Comparison of Laser Haemorrhoidoplasty and Ferguson Haemorrhoidectomy in Treating Grade III and Grade IV Haemorrhoids: A Prospective Randomised Study
By Tuba MertAffiliations
doi: 10.29271/jcpsp.2023.01.45ABSTRACT
Objective: To compare the efficiency and safety of laser haemorrhoidoplasty (LH) with Ferguson haemorrhoidectomy (FH) in patients with third- and fourth-grade haemorrhoids.
Study Design: Randomised controlled trial.
Place and Duration of Study: General Surgery Clinic, Medipol University Pendik Hospital, İstanbul, Turkey, from 1st December 2021 to 1st May 2022.
Methodology: The patients who had an indication for surgery for grade III or grade IV haemorrhoidal disease (HD) and who were 18 years and older were randomly allocated to the two study groups. While LH was performed using a 980-diode laser in the patients enrolled in the laser group, a standard FH was performed using diathermy in the patients in the second study group. The length of surgery (LOS), the number of excised lumps, wound healing time, time to symptom relief, pre- and postoperative Visual Analogue Scale (VAS) scores and the difference between them (Δ VAS), and complication rates were compared between two study groups.
Results: LH had less LOS with a similar number of excised lumps, furthermore, it provided faster-wound healing and less time-to-symptom relief when compared to FH. The median VAS score decreased from 5 to 0 in the LH group and from 5 to 2 in FH, and Δ VAS scores of the groups were statistically significantly different (p<0.001). LH also had better outcomes than FH in terms of having any type of postoperative complication.
Conclusion: LH might be an alternative treatment modality in patients with grade III and grade IV HD with a low level of complication rate.
Key Words: Haemorrhoids, Laser therapy, Haemorrhoidectomy, Operative time, Pain measurement, Postoperative complications.
INTRODUCTION
Haemorrhoidal disease (HD) is a common proctologic disorder that affects millions of people globally with an estimated prevalence ranging between 11% and 39% in different types of studies,1-4 and rising to 60% in different age groups.2 While different evidence-based management algorithms were recommended,5-9 there is not a definitive treatment method because of the highly variable predisposing factors and various covariates affecting the success of treatment.4,10,11
The preference of treatment modalities depends on the location and severity of prolapses, the grade of the disease, being a primary or recurrent disease, being with or without complication, and also other patient-related variables.1,5-8 In patients with grade III and grade IV HD, surgical approaches such as doppler-guided haemorrhoidal ligation, haemorrhoidopexy, mucopexy, haemorrhoidal artery ligation, and haemorrhoidectomy (open/closed/stapled) are widely used treatment methods with different success and recurrence rates and safety levels.5,6,8,12
Laser technology has been used for excisional and non-excisional procedures in patients with different grades of HD effectively and safely.14-17 While there are many studies aimed to compare the non-excisional laser therapies with Milligan Morgan Haemorrhoidectomy (MMH) or rubber band ligation,14 to the best of the author’s knowledge, there is not a published randomised clinical trial (RCT) comparing laser haemorrhoidoplasty (LH) with Ferguson Haemorrhoidectomy (FH) in patients with grade III and IV HD in the literature. Consequently, this study aimed to compare the efficiency and safety of LH with FH in patients with third- and fourth-grade haemorrhoids.
METHODOLOGY
It was a prospective randomised controlled surgical study using random permuted blocks of 4 with an allocation ratio of 1:1. This study was conducted at the general surgery department of Medipol University Pendik Hospital between 1st December 2021 and 1st May 2022.
The CONSORT guidelines and the Declaration of Helsinki were followed during the study. An estimated minimum sample size of 49 participants in each study group was calculated with an effect size of 0.6, a type 1 error of 0.05, and a power of 0.90 via GPower 3.1 software.
First, a full medical history was taken, and then a detailed physical examination was performed on all patients. Next, all eligible patients were evaluated in terms of the inclusion and exclusion criteria of the study. The two inclusion criteria were age 18 years and older, and an indication for surgery for grade III or grade IV haemorrhoids. Patients with thrombosed haemorrhoids, perianal fistula, perianal abscess, inflammatory bowel disease, chronic obstructive pulmonary disease, cirrhosis, HIV positivity, ischemic heart disease, migraine, hypertension, uncontrolled diabetes, bleeding disorder, and/or immunosuppression, and pregnant women were excluded from the study. Patients using anticoagulants or acetylsalicylic acid were directed to discontinue their medication 7 days before surgery. Following fulfilling the inclusion and exclusion criteria, patients were allocated to the study groups randomly using opaque and sealed envelopes to ensure allocation concealment.
