |
3 (18.8) |
2 (12.5) |
0.859 |
|
|
Flank pain |
4 (25.0) |
4 (25.0) |
1 (6.2) |
0.345 |
|
|
SBP (mmHg) |
Initial |
121.0 (114.5-135.5) |
140.0 (119.5-160.0) |
131.0 (122.5-144.0) |
0.210 |
|
15-min |
123.5 (110.5-142.5) |
140.0 (120.0-150.0) |
126.5 (120.0-142.5) |
0.280 |
|
|
30-min |
131.8±19.7 |
137.9±26.0 |
131.4±18.3 |
0.633 |
|
|
60-min |
128.1±19.9 |
134.7±23.0 |
127.5±18.6 |
0.550 |
|
|
DBP (mmHg) |
Initial |
71.9±10.6 |
73.6±9.3 |
70.6±8.1 |
0.665 |
|
15-min |
73.9±10.4 |
73.8±7.8 |
75.3±8.8 |
0.875 |
|
|
30-min |
74.4±8.2 |
73.4±7.9 |
75.6±7.5 |
0.723 |
|
|
60-min |
75.3±9.5 |
72.3±6.5 |
72.4±9.9 |
0.546 |
|
|
HR (per minute) |
Initial |
82.8±10 |
80,1±14,3 |
83.7±9.4 |
0.660 |
|
15-min |
83.4±12.3 |
79.1±12.5 |
83.3±10.1 |
0.503 |
|
|
30-min |
80.9±11.4 |
77.4±12.8 |
81.4±9.1 |
0.551 |
|
|
60-min |
80.2±10.6 |
75.9±12.1 |
81.4±11.2 |
0.354 |
|
|
RR (per minute) |
Initial |
18.4±1.8 |
18.7±2.2 |
18.3±1.6 |
0.804 |
|
15-min |
18.3±2.2 |
18.0±1.7 |
17.3±1.5 |
0.342 |
|
|
30-min |
16.7±1.4 |
17.1±1.5 |
16.5±1.2 |
0.519 |
|
|
60-min |
16.0 (15.0-17,0) |
16.5 (15.5-17.5) |
16.0 (15.5-17.0) |
0.538 |
|
|
BT (°C) |
Initial |
36.35 (36.1-36.7) |
36.2 (36.1-36.55) |
36.3 (36.2-36.6) |
0.508 |
|
15-min |
36.3 (36.2-36.5) |
36.25 (36-36,5) |
36.3 (36.2-36.5) |
0.468 |
|
|
30-min |
36.25 (36.1-36.5) |
36.20 (36.1-36.4) |
36.3 (36.1-36.5) |
0.782 |
|
|
60-min |
36.35 (36.2-36.5) |
36.3 (36.1-36.5) |
36.25 (36.2-36.45) |
0.612 |
|
|
sO2 (%) |
Initial |
95.4±1.7 |
94.6±1.5 |
95.9±1.9 |
0.109 |
|
15-min |
95.7±1.4 |
95.1±1.4 |
95.4±1.6 |
0.484 |
|
|
30-min |
96.1±1.2 |
95.4±1.5 |
95.9±1.4 |
0.341 |
|
|
60-min |
96.5 (96.0-97.0) |
95.5 (95.0-97.0) |
96.0 (95.0-97.0) |
0.300 |
|
|
Trauma mechanism- n (%) |
MVC |
9 (56.2) |
5 (31.2) |
8 (50.0) |
0.294 |
|
Fall |
6 (37.5) |
11 (68.8) |
8 (50.0) |
||
|
Struck by |
1 (6.2) |
0 (0,0) |
0 (0.0) |
||
|
Number of fractures |
2.0 (2.0-3.0) |
3.0 (2.0-3.0) |
3.0 (2.5-3.0) |
0.085 |
|
|
Fracture side- n (%) |
Right |
7 (43.8) |
8 (50.0) |
9 (56.2) |
0.874 |
|
Left |
8 (50.0) |
6 (37.5) |
5 (31.2) |
||
|
Bilateral |
1 (6.2) |
2 (12.5) |
2 (12.5) |
||
|
Prior analgesic use- n (%) |
1 (6.2) |
1 (6.2) |
3 (18.8) |
0.596 |
|
|
Admission via EMS- n (%) |
13 (81.2) |
13 (81.2) |
15 (93.8) |
0.671 |
|
|
One-Way ANOVA test (mean ± SD): Age, SBP-30, SBP-60, DBP-0, DBP-15, DBP-30, DBP-60, HR-0, HR-15, HR-30, HR-60, RR-0, RR-15, RR-30, sO2-0, sO2-15, sO2-30, sO2-60. Kruskal Wallis test (median- IQR): SBP-0, SBP-15, RR-60, BT-0, BT-15, BT-30, BT-60, sO2-60, number of fractures. Fisher’s Exact test (n- %): Gender, DM, COPD, CAD, chest pain, dyspnea, back pain, flank pain, trauma mechanism, fracture side, prior analgesic use, admission type. Pearson Chi-square test (n- %): Comorbidity, HT. HT: hypertension, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, CAD: coronary artery disease, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, RR: respiratory rate, BT: body temperature, sO2: oxygen saturation, min: minute, MVC: motor vehicle collision, EMS: emergency medical service, SD: standard deviation, IQR: interquartile range |
