Comparing Crystallized Phenol and Surgical Excision Treatments in Pilonidal Sinus Disease
By Ali Gozukucuk1, Basri Cakiroglu2, Sefa Yapici3, Ilknur Banli Cesur4, Zerrin Ozcelik4, Hassan Huseyin Kilic5Affiliations
doi: 10.29271/jcpsp.2022.05.652ABSTRACT
Objective: To compare the results of commonly used treatments (Karydakis Flap method and crystallized phenol application) in the treatment of pilonidal sinus.
Study Design: Comparative study.
Place and Duration of Study: Adana Seyhan State Hospital, Adana City Hospital, and Hisar Intercontinental Hospital Pediatric Surgery Clinic, from January 2016 to December 2020.
Methodology: Patients who were treated for pilonidal Sinus and treated with surgical repair (karydakis flap method) and crystallized phenol method were included in the study. The efficacy and complications of both treatments were compared.
Results: Of the patients, 111 (34.7%) were treated with surgical repair, and 208 (65.3%) with the crystallized phenol method. Of the patients included in the study, 166 (52%) were male and 153 (48%) were female. The mean age was calculated as 15.5 (± 1.4). The mean hospital stay in the surgery group was 1.6 ± 0.4 days. The mean time to return to school was 2.8 ± 1.02 days in the phenol group and 12.3 ± 2.2 days in the Surgery group. Despite the third session of phenol application, recovery could not be achieved in 12 (5.7%) patients. Among those who had surgery, recurrence occurred in 7 (6.3%) patients and they had to be operated once more.
Conclusion: Crystallized Phenol application can be applied in uncomplicated cases due to high success, low complication, rapid recovery, early return to daily activities.
Key Words: Crystallized phenol, Surgical treatment, Pilonidal sinus disease.
INTRODUCTION
Pilonidal Sinus Disease (PSD) is an infectious and inflammatory disease of the sacrococcygeal area generally seen in young adults.1 Its onset is usually during adolescence. Although it is seen at an equal rate in men and women during adolescence, it is much more common in men than women after adolescence.2 It seems that being overweight, having a lot of hair, bad hygiene, and long sitting durations increase the risk of disease and recurrence.1,2 It is thought that PSD develops after the hair shed from skin gaps due to friction and pressure in the presacral area and passes under the skin.
The hair moving towards the subcutaneous tissue causes the formation of subcutaneous cysts. They may progress with infections that cause severe and purulent discharge in the intergluteal area. Patients frequently complain about pain, swelling, and the inability to sit on the coccygeal area.2 Symptoms such as repeating acute abscess and chronic suppuration can have significant effects on the quality of life, education, and social integration of the patients. The ideal treatment for this condition should have good recovery and recurrence rates while causing minimum disruption and discomfort. Hygiene and lifestyle are individual factors that affect the development of the disease, post-treatment recovery rates, and recurrence.1,3,4
Epilation could be recommended before the surgical treatment and crystallised phenol application. Not only does epilation eliminate the source of the disease, but also creates a clean workspace for the surgeon. Hair removal also decreases the risk of wound infections after crystallized phenol treatment.1,4,5 Additionally, washing the anogenital region with hot water after epilation is also recommended since it decreases the number of bacteria that can cause wound infections after the surgery.6
Table I: Surgical (KFR) and phenol (KFP) treatment data in pilonidal sinus cases.
|
Treatment groups |
M/F |
Age |
BMI |
Number of complications |
|
Group 1 (N=111) Surgery (KFR) |
68/43 |
15.58±1.42 |
20.67±2.33 |
9 (8.11% |
|
Group 2 (N=208) Phenol (KFP) |
98/110 |
15.52±1.36 |
21.10±2.77 |
10 (4.81%) |
|
p:0.684 |
p:0.165 |
p:0.001 |
||
Surgical and non-surgical treatment approaches are available; however, the optimal treatment is debatable.1-3 There are many reported approaches in the surgical treatment of PSD, ranging in complexity from simple drainage to intricately designed multi-flap closures.1
Today, the phenol application is starting to become popular due to being a minimally invasive treatment, being easily applied in adult age groups, and having good results. Phenol has antiseptic, anesthetic, and strong sclerosant properties. It is a white crystal solid at room temperature. It can become liquid at higher temperatures.7 The epithelium in the sinus is sclerosed with phenol.2 It was reported that there were smaller scars, less pain, faster wound healing, and early return to work when the Crystallised Phenol application was compared to Radical surgical excision.2,7 In this study, the aim was to compare the results of PSD treatment with surgical treatment (karydakis method), and with crystallised phenol treatment.