Two hours before operations, two enemas were administered to all patients. Both two procedures were performed in lithotomy position under spinal anaesthesia. Before the operation, an anorectal exploration was done using a 15 cm proctoscope (Aesculap, Germany, B. Braun Medikal Dış Tic. A.Ş.) following a digital anal examination. A standard FH was performed using diathermy in patients allocated to the excisional haemorrhoidectomy group.18
The laser procedure was performed using a 980-diode laser (NeoVlaser, Israel, Atak Cerrahi A.Ş.) through a 1000-nm optic fibre. Five laser shots were delivered with 13-watt power. Each shot lasted 1.2 seconds and then paused for 0.6 seconds to shrink the mucosal and submucosal tissue to a depth of 5 mm, approximately.
Patients were discharged on the postoperative first day and were treated with the combination therapy of a laxative agent, oral metronidazole, and an oral analgesic for 1 week postoperatively. They were trained on how to take a warm water bath on the surgical sites, and a 5-minute warm water bath at least three times a day for one week was recommended. All surgical procedures were performed by one surgeon who had at least 20-year experience in proctologic surgery.
The age, gender, symptoms, and clinical findings of the patients were recorded. The haemorrhoids that protruded outside and required manual reduction were classified as grade III, and those constantly prolapsed as grade IV. The number of involved quadrants was also recorded. To ensure a standard lesion localisation approach, the perianal region was divided into four anatomic quadrants; left anterior, left posterior, right anterior, and right posterior.
There were two groups of the primary outcomes of the study. The first group, which was used for the comparison of the efficiency of the surgical methods, included surgical outcomes and pain relief. Surgical outcomes consisted of the length of surgery (LOS) (minutes), the number of excised lumps, wound healing time (days), and time to symptom relief (days). Pain relief was defined as the difference between pre- and postoperative Visual Analogue Scale (VAS) scores which were measured using a scale ranging from 0 (no pain) to 10 (unbearable pain) points. This difference (Δ VAS) was calculated by subtracting the preoperative VAS score from the postoperative VAS score which was recorded on the 7th day after surgery at a control visit. All VAS scores were recorded by a general surgeon. Besides the temporal decrease in VAS score, the presence of actual improvement in pain was also investigated by comparing preoperative and postoperative VAS scores between the study groups.
The second group of primary outcomes includes the presence of several complications of the surgical methods (bleeding, thrombosis, abscess, incontinence, anal fissure, anal fistula, residual haemorrhoid, urinary retention), the presence of any complication, and the need for surgery for complications. The safety of the two surgical modalities was evaluated using these variables. All patients were followed up via a weekly telephone interview for the occurrence of the complications for 60 days, and they were evaluated in two control visits, one on the postoperative 7th day, and the other at the end of the follow-up period.
SPSS version 20 (IBM Corp. in Armonk, NY) was used to conduct statistical analyses. Descriptive statistics were presented as mean with standard deviation and median with interquartile range for numeric data, and frequency with percentage for categorical data. Shapiro-Wilk test and Kolmogorov-Smirnov test were used for evaluating the normality of the distribution of the numerical variables. Mann–Whitney U-Test was used to compare non-normally distributed numerical variables, and Pearson chi-square test or Fisher’s exact test was used for comparing categorical variables between the study groups. A value of p<0.05 was considered the statistically significant level.
RESULTS
This clinical trial was performed with 100 patients admitted to the general surgery clinic of a tertiary-level hospital with several symptoms related to HD. Patients were randomised into the two-study arms half and half, there was no loss to follow-up, and all participants completed the study.