|||||
The authors could not find any literature showing the use of lidocaine 10% spray for analgesic purposes in rib fractures. However, there are studies where it is used with different indications. It has been used in gastrointestinal endoscopic applications, intravenous vascular access, before blood gas collection from the radial artery, in otolaryngological procedures and cervical laminaria placement, and effective results have been obtained in pain control.16 Due to the rapid onset of the effect of lidocaine spray in Denmark, its use is recommended during vascular access.17 In this study, although tramadol seemed to be slightly more effective in reducing pain between periods compared to the NRS pain score, there was no statistically significant difference. The median of the baseline NRS score was the highest in this group, while fentanyl had the lowest median. In addition, the duration of action of lidocaine is thought to be 15 minutes and is shorter than other opiates.11,17 Opiates were given to patients as an infusion, which may have led to longer-lasting effectiveness. Fentanyl's lipophilic feature allows it to pass quickly to the central nervous system. Its half-life varies between 3-8 hours due to its re-release feature. However, continuous infusion rather than bolus administration prolongs the duration of action.18
Table II: Primary outcomes.
|
Parameters |
Groups |
p-value |
|||
|
Lidocaine |
Tramadol |
Fentanyl |
|||
|
NRS scores (cm) |
Initial |
7.5 (6.0-8.0) |
8.0 (6.0-9.5) |
7.0 (6.5-8.0) |
0.667 |
|
15-min |
5.4±2.4 |
5.3±1.9 |
5.5±2.2 |
0.970 |
|
|
30-min |
3.8±1.8 |
3.4±2.1 |
3.6±2.2 |
0.869 |
|
|
60-min |
2.0 (1.0-3.0) |
2.0 (1.0-3.5) |
1.0 (0.0-3.5) |
0.743 |
|
|
Rescue drug need- n (%) |
0 (0.0) |
0 (0,0) |
0 (0.0) |
- |
|
|
Adverse reactions- n (%) |
None |
16 (100.0) |
14 (87.5) |
12 (75.0) |
- |
|
Nausea / emesis / vertigo |
0 (0.0) |
0 (0,0) |
3 (18.8) |
||
|
Hypotension |
0 (0.0) |
1 (6.2) |
1 (6.2) |
||
|
Tongue paresthesia |
0 (0.0) |
1 (6.2) |
0 (0.0) |
||
|
NRS diff (cm) |
Diff 0-15 min |
1.5 (1.0-3.0) |
2.5 (1.0-4.0) |
2.0 (1.0-2.0) |
0.465 |
|
Diff 0-30 min |
3.0 (2.5-5.0) |
5.0 (3.5-5.5) |
4.0 (3.0-5.0) |
0.256 |
|
|
Diff 0-60 min |
5.5 (4.0-6.0) |
6.0 (5.0-7.0) |
5.0 (3.5-7.0) |
0.678 |
|
|
One-Way ANOVA test (mean ± standard deviation): NRS-15, NRS-30. Kruskal Wallis test (median- IQR): NRS-0, NRS-60, NRS diff 0-15, NRS diff 0-30, NRS diff 0-60. NRS: Numeric Rating Scale, min: minute, diff: difference, cm: centimeter, IQR: interquartile range |
|||||
Table III: Follow-up of the vital signs.
