Bilateral Temporomandibular Joint Dislocation Following Arthrocentesis Plus Hyaluronic Acid Injection
By Sadi Memis1, Mert Can2Affiliations
doi: 10.29271/jcpsp.2022.05.677ABSTRACT
Arthrocentesis plus intra-articular hyaluronic acid (HA) injection for temporomandibular joint (TMJ) disorders is known to be a safe and minimally invasive surgical procedure. Arthrocentesis plus HA injection has a pain-reducing effect on TMJ disorders. It is also a palliative treatment that yields positive results in terms of clinical findings such as clicking and mouth opening. Even though some complications have been reported after the performance of this highly successful procedure, the development of bilateral TMJ dislocation after arthrocentesis plus intra-articular HA injection has not been reported to date. This case report presents bilateral TMJ dislocation following arthrocentesis plus intra-articular HA injection that developed within a few hours and resisted manual Hippocrates manoeuvre in a 21-year male. Herein, his treatment with systemic corticosteroid therapy, myorelaxant and anti-inflammatory drugs is also presented.
Key Words: Arthrocentesis, Hyaluronic acid, Joint dislocation, Temporomandibular joint, Steroids.
INTRODUCTION
Temporomandibular joint (TMJ) dislocation is defined as a condition in which the condyle head moves out of the glenoid fossa beyond the articular eminence without descending back to its normal position spontaneously.1
Arthrocentesis plus intra-articular hyaluronic acid (HA) injection is a minimally invasive treatment option for TMJ disorders. This treatment provides a pain-reducing effect and yields positive results in terms of clinical findings such as larger mouth opening.2 Although many complications have been reported after arthrocentesis plus intra-articular HA injection3, there has been no case of TMJ dislocation to date. We aimed to present a rare complication of bilateral TMJ dislocation following this procedure and its treatment with systemic corticosteroids.
CASE REPORT
A 21-year male patient was referred to our clinic for the first time in 2018 with complaints of restricted mouth opening, moderate pain, and nocturnal bruxism.
In the clinical examination, the maximum inter-incisal mouth opening (MIO) was 38 mm and bilateral disc displacement with reduction of TMJ was observed on MRI. Upper jaw occlusal splint therapy was started as a conservative treatment. However, the patient admitted that he did not conscientiously use his splint. Upon periodic recurrence of the patient’s complaints, arthrocentesis plus HA was performed twice in November 2018 and January 2019. After about one year, the patient experienced a decrease in complaints and an increase in mouth opening. In January 2020, when he returned with a complaint of severe pain in the TMJ region and the feeling of being stuck in the joint area, the MIO was measured, and it was found to be 44 mm. Arthrocentesis plus HA injection was planned once more for the patient under local anaesthesia to remove any inflammatory mediators that could be causing persistent joint pain. The patient’s skin surface was disinfected and the needle entry locations for TMJ arthrocentesis defined by Laskin4 were localised. Articaine (Ultracain D-S Forte, Aventis, Istanbul, Turkey) with a ratio of 1:100,000 epinephrine was applied as local anaesthesia. Arthrocentesis was performed without any problem using 100 mL Ringer’s lactate solution using two 22-gauge needles separately for both joints. Injection of HA (Hyalgan, Fidia Farmaceutici SpA, Abano Terme, Italy) following arthrocentesis was performed in both joints uneventfully. After the procedure, the patient did not experience any complications until he left the hospital. The next day, when the patient came back to the clinic for follow-up, open bite, pain, and anxiety were detected. It was observed that the class I normal occlusion of the patient changed to class III malocclusion with anterior negative overjet. The patient explained that about 2 hours after the procedure, he had been unable to close his chin and bring his teeth to occlusion. In addition, he mentioned that the situation had developed slowly. Based on TMJ dislocation definition, displacement of the bilateral condyles from the glenoid fossa beyond the articular eminence was detected on the TMJ radiograph (Figure 1). Thereafter, local anaesthesia was performed bilaterally in the TMJ region. The Hippocrates manoeuvre was attempted to replace the condyles, but it was not successful. It was thought that persistent TMJ dislocation due to possible effusion had developed in the TMJ. The patient was prescribed systemic corticosteroids with decreasing doses at consecutive days, namely, 40 mg methylprednisolone (MP) intramuscularly on the first day, 20 mg MP intramuscularly on the second day and 16 mg MP orally on the following three days reduced by half every day. Non-steroidal anti-inflammatory drugs (NSAIDs) (100 mg diclofenac) and myorelaxant (2 mg tizanidine hydrochloride) were also prescribed for oral administration for 5 days. The patient was advised to avoid trauma and to be fed a liquid-soft diet. The patient’s excessive class III malocclusion decreased to anterior tête-à-tête occlusion within two days. It was observed that the patient had normal occlusion before the procedure on the fifth day.