Table I: Demographics, baseline clinical characteristics, and postoperative outcomes of the patients.|
Characteristics |
Laser group (n= 50) |
Ferguson group (n= 50) |
p |
|
Age (years), median (IQR) |
32.0 (29.0-44.5) |
31.5 (26.8-42.3) |
0.289* |
|
Sex (female), n (%) |
41 (82.0) |
39 (78.0) |
0.617* |
|
Bleeding, n (%) |
28 (56.0) |
29 (58.0) |
0.840** |
|
Dyschezia, n (%) |
28 (56.0) |
27 (54.0) |
0.841** |
|
Grade, n (%) |
|
|
|
|
3rd |
31 (62.0) |
33 (66.0) |
0.677** |
|
4th |
19 (38.0) |
17 (34.0) |
|
|
Number of involved quadrants, n (%) |
|
|
|
|
1 |
14 (28.0) |
16 (32.0) |
0.948*** |
|
2 |
24 (48.0) |
21 (42.0) |
|
|
3 |
10 (20.0) |
11 (22.0) |
|
|
4 |
2 (4.0) |
2 (4.0) |
|
|
IQR: Interquartile range, *Mann-Whitney U Test was used, **Pearson Chi-square Test was used, ***Fisher’s Exact Test was used. |
|||
Table II: Surgical outcomes of the patients.
|
Characteristics |
Laser group (n= 50) |
Ferguson group (n= 50) |
p |
|
Length of surgery, n (%) |
|
|
|
|
Less than 20 minutes |
50 (100.0) |
17 (34.0) |
<0.001* |
|
20 minutes and more |
0 (0.0) |
33 (66.0) |
|
|
Number of excised lumps, median (IQR) |
2.0 (1.0-2.0) |
2.0 (1.0-2.0) |
0.946** |
|
Wound healing time, n (%) |
|
|
|
|
Less than 20 days |
50 (100.0) |
20 (40.0) |
<0.001* |
|
20 days and more |
0 (0.0) |
30 (60.0) |
|
|
Time to symptom relief, n (%) |
|
|
|
|
Less than 20 days |
50 (100.0) |
19 (38.0) |
<0.001* |
|
20 days and more |
0 (0.0) |
31 (62.0) |
|
|
Preoperative VAS |
|
|
|
|
Mean±SD |
5.14±1.34 |
5.08±1.29 |
0.859** |
|
Median (IQR) |
5.00 (4.00-6.00) |
5.00 (4.00-6.00) |
|
|
Postoperative VAS |
|
|
|
|
Mean±SD |
0.18±0.48 |
2.04±1.05 |
<0.001** |
|
Median (IQR) |
0.00 (0.00-0.00) |
2.00 (1.00-3.00) |
|
|
Δ VAS |
|
|
|
|
Mean±SD |
4.96±1.16 |
3.04±0.95 |
<0.001** |
|
Median (IQR) |
5.00 (4.00-6.00) |
3.00 (2.00-4.00) |
|
|
Bleeding, n (%) |
0 (0.0) |
3 (6.0) |
0.242*** |
|
Thrombosis, n (%) |
1 (2.0) |
2 (4.0) |
>0.999*** |
|
Abscess, n (%) |
0 (0.0) |
1 (2.0) |
>0.999*** |
|
Incontinence, n (%) |
0 (0.0) |
1 (2.0) |
>0.999*** |
|
Anal fissure, n (%) |
0 (0.0) |
5 (10.0) |
0.056*** |
|
Anal fistula, n (%) |
0 (0.0) |
0 (0.0) |
n/a |
|
Residual haemorrhoid, n (%) |
1 (2.0) |
4 (8.0) |
0.362*** |
|
Urinary retention, n (%) |
0 (0.0) |
2 (4.0) |
0.495*** |
|
Any complication, n (%) |
2 (4.0) |
9 (18.0) |
0.025* |
|
Need for surgery for complications, n (%) |
0 (0.0) |
3 (6.0) |
0.242*** |
|
IQR: Interquartile range, VAS: Visual analogue scale, SD: Standard deviation, IQR: Interquartile range, Δ VAS: The difference between preoperative and postoperative VAS scores. *Pearson Chi-square Test was used, **Mann-Whitney U Test was used, ***Fisher’s Exact Test was used. |
|||
The demographics and baseline clinical characteristics of the patients were summarised in Table I. The median age of the laser group was 32.0 years, and the Ferguson group was 31.5 years, while 41 patients (82.0%) in the LH group and 39 patients (78.0%) in the FH group were women. Bleeding was seen in 28 patients (56.0%) in the LH group, and 29 patients (58.0%) in the FH group. Similarly, 28 patients (56.0%) in the LH group and 27 patients (54.0%) in the FH group presented with dyschezia. Sixty-two percent (n=31) of the LH group and 66.0% of the FH group (n=33) had grade III haemorrhoids and 19 patients (38.0%) in the LH group and 17 patients (34.0%) in the FH group had grade IV haemorrhoids. The majority of patients had involvement in one or two quadrants. All demographics and baseline clinical features were statistically similar between LH and FH groups (Table I).