|
|
0 (initial) |
15 min |
30 min |
60 min |
p-value |
|
|
SBP |
Lidocaine |
121.0 (114.5-135.5) |
123.5 (110.5-142.5) |
125.0 (120.0-141.0) |
124.0 (113.5-131.5) |
0.419* |
|
Tramadol |
140.0 (119.5-160.0) |
140.0 (120.0-150.0) |
134.0 (121.5-147.0) |
133.0 (119.5-145.5) |
0.023* |
|
|
Fentanyl |
131.0 (122.5-144.0) |
126.5 (120.0-142.5) |
130.0 (120.0-136.5) |
126.5 (119.0-133.5) |
0.003* |
|
|
DBP |
Lidocaine |
71.9 ± 10.6 |
73.9 ± 10.4 |
74.4 ± 8.2 |
75.3 ± 9.5 |
0.530 |
|
Tramadol |
73.6 ± 9.3 |
73.8 ± 7.8 |
73.4 ± 7.9 |
72.3 ± 6.5 |
0.691 |
|
|
Fentanyl |
70.6 ± 8.1 |
75.3 ± 8.8 |
75.6 ± 7.5 |
72.4 ± 9.9 |
0.142 |
|
|
HR |
Lidocaine |
82.8 ± 10.0 |
83.4 ± 12.3 |
80.9 ± 11.4 |
80.2 ± 10.6 |
0.129 |
|
Tramadol |
80.1 ± 14.3 |
79.1 ± 12.5 |
77.4 ± 12.8 |
75.9 ± 12.1 |
0.010 |
|
|
Fentanyl |
83.7 ± 9.4 |
83.3 ± 10.1 |
81.4 ± 9.1 |
81.4 ± 11.2 |
0.439 |
|
|