METHODOLOGY
A total of 319 patients who were treated for Pilonidal sinus in the Adana Seyhan Public Hospital, Adana City Hospital, and Hisar Intercontinental Hospital Pediatric Surgery between January 2016 and December 2020 were retrospectively evaluated. The data of the patients were accessed through the electronic medical record system. Gender and age, height and weight, (for BMI), number of phenol applications, anesthesia type, operation duration, drainage usage (number of days drained, drainage amount), post-operative hospital stay duration, the duration for returning to school or daily activities, postoperative complications, infections, hematoma, seroma and recurrence of all cases were retrospectively obtained from the records. The checkups of patients were also followed from the records. Patients who developed complications or had troubles in treatment were reached by phone and reevaluated. Systemic antibiotic treatment was given before surgery to patients who were admitted with an infection or abscess. The operation was performed after the infection improved.
The surgery duration was determined as the duration between the incision made with a scalpel and the last suture. The phenol application duration was defined as the duration starting from the beginning of the procedure by protecting the surrounding tissue with Nitrofurazone topical antibiotic cream, to closing it with a medical dressing. The duration of hospital stay was calculated from the day of surgery to the day of discharge. The polyclinic control duration and results of the patients were recorded.
The patients and their families chose the treatment method in this study. The advantages and disadvantages of both methods were told to the patients and their families and the choice was left to the families. There was no compulsion to prefer a particular method.
In both groups of patients, it was recommended to perform depilation (laser or topical creams) to the area approximately one month (4-8 weeks) before the operation, if possible, and for patients who could not perform this, to shave the entirety of the operation area one day before the surgery, if necessary. PSD patients aged 0-18 years were included in the study. Patients with previous PSD surgery and sacrococcygeal region anomalies were excluded.
Before the operation, the patients were informed about general or regional anesthesia according to the pre-operative evaluation of the anesthesia expert. The anesthesia method and post-operative analgesic method were decided on with the patients and their families. The operations were performed with; general anesthesia, spinal anesthesia, sedo-analgesic anesthesia or local anesthesia. Caudal block was applied for the purpose of post-operative analgesic, to patients who preferred caudal block. Intravenous (acetaminophen, tramadol, pethidine) analgesic method was applied to other patients. 05% bupivacaine hydrochloride was infiltrated intralesional and subcutaneously for local anesthesia. Thirty to sixty minutes before the operation, prophylaxis with cephazoline was applied to all patients. The procedure was performed in the prone position. The sacrococcygeal fascia was excised with an asymmetric ellipsoid incision, including all cystic formations in the midline, approximately 2 cm lateral to the intergluteal sulcus, including all pits in the gluteal region. If the midline defect was not suitable for primary closure, it was closed with an adipo-cutaneous flap prepared from the opposite side of the elliptical incision pole. The flap was sutured to the base and lateral tissues. A hemovac drainage was placed under the flap in all patients (the Karydakis method).8-10 The patients were hospitalised for 1 night because the postoperative pain may be excessive and close follow-up may be required. The patients who did not have excessive drainage from the drain were discharged by removing the drain. Absorbable PDS threads were preferred for subcutaneous sutures. The skin was closed with a vertical mat using a monofilament non-absorbable strip.