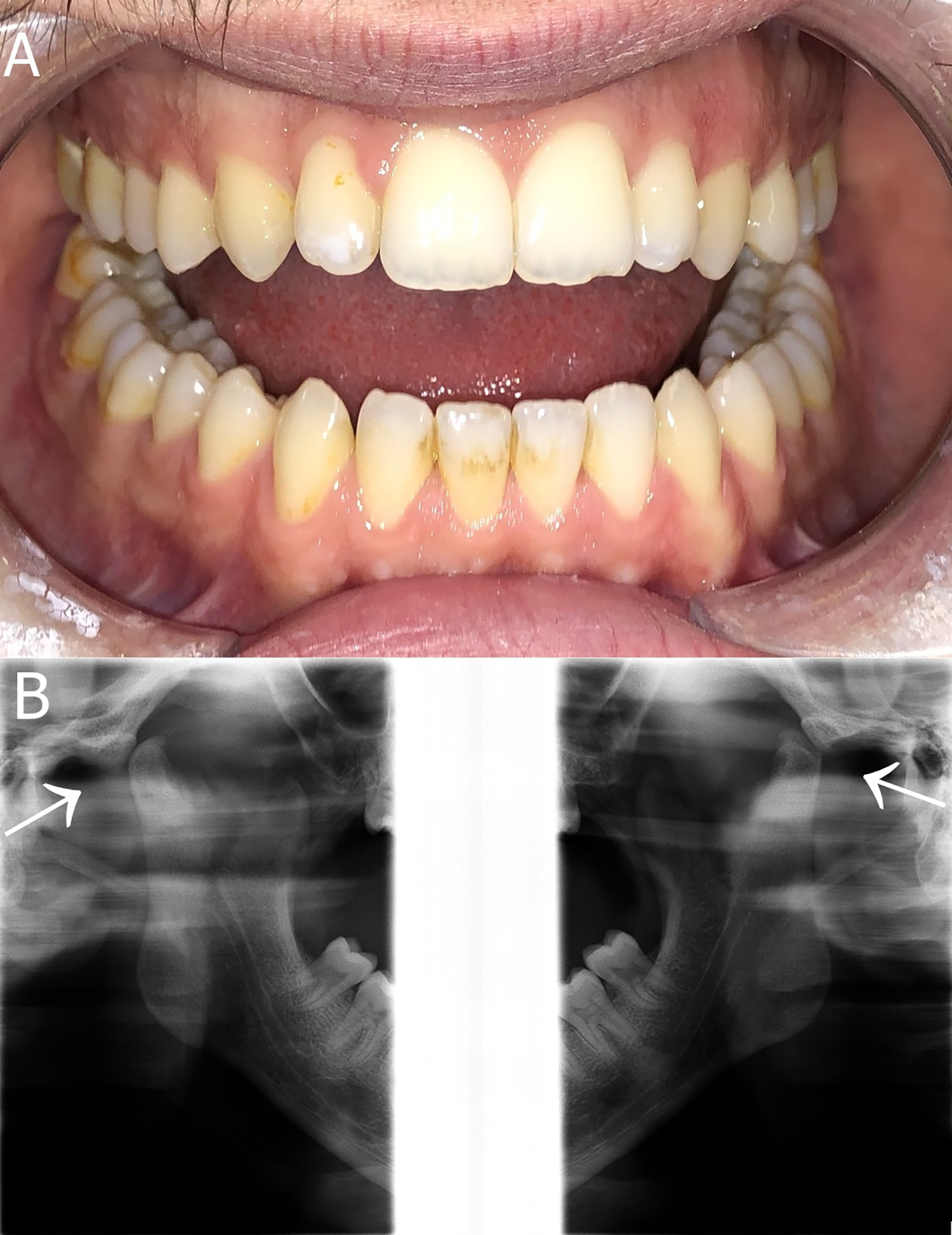 Figure 1: Initial clinical and radiographic findings of the patient after the complication developed. (A) Malocclusion (open bite) is observed. (B) TMJ radiograph showing that the position of the condyle heads is beyond the articular eminences (white arrows), a feature that is compatible with bilateral TMJ dislocation.