*Friedman test (median- IQR): SBP (Wilcoxon sign test and Paired Samples-t test were used for subgroup analysis, and Bonferroni correction was used for p-value). †Repeated measures-ANOVA (mean ± SD): DBP, HR (Paired Samples-t test was used for subgroup analysis, and Bonferroni correction was used for p-value). As a result of sub-group analysis, it was found that the difference in SBP parameter in the Tramadol group was due to the differences in the 0-60 and 15-60 periods, while the difference in the Fentanyl group was due to the difference int the 0-60 period. The difference in the HR parameter in the Tramadol group is due to the difference in the 15-60 period. Min: minute, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, IQR: interquartile range, SD: standard deviation. |
||||||
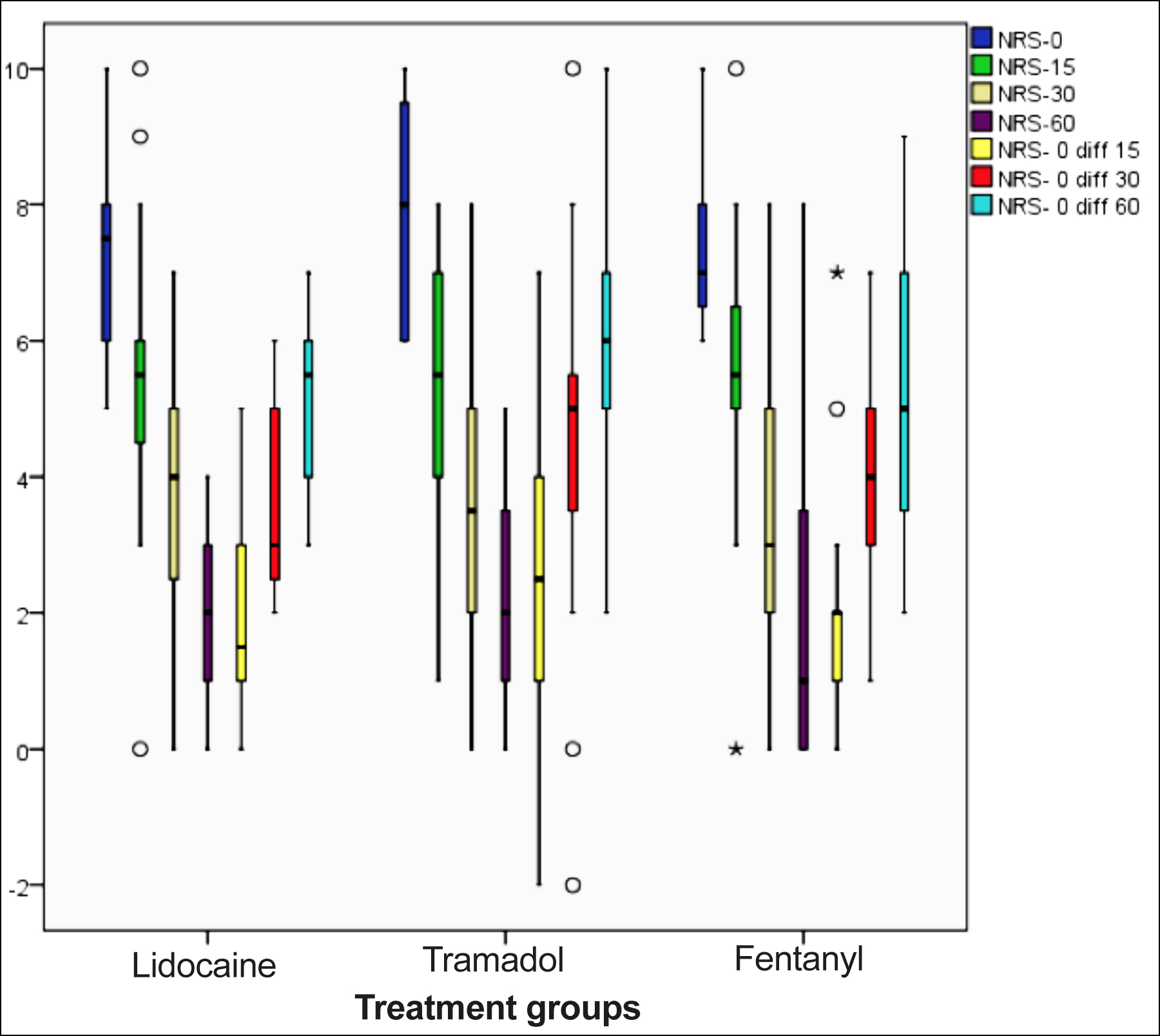 Figure 1: Relationship between numerical analog scale score and time.
Figure 1: Relationship between numerical analog scale score and time.