While LOS was less than 20 minutes in all patients who underwent LH, the surgery took 20 minutes or more in 33 patients (66.0%) in the Ferguson group. This difference in LOS between the groups was statistically significant (p<0.001). The median number of excised lumps was 2 (IQR: 1.0-2.0) in both groups. Although both wound healing time and time to symptom relief were under 20 days in all patients in the laser group; in the Ferguson group, wound healing time was less than 20 days in 20 patients (40.0%), 20 days or more in 30 patients (60.0%), and time to symptom relief was less than 20 days in 19 patients (38.0%), 20 days and more in 31 patients (62.0%). Statistically significant differences were found in both wound healing time and time to symptom relief between the two surgical techniques (p<0.001 and p<0.001, respectively) (Table II)
The median preoperative VAS scores were 5.0 and statistically similar in both study groups. A decrease of approximately 5.0 points was observed in the VAS score after surgery in the laser group, and the median postoperative VAS score was 0.0. However, the median VAS score reduction in the Ferguson group was about 3.0 points and the median postoperative VAS score was 2.0. In other words, when compared to FH, a statistically significantly lower postoperative VAS score was obtained (p<0.001), with a statistically significantly greater improvement in the score of the laser group (p<0.001, Table II and Figure 1).
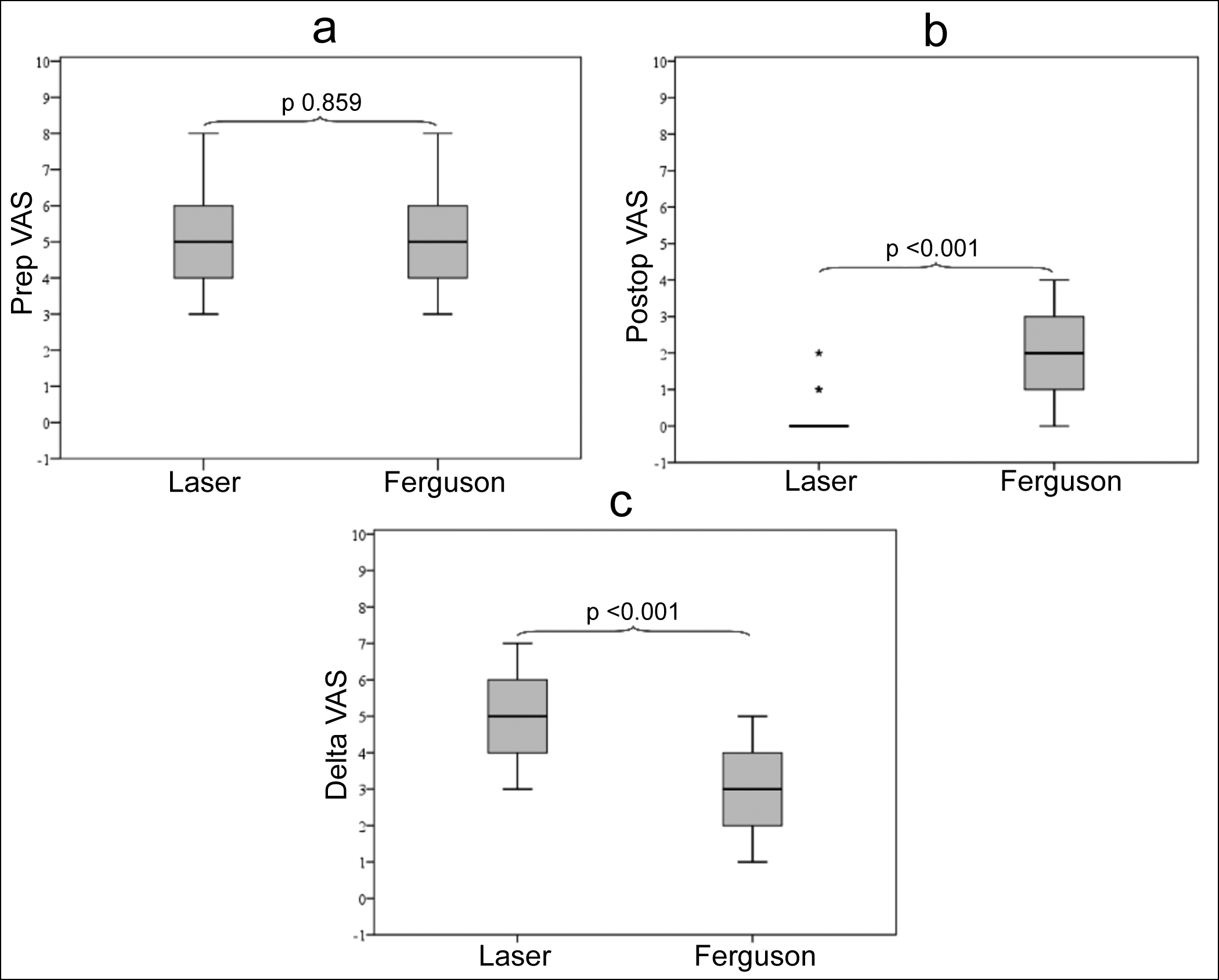 Figure 1: Box-plot of (a) preoperative, (b) postoperative, and (c) Δ VAS scores of the patients
Figure 1: Box-plot of (a) preoperative, (b) postoperative, and (c) Δ VAS scores of the patients
Although postoperative anal fistula was not observed in either surgical treatment group, all other complications were observed more frequently in the Ferguson group with a statistical similarity. The presence of any complication, on the other hand, was statistically significantly higher in FH than in LH (p=0.025). While only three patients in the FH group required surgical treatment for complications, the need for surgery due to complications was also statistically similar between the groups (Table II). Except for the complications requiring surgical treatment, the others improved with proper medical treatment.
DISCUSSION
Although there are several approaches in the management of HD including behavioural changes, and medical and surgical treatment modalities, the efficiency and safety of LH and FH were compared in grade III or grade IV HD patients. The demographics and baseline clinical characteristics of the patients were similar which means that the randomisation was proper. The median age was about 32.0 years, and four-fifths of the patients were women. While bleeding and dyschezia were seen in about half of the patients, the most of patients had involvement in one or two quadrants. Except for some variations, these features were comparable with other grade-III and grade-IV HD patient populations studied in the literature.1,2,4,15