Figure 1: Initial clinical and radiographic findings of the patient after the complication developed. (A) Malocclusion (open bite) is observed. (B) TMJ radiograph showing that the position of the condyle heads is beyond the articular eminences (white arrows), a feature that is compatible with bilateral TMJ dislocation.
After five days, MRI detected normal findings. TMJ distances and surfaces were viewed regularly. Panoramic radiograph indicated that the condyle had spontaneously returned to its position in the glenoid fossa (Figure 2).
Within two weeks, MIO was measured and was 47 mm. In the three-month follow-up, clicking and pain in the TMJ and masticating muscles disappeared completely.
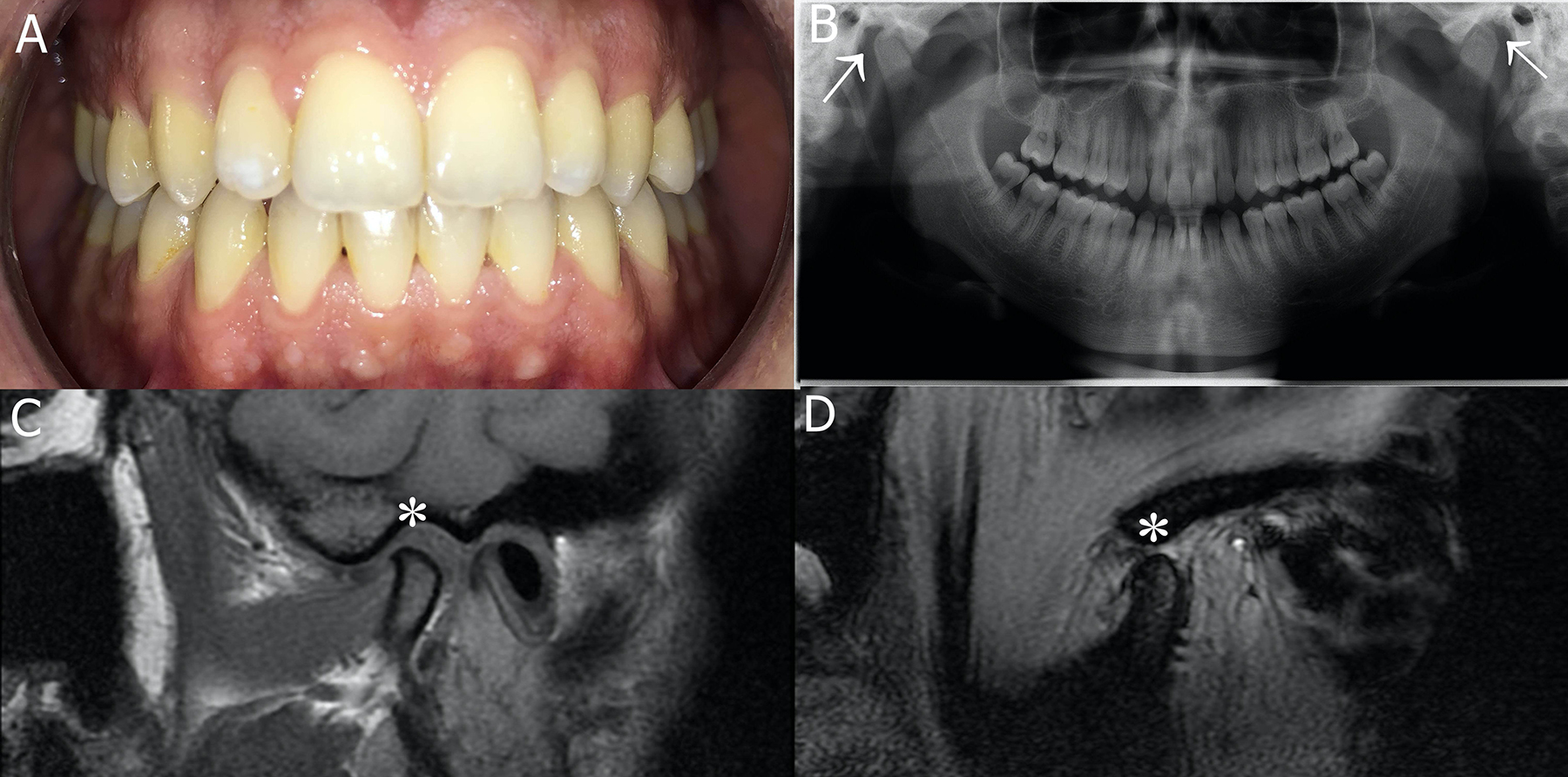 Figure 2: Clinical and radiographic findings of the patient after treatment. (A) Malocclusion improved after medication. (B) Panoramic radiograph showing that the condyle heads reached their positions (white arrows) in the glenoid fossa bilaterally. (C) In the closed mouth position, the MRI indicates that the right TMJ condyle and disc show correct position (white star) and normal relationship. (D) In the open mouth position, the MRI shows that the right TMJ condyle and disc are in the correct position (white star) with a normal relationship.