Prophylaxis was applied with 1. generation cephalosporin to all patients thirty to sixty minutes before the operation. The application was conducted in the operating room in the prone position under local anesthesia. The skin was cleaned with 10% povidone-iodine. The pits were identified. The pits that were clogged from granulation, fibrin, shed hair and other reasons, were opened with a fine-tip wedge and debrided with a curette. The sinus tract was identified with the help of a branule. Nitrofurazone topical antibiotic cream was applied to the surrounding tissue to protect the skin before the crystallized phenol application. As explained in the application of Dogru et al., the crystallised phenol was placed into the sinus with the help of a clamp. The phenol that was crystallized, quickly became liquid at body temperature and filled the sinus. Phenol was left in its place for approximately two minutes and then drained by pressing. The debris in the sinus was also drained. The process was performed a second time and drainage was done once again.7 The sinus area was neutralized with 70% ethanol. The process was terminated after the medical dressing and the patient was quickly discharged. The application area was checked on the 15th day of the procedure. A second application was not performed in cases that had epithelization in the PSD area. The second and third applications were performed after similar durations in patients who did not have epithelization with the same technique. More than three applications were not performed. Failure of the procedure was defined as non-epithelialized cases after three applications and recurring cases within three months. The application was performed by the same experienced surgical team (Figure 1).
The SPSS 25.0 (statistical package for social sciences, Chicago, USA) program was used in the statistical analysis of the data. Descriptive statistics were presented as mean ± standard deviation (mean ± SD) for continuous variables, and as numbers and percentages for categorical data. The data differences between the groups were analyzed with the student’s T-test (independent samples test) and Ki-Square test (chi-square tests). The value p<0.05 was accepted to be statistically significant.