To compare the success of the procedures between LH and FH, LOS, the number of excised lumps, wound healing time, and time to symptom relief after surgery were used. LH took less time with a similar number of excised lumps when compared to FH. Furthermore, the patients who underwent LH had statistically significantly faster-wound healing and symptom relief than patients in the FH group. LH had also better outcomes for pain relief and postoperative complications. Despite there being no published RCT aimed to compare non-excisional laser techniques and FH in HD patients, LH had lower operation time (ranging between 5 minutes and 40 minutes) and similar symptom resolution rates, and it was more effective in relieving pain when compared to open haemorrhoidectomy according to a recent systematic review conducted by Longchamp et al.14 However, Bhatti et al. included seven RCTs which compared open and closed haemorrhoidectomy procedures in their meta-analysis, and they reported that closed procedure had longer LOS with a pooled mean difference of 6.1 minutes and a significant heterogeneity which means that there may be several variations in the design of those studies.13 They also found that the closed technique had lower postoperative pain, less wound healing time, and reduced postoperative bleeding risk than open haemorrhoidectomy, however, the two procedures were similar in terms of postoperative complication rate, and recurrence.13
Naderan et al. carried out an RCT to compare the laser procedure with MMH in patients with grade II or III internal haemorrhoids and found that the mean LOS of the laser procedure and MMH were 33.1 minutes and 52.6 minutes, and the complete resolution rates of the two procedures were 70% and 76.7% (with no statistical significance), respectively.19 Alsisy et al. performed another RCT with grade II or III HD patients to compare diode laser coagulation with MMH, and reported that mean LOS was 30.6 minutes in the laser group and 50.5 minutes in the MMH group.20 The author also found that all patients underwent laser procedures and 90% of the MMH group had a complete symptom resolution within three months.20 Poskus et al. compared LH with sutured mucopexy and excisional haemorrhoidectomy in their RCT, and they found that the LOS of laser procedure was nearly half of excisional haemorrhoidectomy (15 minutes versus 29 minutes), the percentage of symptom-free patients was 72.5% for LH and 82.5% for excisional haemorrhoidectomy (with no statistical significance) within one year after surgery.21 Maloku et al. reported that the mean LOS was 15.9 minutes for LH and 27.2 minutes for MMH in their RCT conducted in patients with grade III HD.22 They also found that the mean recovery time was 17.2 days for LH, and 19.2 days for MMH.22 When compared to MMH, LH might have a higher risk of postoperative thrombosis, but other complications such as postoperative bleeding, urinary retention, anal discharge, anal stenosis, and the need for secondary surgery were similar.19,20 Although both these studies excluded grade IV HD patients, one RCT studied grade III and grade IV patients, but the authors preferred LH in grade III patients and open haemorrhoidectomy in grade IV patients.15 However, LH was efficiently applicable in grade IV patients in this study.