Figure 2: Clinical and radiographic findings of the patient after treatment. (A) Malocclusion improved after medication. (B) Panoramic radiograph showing that the condyle heads reached their positions (white arrows) in the glenoid fossa bilaterally. (C) In the closed mouth position, the MRI indicates that the right TMJ condyle and disc show correct position (white star) and normal relationship. (D) In the open mouth position, the MRI shows that the right TMJ condyle and disc are in the correct position (white star) with a normal relationship.
DISCUSSION
Various conservative approaches, such as occlusal splint therapy, physical therapy and pharmacotherapy, can be applied initially for the treatment of TMJ disorders. In some cases, where these fail or are not effective, minimally invasive surgical procedures such as arthrocentesis and intra-articular HA injection are performed.
Heo et al.5 reported that arthrocentesis cannot directly prevent mechanical stress and intra-articular pressure in patients with bruxism. With this viewpoint, this patient’s treatment was started with occlusal splint therapy. However, success could not be achieved as the patient had not used the splint regularly. To ensure the stabilisation of TMJ and nutrition of the joint space, the patient was administered arthrocentesis and HA injection.
In this case, the procedure was performed using the arthrocentesis entry points defined by Laskin.4 However, there are various arthrocentesis modifications used in the literature,5,6 and the preferred choice is based on the characteristics of the cases.
The use of intra-articular HA injection with arthrocentesis was first introduced by Kopp et al.7 Subsequently, clinical studies have been reported showing that arthrocentesis plus HA injection yields more successful clinical results than arthrocentesis alone.2 Arthrocentesis is believed to have between 70% and 90% success rate in reducing pain and improving joint function.3 Although it has low morbidity, some complications may occur. Some of these complications have been reported in the literature, namely, nerve damage, local swelling, temporary ipsilateral open bite, otological injuries, periauricular hematoma, arterial aneurysm and injury, transarticular perforation, intracranial perforation, extradural hematoma, intra-articular hemarthritis, bacterial infection and tool breakage in the joint.3 However, the development of TMJ dislocation after this treatment procedure has not been previously reported.
In this case, there was no noticeable extraoral swelling after arthrocentesis plus HA injection. It was thought that due to intra-articular effusion and increased pressure, the condyle head went beyond the articular eminence, which caused it to become dislocated. The reason for the failure of the Hippocrates manoeuvre was similarly attributed to effusion and increased intra-articular pressure. Evidence has been previously reported indicating that an abnormal relationship between the joint disc position and morphology can lead to joint effusion findings.8 Conversely, effusion can also lead to improper relations of joint components and structures. The patient had a pretreatment mouth opening of 44 mm, and arthrocentesis usually increases the mouth opening further. Therefore, it is possible that the patient yawned and the TMJ dislocation occurred.
Vaira et al.3 reported that after arthrocentesis, there is an increase in joint vertical size caused by the expansion of the upper joint space. Therefore, an ipsilateral open bite table may develop. Intra-articular fluid drainage of the TMJ is not carried out rapidly due to its anatomical structure. In this case, prescribing systemic corticosteroids and NSAIDs caused the condition to regress within a few days due to their anti-inflammatory effects. The prescription of myorelaxant aimed to prevent a possible disc displacement or the condyle not returning to the glenoid fossa as a result of possible lateral pterygoid muscle contraction. It was also aimed to prevent myospasms in other chewing muscles during the period when occlusion cannot be achieved.