RESULTS
Of the patients included in the study, 166 (52%) were male and 153 (48%) were female. The mean age was calculated as 15.5 ± 1.4 years. 111 (34.7%) patients were treated with surgical repair and 208 (65.3%) patients were treated with crystallised phenol method. The demographic and clinical characteristics of the patients are presented in Table I. The mean withdrawal time of the drains placed under the flaps in the surgical group was 1.2 days and the mean amount of drainage was 15.33 ml.
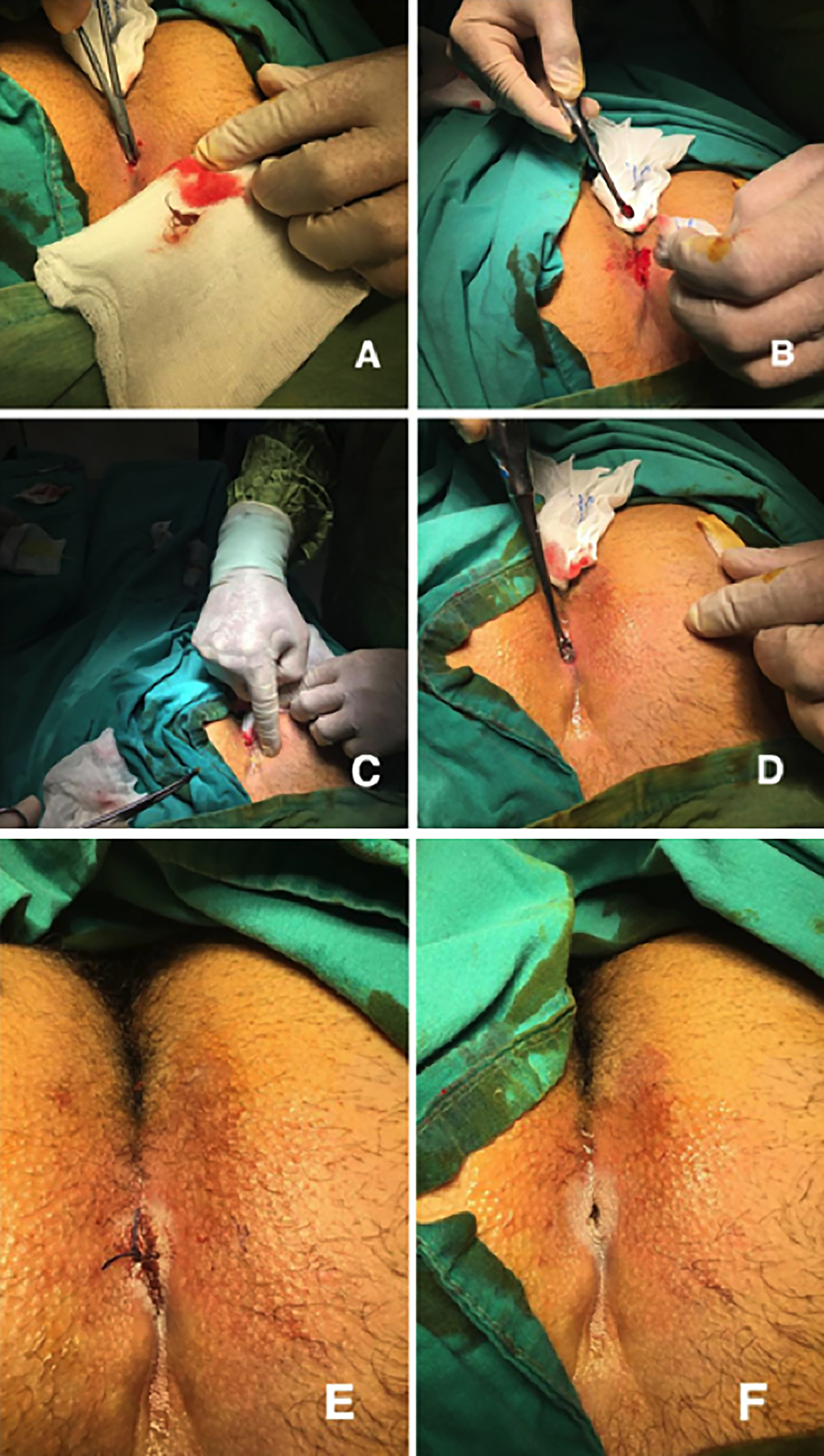 Figure 1: Crystallised phenol procedure.
Figure 1: Crystallised phenol procedure.
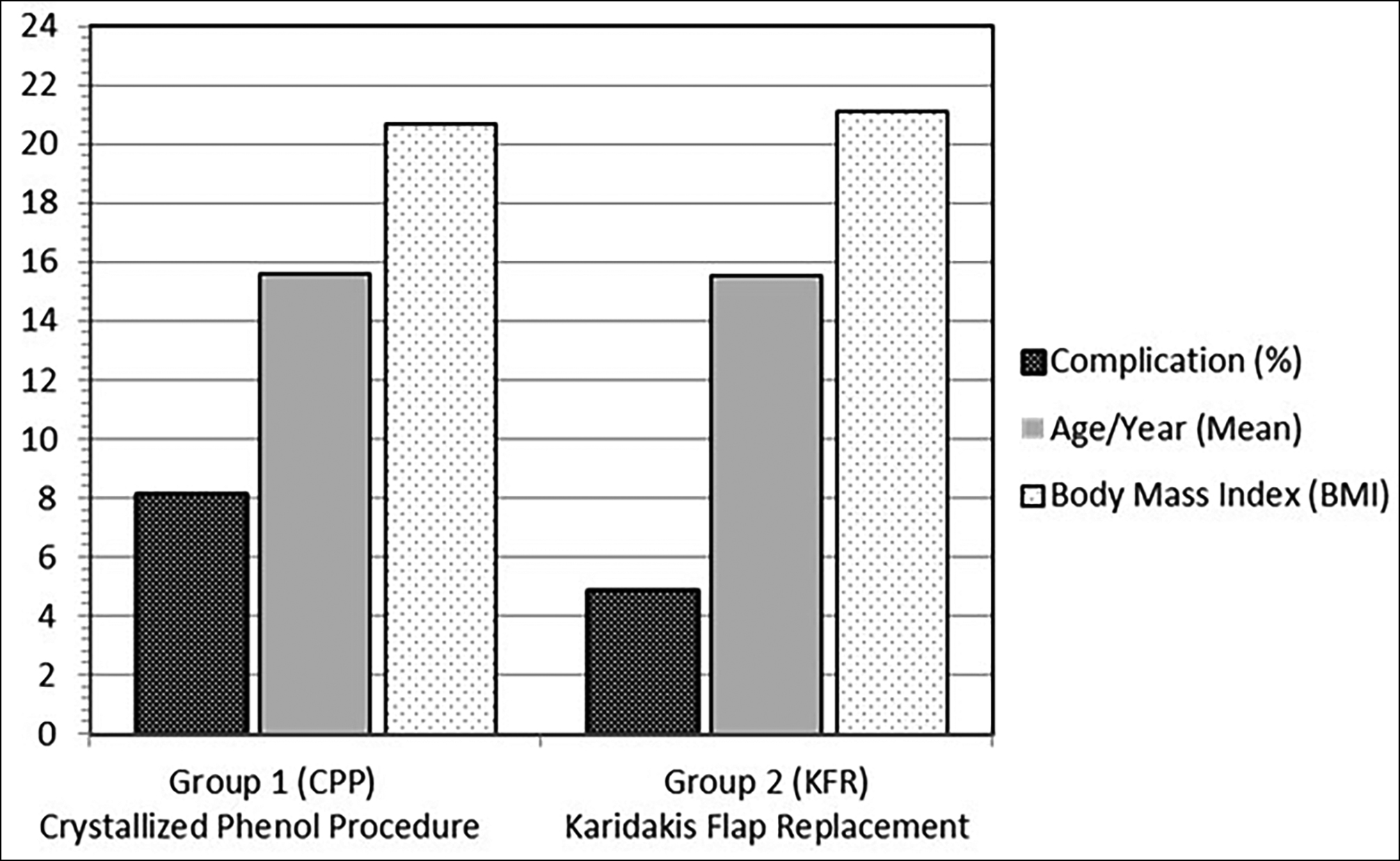 Figure 2: Complication percentages in treatment group in pilonidal sinus cases.
Figure 2: Complication percentages in treatment group in pilonidal sinus cases.
Complications such as wound infections, seroma, wound dehiscence, and hematoma were evaluated. Complications developed in 11 (9.9%) patients who underwent surgery and 12 (5.7%) patients who underwent phenol. Seven (30.4%) of 23 cases with BMI >25 were treated surgically. Complications developed in 8 (34.78%) of 23 cases with BMI >25. Complications developed in 12 (4.05%) of 296 patients with BMI <25. Complications developed in 19 (5.96%) of 319 cases with pilonidal sinus. Complications developed in 7 (50%) of 14 patients with both BMI >25 and hairy type (Figure 2) phenol group patients underwent day surgery and were not admitted to the hospital. The mean hospital stay in the surgery group was 1.6 ± 0.4 days. The mean time to return to school was 2.8 ± 1.02 days in the phenol group and 12.3 ± 2.2 days in the surgery group. After the first phenol injection session, a second session was required in 32 (15.35%) patients. The complaints of 16 (7.6%) patients continued after the second session. At the end of the third session, four patients completely recovered with phenol treatment. Twelve (5.7%) patients did not improve despite multiple sessions of phenol application. Recurrence occurred in 7 (6.3%) patients in the surgical group. The mean follow-up period was 12.56 (11-16) months in the surgical group and 14.52 (10-18) months in the phenol group.