Many types of covariates can be associated with post-haemorrhoidectomy pain relief including using anaesthetic agents, choosing advanced surgical techniques like using an ultrasonic scalpel or a vascular sealing device, and intra- or postoperative interventions such as Botulinum toxin injection, using topical calcium channel blockers, and oral metronidazole.23-25 Above-mentioned additional interventions were not used to determine the precise effects of the two different methods on the outcomes of the study.
This study has several limitations. First, evaluating the one-week pain relief using VAS scores was not able to compare the mid- or long-term improvement in pain relief between the study groups. On the other hand, other surgical outcomes and the presence of complications were compared through a 60-day follow-up which can be accepted as a mid-term period. The last limitation was the relatively small sample size of this single-centre study which means that the study results could not be generalised to other patient populations suffering from haemorrhoids. Readers should consider these limitations when interpreting the results of the study.
CONCLUSION
LH might be an alternative treatment modality in patients admitted with grade III and grade IV haemorrhoids with a low level of complication rate. Further multi-centre clinical trials with relatively large study populations, using long-term outcomes of interest and evaluating the quality of life, postoperative analgesic usage, and patient satisfaction, should be performed to validate the results of this study.
ETHICAL APPROVAL:
Ethical approval was obtained from the Clinical Research Ethics Committee of Istanbul Medipol University (Approval Date 13.12.2021, No. E-10840098-772.02-6314).
PATIENTS’ CONSENT:
Written informed consents were obtained from all patients included in the study.
COMPETING INTEREST:
The author declared no competing interest.
AUTHOR’S CONTRIBUTION:
TM: Design of the study, surgical intervention, data collection, data analysis, and manuscript writing.
REFERENCES
- Sheikh P, Régnier C, Goron F, Salmat G. The prevalence, characteristics and treatment of hemorrhoidal disease: Results of an international web-based survey. J Comp Eff Res 2020; 9(17):1219-32. doi: 10.2217/cer-2020-0159.
- Riss S, Weiser FA, Schwameis K, Riss T, Mittlbock M, Steiner G, et al. The prevalence of hemorrhoids in adults. International J Colorectal Disease 2012; 27(2):215-20. doi: 10. 1007/s00384-011-1316-3.
- Peery AF, Sandler RS, Galanko JA, Bresalier RS, Figueiredo JC, Ahnen DJ, et al. Risk factors for hemorrhoids on screening colonoscopy. PLoS One 2015; 10(9):e0139100. doi: 10.1371/journal.pone.0139100.
- Hong YS, Jung KU, Rampal S, Zhao D, Guallar E, Ryu S, et al. Risk factors for hemorrhoidal disease among healthy young and middle-aged Korean adults. Sci Rep 2022; 12(1):129. doi: 10.1038/s41598-021-03838-z.
- De Schepper H, Coremans G, Denis MA, Dewint P, Duinslaeger M, Gijsen I, et al. Belgian consensus guideline on the management of hemorrhoidal disease. Acta Gastroenterol Belg 2021; 84(1):101-20. doi: 10.51821/84. 1.497.
- Gallo G, Martellucci J, Sturiale A, Clerico G, Milito G, Marino F, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): Management and treatment of hemorrhoidal disease. Tech Coloproctol 2020; 24(2): 145-64. doi: 10.1007/s10151-020-02149-1.
- Van Tol RR, Kleijnen J, Watson AJM, Jongen J, Altomare DF, Qvist N, et al. European Society of ColoProctology: Guideline for haemorrhoidal disease. Colorectal Dis 2020; 22(6):650-62. doi: 10.1111/codi.14975.
- Wald A, Bharucha AE, Limketkai B, Malcolm A, Remes-Troche JM, Whitehead WE, et al. ACG clinical guidelines: Management of benign anorectal disorders. Am J Gastroenterol 2021; 116(10):1987-2008. doi: 10.14309/ajg.0000 000000001507.
