Avoiding “COVID Blindness”: Advocating Cognitive Bias Teaching in the Context of COVID-19
By Fenghua Qian1, Meina Zheng2, Jian Jiao2Affiliations
doi: 10.29271/jcpsp.2023.05.594
Sir,
The global pandemic of COVID-19 placed enormous pressure on the general population and healthcare systems due to its variability, unpredictability and highly contagious in recent years. This challenge created a context ripe for clinical reasoning and decision-making errors involving both systems and cognitive factors. The term COVID blindness has been recently used to define this issue.1
The study on cognitive bias in clinical reasoning during the epidemic of COVID-19 are scarce. Lucas et al. examined the frequency and causes for patients upgraded to intensive care unit (ICU) following admission from the emergency department (ED) to non-critical care units.2 Results showed that the percentage of upgraded cases with non-concordant diagnoses increased from a baseline range of 14–20% to 41.3%, the majority of upgrades were due to premature closure (72.2%), anchoring (61.1%), and confirmation bias (55.6%). Coen’s study also suggested that the premature closure, confirmation bias, and anchoring bias are the most common types of COVID-19-related cognitive biases in clinical reasoning. The biases were usually promoted by human factors, circumstances factors, and their interactions (Figure 1).3
Emphasising COVID-19 related cognitive bias teaching is the premise of debiasing to reduce the impact of biases in clinical decision-making. Cognitive biases are not randomly distributed; they follow a pattern always going wrong in the same direction, which makes the biases predictable and therefore somewhat correctable.4 Therefore, medical education should emphasise not only knowledge and clinical skills but also teaching students about thinking itself, which is called metacognition.
COVID-19 has gone through several iterations in China over the past three years. We carried out several cognitive bias teaching activities in our hospital and optimised the external environment prone to bias based on feedback. The teaching activities inluded (1) setting up a teaching database of concepts and illness scripts about COVID-19; (2) carrying out online case-based learning (CBL) curriculum focused on COVID-19 related cognitive biases; (3) constructing an online teaching platform to exchange views on factors that contribute to COVID-19-related biases; and (4) establishing reasonable arrangements and a standardised process to minimise the biases caused by circumstance factors (Figure 1). These teaching activities also promote the improvement of hospital management, de-biasing measures such as opening buffer wards, closed-loop management, COVID-19 diagnosis checklists, and “COVID-19 multidisciplinary team were adopted according to the debiasing suggestion. Retrospective analysis showed that COVID-19 bias teaching activities were effective and necessary. The coincidence rate of preliminary diagnosis and final diagnosis improved from 93% (pre-course) to 99% (post-course).
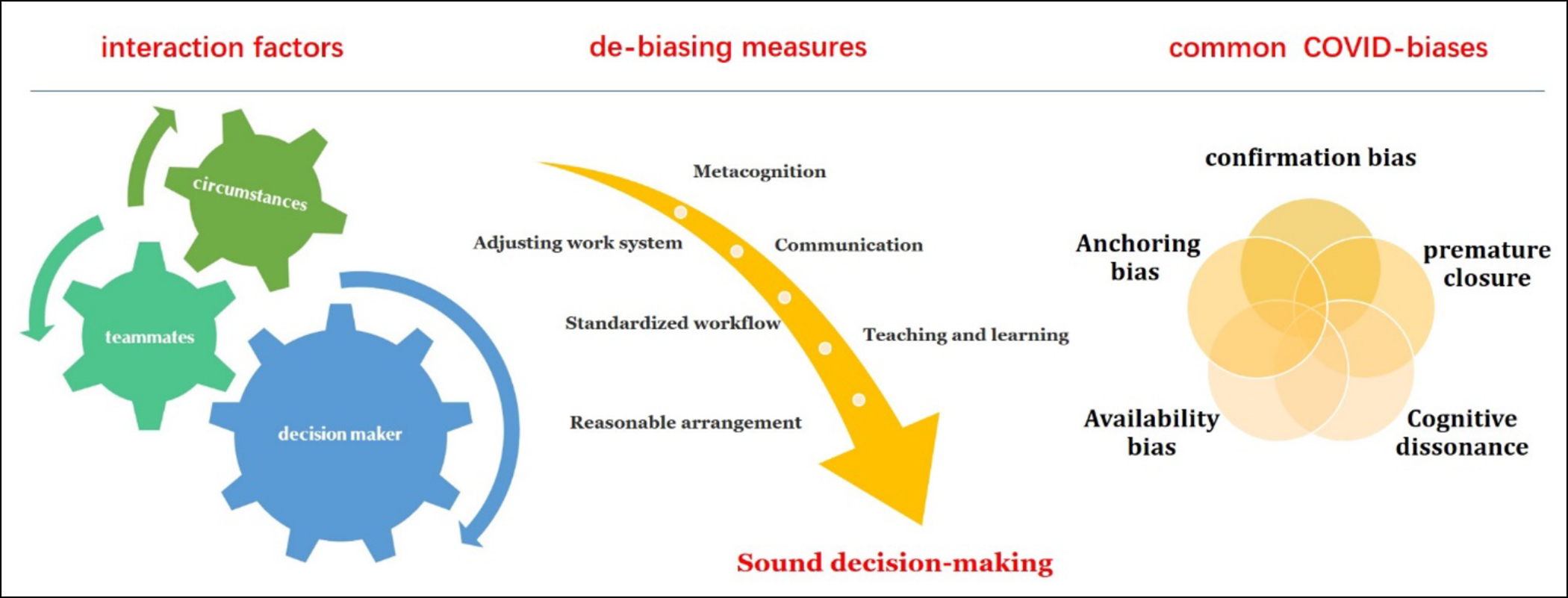 Figure 1: Common congnitive biases, influencing factors and de-biasing measures.
Figure 1: Common congnitive biases, influencing factors and de-biasing measures.
In summary, biased teaching during the COVID-19 pandemic is very important to help avoid the so-called COVID-19 blindness.
FUNDING STATEMENT:
Supported by the “Undergraduate Teaching Reform” and “Disciplinary Education Demonstration Course" research project of Jilin University.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
QFH, ZMN, JJ: Substantial contributions to the design of the work; the acquisition, analysis, interpretation of data for the work; drafting the work and revising it critically for important intellectual content; and final approval of the version.
REFERENCES
- Brown L. COVID Blindness. Diagnosis (Berl) 2020; 7(2): 83-4. doi: 10.1515/dx-2020-0042.
- Lucas NV, Rosenbaum J, Isenberg DL, Martin R, Schreyer KE. Upgrades to intensive care: The effects of COVID-19 on decision-making in the emergency department. Am J Emerg Med 2021; 49:100-3. doi: 10.1016/j.ajem.2021.05.078.
- Coen M, Sader J, Junod-Perron N, Audetat MC, Nendaz M. Clinical reasoning in dire times. Analysis of cognitive biases in clinical cases during the COVID-19 pandemic. Intern Emerg Med 2022; 17(4):979-88. doi: 10.1007/s11739- 021-02884-9.
- Norris B. Books: ABC of Clinical Reasoning: Sound and rational decision making. Br J Gen Pract 2017; 67(656): 129. doi: 10.3399/bjgp17X689737.