DISCUSSION
PSD is a chronic inflammatory disease. It is not rarely seen in children and its onset is often during adolescence.1 PSD can decrease quality of life and can cause morbidities in different degrees.1,11,12 Thus, PSD treatment and management in children are important. The ideal treatment to be preferred in PSD should be simple and effective. The short period of hospital stays, less need for analgesic, low complication rates, quick recovery, return to school or daily activities in a short time, low recurrence rates, and least scar tissue should be targeted.1-3,5 The existing treatment methods cannot meet all expectations.1 Different surgical methods are frequently used. Excision and primary repair have been preferred for years in uncomplicated cases due to their low recurrence rates and easy application technique. We used the Karydakis method, which is an excision and primary closure technique, in our patients in the Surgical group.8-10,13
Phenol has antiseptic, anesthetic, and strong sclerosant properties.7,11,12 Liquid or crystallised phenol can be used in PSD treatment. In our study, crystallized phenol was used due to concerns such as high rates of fat necrosis, damage to surrounding tissue, and the quick diffusion of liquid phenol to healthy tissues.8,14
PSD affects young men more; it is rarely seen under the age of 12 and over the age of 40 years.1,12,13 The highest incidence is detected in the 15-24 years age group.15 In this study, 52% of the patients were male with the mean age was 15.5 ± 1.4 years. This was consistent with the literature.1,2
The treatment of PSD with crystallised phenol has less peri operative pain and shorter post-operative rest duration compared to surgical treatment methods. There is no need to stay at the hospital since the patients can return to daily activities after the procedure.6 Similarly, in this study shorter hospital stays duration and shorter time to return to school and similar activities in the crystallised phenol group after the procedure were found.