- Yamana T. Japanese practice guidelines for anal disorders I. Hemorrhoids. J Anus Rectum Colon 2017; 1(3):89-99. doi: 10.23922/jarc.2017-018.
- De Marco S, Tiso D. Lifestyle and risk factors in hemorrhoidal disease. Frontiers In Surgery 2021; 8:729166. doi: 10.3389/fsurg.2021.729166.
- Rubbini M, Ascanelli S. Classification and guidelines of hemorrhoidal disease: Present and future. World J Gastrointest Surg 2019; 11(3):117-21. doi: 10.4240/wjgs.v11.i3. 117.
- Mott T, Latimer K, Edwards C. Hemorrhoids: Diagnosis and treatment options. Am Fam Physician 2018; 97(3):172-9.
- Bhatti MI, Sajid MS, Baig MK. Milligan-morgan (open) versus ferguson haemorrhoidectomy (closed): A systematic review and meta-analysis of published randomized, controlled trials. World J Surg 2016; 40(6):1509-19. doi: 10.1007/ s00268-016-3419-z.
- Longchamp G, Liot E, Meyer J, Toso C, Buchs NC, Ris F. Non-excisional laser therapies for hemorrhoidal disease: A systematic review of the literature. Lasers Medical Science 2021; 36(3):485-96. doi: 10.1007/s10103-020-03142-8.
- Maloku H, Gashi Z, Lazovic R, Islami H, Juniku-Shkololli A. Laser hemorrhoidoplasty procedure vs open surgical hemorrhoidectomy: A trial comparing 2 treatments for hemorrhoids of third and fourth degree. Acta Informatica Med 2014; 22(6):365-7. doi: 10.5455/aim.2014.22.365- 367.
- Zahir KS, Edwards RE, Vecchia A, Dudrick SJ, Tripodi G. Use of the Nd-YAG laser improves quality of life and economic factors in the treatment of hemorrhoids. Conn Med 2000; 64(4):199-203.
- Elfallal AH, Fathy M, Elbaz SA, Emile SH. Comprehensive literature review of the applications of surgical laser in benign anal conditions. Lasers Med Sci 2022; 37(7): 2775-89. doi: 10.1007/s10103-022-03577-1.
- Ferguson JA, Heaton JR. Closed hemorrhoidectomy. Dis Colon Rectum 1959; 2(2):176-9. doi: 10.1007/BF02616713.
- Naderan M, Shoar S, Nazari M, Elsayed A, Mahmoodzadeh H, Khorgami Z. A randomized controlled trial comparing laser intra-hemorrhoidal coagulation and milligan-morgan hemorrhoidectomy. J Invest Surg 2017; 30(5):325-31. doi: 10.1080/08941939.2016.1248304.
- Alsisy A, Alkhateep Y, Salem I. Comparative study between intrahemorrhoidal diode laser treatment and Milligan-Morgan hemorrhoidectomy. Menoufia Med J 2019; 32(2): 560-5.
- Poskus T, Danys D, Makunaite G, Mainelis A, Mikalauskas S, Poskus E, et al. Results of the double-blind randomized controlled trial comparing laser hemorrhoidoplasty with sutured mucopexy and excisional hemorrhoidectomy. Int J Colorectal Dis 2020; 35(3):481-90. doi: 10.1007/s00384- 019-03460-6.
- Maloku H, Lazović R, Terziqi H. Laser hemorrhoidoplasty versus Milligan-morgan hemorrhoidectomy - short term outcome. Vojnosanitetski Pregled 2019; 76(1):8-12.
- Lohsiriwat V, Jitmungngan R. Strategies to reduce post-hemorrhoidectomy pain: A systematic review. Medicina (Kaunas) 2022; 58(3):418. doi: 10.3390/medicina580 30418.
- Huang YJ, Chen CY, Chen RJ, Kang YN, Wei PL. Topical diltiazem ointment in post-hemorrhoidectomy pain relief: A meta-analysis of randomised controlled trials. Asian J Surg 2018; 41(5):431-7. doi: 10.1016/j.asjsur.2017.06.002.
- Re AD, Toh JWT, Iredell J, Ctercteko G. Metronidazole in the management of post-open haemorrhoidectomy pain: Systematic review. Ann Coloproctol 2020; 36(1):5-11. doi: 10. 3393/ac.2020.01.08.