Tramadol has an effective analgesic effect on spinal, supraspinal and peripheral nerves. Even in vivo studies, intradermal applications provided similar analgesic efficacy to lidocaine. It did this by its effect on sodium channels. When viewed from these aspects, tramadol is considered a superior analgesic agent because it provides analgesic properties in many different ways.19 Despite these differences, lidocaine 10% spray successfully reduced pain and did not require an additional rescue analgesic drug and method. It is thought that this effect may be due to the effect of lidocaine on free nerve endings. Free nerve endings contain sensory receptors for pain and temperature. There are studies showing that lidocaine is effective on these specific receptors.20,21
However, side effects such as hypotension, dizziness, nausea, and vomiting were observed in opiate group drugs as expected. The most adverse effects occurred in the fentanyl group in accordance with the literature. Finally, when the vital signs of the patients were examined, a statistically significant decrease was observed in SBP in those given opiate group drugs. HR showed a significant decrease in patients given tramadol. The reductions in SBP and HR produced no clinically relevant effects. The side-effect profile associated with opiates may progress from hypotension, bradycardia, tachycardia, nausea, vomiting, and drowsiness to respiratory depression.18,19 There were no side effects in the patients who had applied lidocaine spray. There was no deterioration in the SBP, DBP, and HR parameters of the patients who were given lidocaine spray, which required clinical intervention. This safe situation is due to the dose and topical application. In addition, since patients over the age of 18 years were included in this study, it may have reduced the possibility of side effects in terms of surface area. In the literature reviews, fearful systemic side effects of local anaesthetics such as lidocaine can be seen very rarely. These effects are observed when the topical application dose is exceeded, especially in children, because the surface area is small or when the drug reaches the vascular circulation. Allergic reactions due to topical applications and methemoglobinemia in children can be seen very rarely.22
Since the administration method of the agents used in this study was local and intravenous, it was not planned blindly. The preference for trauma patients in this study may have shown the subjective value of pain to be more severe in the description of pain. Because patients experience a constant feeling of pain with breathing, which can cause this situation. In addition, as the anxiety of the patients decreased, the decrease in pain intensity may have been affected. In addition, the difference in pain thresholds of individuals was another limitation of this study. There are certainly various scorings that include advantages and disadvantages in terms of use among pain scores. Therefore, in this study, it was preferred to use the NRS pain score, where patients can easily describe their pain. The ease of use of the agent and the fact that there is no need for vascular access has drawn an important roadmap to carry out this study.
CONCLUSION
Lidocaine spray can be used effectively and safely primarily as an initial treatment for multimodal pain relief in rib fractures. It has the same efficacy compared to opiate derivative analgesics and provides a great advantage in terms of side effects.
ETHICAL APPROVAL:
The study protocol was approved by the Ministry of Health Ankara City Hospital ethics committee (E1-21-1678). The study was conducted in accordance with the principles of the Declaration of Helsinki.
PATIENTS’ CONSENT:
Patient consent was not obtained because it was a retrospective file study.
DATA SHARING STATEMENT: The data that support the findings of this study are available from the corresponding author upon reasonable request.
COMPETING INTEREST:
The authors declared no competing interest with respect to the authorship and/or publication of this article.
AUTHORS’ CONTRIBUTION:
ABE, SD, AS: Idea/concept, designing the study, controlling for variables, collecting and analysing data, conducting a literature review, and approving the final version of the manuscript.
REFERENCES
- Tignanelli CJ, Rix A, Napolitano LM, Hemmila MR, Sisi Ma, Kummerfeld E. Association between adherence to evidence-based practices for treatment of patients with traumatic rib fractures and mortality rates among US trauma centers. JAMA Netw Open 2020; 3(3):e201316. doi.org/10.1001/jamanetworkopen.2020.1316.
- Simon JB, Wickham AJ. Blunt chest wall trauma: An overview. Br J Hos Med 2019; 80(12):711-5. doi.org/10. 12968/hmed.2019.80.12.711.
- Jeffery Z, Everson M, Carty S. Management of rib fractures. Br J Hos Med 2019; 80(10):C146-9. doi.org/10.12968/ hmed.2019.80.10.C146.
- Akça AH, Şaşmaz Mİ, Kaplan Ş.Kinesiotaping for isolated rib fractures in emergency department. Am J Emerg Med 2020; 38(3):638-40. doi.org/10.1016/j.ajem.2019.11.049.
- Ingalls NK, Horton ZA, Bettendorf M, Frye I, Rodriguez C. Randomised, double-blind, placebo-controlled trial using lidocaine patch 5% in traumatic rib fractures. J Am Coll Surg 2010; 210(2):205-9. doi.org/10.1016/j.jamcollsurg.2009. 10.020.
- Krdzalic G, Musanovic N, Kradzalic A, Mehmedagic I, Kesetovic A. Opiate analgesia treatment reduced early inflammatory response after severe chest injuries. Med Arch 2016; 70(6):457-9. doi.org/10.5455/medarh.2016.70.457-459.