Reviewing the minimal invasive procedures performed in the treatment of PSD in terms of surgery length, it is shorter compared to surgical methods with flaps. Pronk et al. reported in their research that the respective average procedure duration of patients treated with phenol was 18.6 ± 6.8 minutes, and 33 (± 3) minutes in surgical technique.16 In this study, we found the average procedure duration of each application as 12.42 +2.6 minutes in the phenol group and 39.40 ± 8.32 minutes in the surgical group. The procedure duration was significantly shorter in the crystallised phenol group than in the surgical group.
One of the most important advantages of minimally invasive procedures in PSD treatments is the duration of hospital stay. In the crystallised phenol application, patients are treated without staying at the hospital. Gurer et al. reported in their study that the average duration of hospital stay in patients treated with the Karydakis method is four days.17 In this study, the average duration of hospital stay in the surgical group was 1.6 ± 0.4 days. Patients in the group that was treated with crystallised phenol received day-case treatment. The duration to return to daily life and activities such as school are other important parameters to consider in PSD treatment.
Routine cavity drainage is recommended to reduce the risk of seroma, hematoma, abscess, wound dehiscence, and infection in surgical methods with flaps applied in PSD.17 Studies have reported that 2.4% of the patients developed seroma after drainage.18 Yıldız et al. reported 1.55% seroma in their study.19 In the present study, a drain was placed under the flap in patients in the surgical group who could not be primarily closed and the flap was turned. In this group, seroma developed in 3 (2.7%) patients, and hematoma developed in 4 (3.6%) patients. When compared with the literature, the seroma and hematoma rates in our study were similar to the literature.18,19
In studies evaluating crystallized phenol treatments, the rate of developing one or more complications is reported to be 0%-16%.1,2,12,20 In this case series, the complication rate was 8.11% in the surgical group and 4.81% in the crystallised phenol group. More complications were seen in the surgical group than in the phenol group.
The overall combined risk of recurrence rate for excision and non-midline primary closure is 6% (1-15%).12 The recurrence rates for patient series related to Karydakis flap method is reported as 4.6-2.4%.8,20 The surgical removal of all sinuses and closure of the cavity with a flap brings surgical risks along with low recurrence rates. The crystallized phenol application is an effective treatment option with low recurrence rates.6 Stauffer et al. reported that recurrence rates increased to 1.6% in 12 months for non-midline closure and to 6.7% in 10 years in adults.21 In their study, Hardy et al. reported an 8% recurrence rate after non-midline closure in children with a median follow-up of only 25.5 months.12 Excision and secondary recovery were found to have the worst average recurrence risk in children (26%), while in adults this procedure had the best recurrence rates (1.5% at 12 months and 13% at 5 years). In this study, the recurrence rate in the surgical group was 6.3%, similar to the literature. In studies recommending the use of PSD phenol, the success of the treatment is reported between 59% and 95.1%.1,2,12 In those that were unsuccessful, phenol can be applied again, Girgin et al. reached a 64.5% recovery rate after one phenol application, and 95% recovery with two or more applications.22
In this study, the recurrence rate after all applications was 6.3% in the surgical group and 5.7% in the phenol group.
In the phenol group patients, more than one session of phenol injection was necessary for 32 patients. Complete recovery was achieved in 20 (9.6%) patients with multiple phenol applications.