Corticosteroids are used to treat pain, trismus and swelling and suppress inflammatory reactions and inhibit enzyme phospholipase A2. They reduce the release of arachidonic acid at the inflammatory site. Furthermore, leukotrienes, prostaglandin synthesis and neutrophil accumulation are reduced.9
Various surgical and non-surgical treatments have been reported for the treatment of dislocations. Bayoumi et al. suggested starting less invasive treatment options before applying more invasive surgical approaches for the effective treatment of dislocations.10 Since the present patient did not have any structural disorders, the non-surgical pharmacotherapy approach was preferred as a first treatment option.
In conclusion, it was observed that the use of systemic corticosteroids, myorelaxant and anti-inflammatory medication yielded positive results in the treatment of bilateral TMJ dislocation, which is a rare complication of arthrocentesis plus HA injection. In order to prevent this complication, it is recommended that caution be applied so as not to create excessively high pressure inside the joint during the arthrocentesis procedure and to slowly infuse HA into the joint.
PATIENT’S CONSENT:
Informed consent was obtained from the patient.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
SM: Drafting the work and writing.
MC: Literature search.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Stolbizer F, Saiegh J, Andrada MM. Anterior dislocation of the temporomandibular joint: A simplified non-traumatic manual technique. J Man Manip Ther 2020; 28(4):246-50. doi: 10.1080/10669817.2019.1704516.
- Yilmaz O, Korkmaz YT, Tuzuner T. Comparison of treatment efficacy between hyaluronic acid and arthrocentesis plus hyaluronic acid in internal derangements of temporo-mandibular joint. J Cranio-Maxillofacial Surg 2019; 47(11): 1720-7. doi: 10.1016/j.jcms.2019.07.030.
- Vaira LA, Raho MT, Soma D, Salzano G, Dell’aversana Orabona G, Piombino P, et al. Complications and post-operative sequelae of temporomandibular joint arthrocentesis. Cranio - J Craniomandib Pract 2018; 36(4): 264-7. doi: 10.1080/08869634.2017.1341138.
- Laskin DM. Needle placement for arthrocentesis. J Oral Maxillofac Surg 1998; 56(7):907. doi: 10.1016/S0278- 2391(98)90043-X.
- Heo HA, Yoon HJ. Clinical outcomes of patients with bilateral anterior disc displacement without reduction and erosive change of the temporomandibular joint after performance of unilateral arthrocentesis and stabilisation splint therapy. J Oral Rehabil 2020; 47(3):307-12. doi: 10.1111/joor.12897.
- Alkan A, Baş B. The use of double- needle canula method for temporomandibular joint arthrocentesis: Clinical report. Eur J Dent 2007; 01(03):179-82. doi: 10.1055/s-0039- 1698335.
- Kopp S, Wenneberg B, Haraldson T, Carlsson GE. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction. J Oral Maxillofac Surg 1985; 43(6):429-35. doi: 10.1016/S0278-2391(85)80050-1.
- Pasqual PGV, Poluha RL, Setogutti ÊT, Grossmann E. Evaluation of effusion and articular disc positioning after two different arthrocentesis techniques in patients with temporomandibular joint disc displacement without reduction. Cranio - J Craniomandib Pract 2020; 38(4): 256-63. doi: 10.1080/08869634.2018.1511266.
- Koçer G, Yuce E, Tuzuner Oncul A, Dereci O, Koskan O. Effect of the route of administration of methylprednisolone on oedema and trismus in impacted lower third molar surgery. Int J Oral Maxillofac Surg 2014; 43(5):639-43. doi: 10.1016/j.ijom.2013.11.005.
- Bayoumi AM, Al-Sebaei MO, Mohamed KM, Al-Yamani AO, Makrami AM. Arthrocentesis followed by intra-articular autologous blood injection for the treatment of recurrent temporomandibular joint dislocation. Int J Oral Maxillofac Surg 2014; 43(10):1224-8. doi: 10.1016/j.ijom.2014. 05.004.