- Rodriguez MS, Ochoa D, Herrador C, Belmonte C, Román M, Alday E, et al. Polymorphisms associated with fentanyl pharmacokinetics, pharmacodynamics and adverse effects. Basic Clin Pharmacol Toxicol 2019; 124(3):321-9. doi. org/10.1111/bcpt.13141.
- Bravoa L, Mico JA, Berrocoso E. Discovery and development of tramadol for the treatment of pain. Expert Opin Drug Discov 2017; 12(12):1281-91. doi.org/10.1080/17460 441.2017.1377697.
- Zink KA, Mayberry JC, Peck EG, Schreiber MA. Lidocaine patches reduce pain in trauma patients with rib fractures. Am Surg 2011; 77(4):438-42. doi.org/10.1177/0003134 81107700419.
- Zhu J, Liu J, Shen G, Zhong T, Yu X. Comparison of efficacy outcomes of lidocaine spray, topical lidocaine ınjection, and lidocaine general anesthesia in nasal bone fractures surgeries: A randomised, controlled trial. Med Sci Monit 2018; 24:4386-94. doi.org/10.12659/MSM.908468.
- Datemaa J, Veldhuisa J, Bekhof J. Lidocaine spray as a local analgesic for intravenous cannulation: A randomised clinical trial. Eur J Emerg Med 2019; 26(1):24-8. doi.org/10. 1097/MEJ.0000000000000496.
- Aktaş YY, Karabulut N. The use of cold therapy, music therapy and lidocaine spray for reducing pain and anxiety following chest tube removal. Complement Ther Clin Prac 2019; 34:179-84. doi.org/10.1016/j.ctcp.2018.12.001.
- Witt CE, Bulger EM. Comprehensive approach to the management of the patient with multiple rib fractures: A review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open 2017; 2(1):1-7. doi.org/10.1136/tsaco-2016-000064.
- Kaiser AM, Zollinger A, De Lorenzi D, Largiadèr F, Weder W. Prospective, randomized comparison of extrapleural versus epidural analgesia for postthoracotomy pain. Ann Thorac Surg 1998; 66(2):367-72. doi.org/10.1016/s0003-4975 (98)00448-2.
- Tekşen S, Oksüz G, Oksüz H, Sayan M, Arslan M, Urfalıoglu A, et al. Analgesic efficacy of the serratus anterior plane block in rib fractures pain: A randomised controlled trial. Am J Emerg Med 2021; 41:16-20. doi.org/10.1016/j.ajem. 2020.12.041.
- Gur A, Tekin E. 10% Lidocaine spray as a local anaesthetic in blood gas sampling: A randomised, double-blind, placebo-controlled study. Am J Emerg Med 2021; 49:89-93. doi.org/10.1016/j.ajem. 2021.05.060.
- Van Dongen EC, Eppens EF, De Jonge N, Roelofs MAMA. Dutch guideline: How to take a veneous blood sample; 2013:1-45. www.nvkc.nl/sites/default/files/2.pdf.
- Schug SA, Ting S. Fentanyl formulations in the management of pain: An update. Drugs 2017; 77(7):747-63. doi. org/10. 1007/s40265-017-0727-z.
- Barakat A. Revisiting tramadol: A multi-modal agent for pain management. CNS Drugs 2019; 33(5):481-501. doi. org/10.1007/s40263-019-00623-5.
- Sakai T, Tomiyasu S, Yamada H, Ono T, Sumikawa K. Quantitative and selective evaluation of differential sensory nerve block after transdermal lidocaine. Anesth Analg 2004; 98(1):248-51. doi.org/10.1213/01.ANE.0000093232.72967. 76.
- Sessle BJ. Mechanisms of oral somatosensory and motor functions and their clinical correlates. J Oral Rehabil 2006; 33(4):243-61. doi.org/10.1111/j.1365-2842.2006.01623.x.
- Cherobin ACFP, Tavares GT. Safety of local anaesthetics. An Bras Dermatol 2020; 95(1):82-90. doi.org/10.1016/j.abd. 2019.09.025.