There are different studies explaining the relationship between PSD, BMI, and hairy body types. It is stated that high BMI is an important risk factor for more complications and recurrence.23,24 In a study, operative time, average hospital stay, and postoperative complications were found to be higher in obese patients compared to non-obese patients.8 In this study, 7 (30.4%) of 23 patients with BMI >25 Kg/m2 were treated with PSD surgically. Complications developed in 8 (34.78%) of 23 cases with BMI >25 Kg/m2. Complications developed in 12 (4.05%) of 296 cases with BMI <25 Kg/m2. Complications developed in 19 (5.96%) of 319 patients with pilonidal sinus. Complications developed in 7 (50%) of 14 patients with both BMI >25 and hairy type. Therefore, if the body is hairier than normal and the BMI is higher than 25, the rate of complication development is clearly high. While the complication rate was 5.96% in the complete series, it increased to 50% in hairy patients and those with BMI higher than 25 Kg/m2.
Although it is a large series showing the application of crystallised phenol, which is one of the minimally invasive methods, with surgical treatment used in PSD treatments. The major limitation is that it is a retrospective study so postoperative pain could not be fully evaluated. Another limitation is that cosmetic satisfaction of the patient according to positive criteria could not be evaluated.
CONCLUSION
Regarding surgical treatment and phenol treatments in PSD in young age groups, the phenol application can be performed on selected cases with high success, low complications, hospitalisation, and early return to activities such as schooling.
ETHICAL APPROVAL:
The study protocol approval was given by the Adana City Hospital Ethic Committee on 06.05.2021. The institutional review board (IRB) No. 80/1387.
PATIENT’S CONSENT:
Written consent was given by the patients and their families to use their surgical images.
COMPETING INTERESTS:
The authors declared no competing interests.
AUTHORS' CONTRIBUTION:
AG, BC, SY, IBC: Designed the study, collected data, wrote the article, and conducted the literature review.
ZO: Designed the study, collected data, wrote the article, and conducted the literature review.
HHK: Designed the study, collected data, wrote the article, and conducted the literature review.
REFERENCES
- Grabowski J, Oyetunji TA, Goldin AB, Baird R, Gosain A, Lal DR, et al. The management of pilonidal disease: A systematic review. J Pediatr Surg 2019; 54(11):2210-21. doi: 10.1016/j.jpedsurg.2019.02.055.
- Ates U, Ergun E, Gollu G, Sozduyar S, Kologlu M, Cakmak M, et al. Pilonidal sinus disease surgery in children: the first study to compare crystallized phenol application to primary excision and closure. J Pediatr Surg 2018; 53(3):452-5. doi: 10.1016/j.jpedsurg.2017.05.012.
- Sit M, Aktas G, Yilmaz EE. Comparison of the three surgical flap techniques in pilonidal sinus surgery. Am Surg 2013; 79(12):1263-8.
- Mutus HM, Aksu B, Uzun E, Gulcin N, Gercel G, Ozatman E, et al. Long-term analysis of surgical treatment outcomes in chronic pilonidal sinus disease. J Pediatr Surg 2018; 53(2):293-4. doi: 10.1016/j.jpedsurg.2017.11.031.
- Halleran DR, Onwuka AJ, Lawrence AE, Fischer BC, Deans KJ, Minneci PC. Laser hair depilation in the treatment of pilonidal disease: A systematic review. Surg Infect (Larchmt) 2018; 19(6):566-72. doi: 10.1089/sur.2018.099.
- Yuksel ME. Pilonidal sinus disease can be treated with crystallised phenol using a simple three-step technique. Acta Dermatovenerol Alp Pannonica Adriat 2017 Mar; 26(1): 15-7. doi: 10.15570/actaapa.2017.4.
- Dag A, Colak T, Turkmenoglu O, Sozutek A, Gundogdu R. Phenol procedure for pilonidal sinus disease and risk factors for treatment failure. Surgery 2012; 151(1):113-7. doi: 10.1016/j.surg.2011.07.015.
- Sakr M, El-Hammadi H, Mousa M, Arafa S, Rasheed M. The effect of obesity on the results of Karydakis technique for the management of chronic pilondal sinus. Int J Colorectal Dis 2003; 18(1):36-9. doi: 10.1007/s00384-002-0407-6.
- Smith CM, Jones A, Dass D, Murthi G, Lindley R. Early experience of the use of fibrin sealant in the management of children with pilonidal sinus disease. J Pediatr Surg 2015; 50(2):320-2. doi: 10.1016/j.jpedsurg.2014.11.022.
- Zagory JA, Golden J, Holoyda K, Demeter N, Nguyen NX. Excision and primary closure may be the better option in the surgical management of pilonidal disease in the pediatric population. Am Surg 2016; 82(10):964-7.
- Dogru O, Camci C, Aygen E, Girgin M, Topuz O. Pilonidal sinus treated with crystallized phenol: An eight-year experience. Dis Colon Rectum 2004; 47(11):1934-8. doi: 10. 1007/s10350-004-0720-y.
- Hardy EJO, Herrod PJ, Doleman B, Phillips HG, Ranat R, Lund JN. Surgical interventions for the treatment of sacrococcygeal pilonidal sinus disease in children: A systematic review and meta-analysis. J Pediatr Surg 2019; 54(11): 2222-33. doi: 10.1016/j.jpedsurg.2019.02.058.
- McCallum IJD, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: Systematic review and meta-analysis. BMJ 2008; 336:868-71. doi.org/10.1136/bmj.39517.808160.BE.
- Kayaalp C, Olmez A, Aydin C, Piskin T, Kahraman L. Investigation of a one-time phenol application for pilonidal disease. Med Princ Pract 2010; 19(3):212-5. doi: 10.1159/000 285291.
- Keighley MRB. “Pilonidal sinus,” in Surgery of the Anus Rectum and Colon, M. R. B. Keighley and N. Williams, Eds., pp.1999;2nd edition. London, UK.
- Pronk AA, Smakman N, Furnee EJB. Short-term outcomes of radical excision vs. phenolisation of the sinus tract in primary sacrococcygeal pilonidal sinus disease: A randomised-controlled trial. Tech Coloproctol 2019; 23(7):665-73. doi: 10.1007/s10151-019-02030-w.
- Gurer A, Gomceli I, Ozdogan M, Ozlem N, Sozen S, Aydin R. Is routine cavity drainage necessary in Karydakis flap operation? A prospective, randomised trial. Dis Colon Rectum 2005; 48(9):1797-9. doi: 10.1007/s10350-005-0108-7.
- Bessa SS. Results of the lateral advancing flap operation (modified Karydakis procedure) for the management of pilonidal sinus disease. Dis Colon Rectum 2007; 50(11):1935-40. doi: 10.1007/s10350-007-9049-7.
- Yildiz MK, Ozkan E, Odabaşı HM, Kaya B, Eriş C, Abuoğlu HH, et al. Karydakis flap procedure in patients with sacrococcygeal pilonidal sinus disease: Experience of a single centre in Istanbul. Scientific World J 2013; 2013:807027. doi: 10. 1155/ 2013/807027.
- Can MF, Sevinc MM, Yilmaz M. Comparison of karydakis flap reconstruction versus primary midline closure in sacrococcygeal pilonidal disease: Results of 200 military service members. Surgery Today 2009; 39(7):580-6. doi: 10.1007/ s00595-008-3926-0.
- Stauffer VK, Luedi MM, Kauf P, Schmid M, Diekmann M, Wieferich K, et al. Common surgical procedures in pilonidal sinus disease: A meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep 2018; 8(1):3058. doi.org/10. 1038/s41598-018-20143-4.
- Girgin M, Kanat BH, Ayten R, Cetinkaya Z, Kanat Z, Bozdag A, et al. Minimally invasive treatment of pilonidal disease: Crystallised phenol and laser depilation. Int Surg 2012; 97(4):288-92. doi: 10.9738/CC130.1.
- Bayhan Z, Zeren S, Duzgun SA, Ucar BI, Alparslan Yumun HN, Mestan M. Crystallized phenol application and modified Limberg flap procedure in treatment of pilonidal sinus disease: A comparative retrospective study. Asian J Surg 2016; 39(3):172-7. doi: 10.1016/j.asjsur.2015.12.007.
- Arda IS, Guney LH, Sevmiş S, Hicsonmez A. High body mass index as a possible risk factor for pilonidal sinus disease in adolescents. World J Surg 2005; 29(4):469-71. doi: 10.1007/s00268-004-7533-y.