Aspergillosis and Mucormycosis in COVID-19 Patients: A Systematic Review
By Saira Afzal, Mehreen NasirAffiliations
doi: 10.29271/jcpsp.2022.05.639ABSTRACT
Fungal infections have increased in number since the onset of this lethal pandemic. This study aimed to assess risk factors and case fatality in COVID-19 cases with aspergillosis or mucormycosis. A systematic review was done according to PRISMA guidelines. Databases used were Google scholar, Pakmedinet, PUBMED, and MEDLINE. Twenty-one case reports and case series of mucormycosis in COVID-19 patients were identified and the mean age was 56.3 years (36 men and 12 women). The most common comorbidity was diabetes and the site was rhino orbital mucormycosis. Case fatality of 48 combined cases was calculated to be 52%. Nineteen articles of aspergillosis were included. Diabetes was the most common comorbidity in cases. The number of affected men cases was more than women. The incidence of aspergillosis in critically sick COVID-19 patients was calculated to be 9.3%. Case fatality was calculated to be 51.2%. Screening can be a beneficial tool for decreasing morbidity and mortality.
Key Words: COVID-19, Mucormycosis, Aspergillosis.
INTRODUCTION
COVID-19 pandemic started in China and subsequently spread throughout the world at an alarming rate. The disease caused by this virus can involve multiple systems of the body. Recently, researchers and medical care providers have noticed that fungal infections such as Aspergillosis and Mucormycosis are on an increasing trend among patients already infected with this lethal covid virus. These fungal infections spread through spores of these fungi that are spread everywhere in the environment. Normal healthy people continue to breathe in the air without being affected by these spores. Getting infected with these fungi is a rare occurrence but patients who are already immunocompromised and suffering from lung diseases due to COVID-19 are more vulnerable to acquiring these devastating pathogens.
Mucormycosis is also known as black fungus. It can affect the nasal cavity, sinuses, lungs, gastrointestinal tract, and skin. When a pathogen enters the bloodstream, it can cause disseminated mucormycosis. Rhino cerebral is the most common site involved in mucormycosis. This disease does not spread by person-to-person contact. Treatment is done with anti-fungal agents and most cases do require surgical recession of the site involved.1
Aspergillosis is commonly known as mold that also affects those who have a weakened immune system or any lung disease for example asthmatics or chronic obstructive lung disease. The mortality with this disease is high.2 There is an association between increased frequency of pulmonary aspergillosis and influenza. Influenza was an independent risk factor for aspergillosis. Early diagnosis and prophylactic antifungals improve the prognosis of patients.3 It is speculated that immune dysregulation associated with acute respiratory distress syndrome (ARDS), disrupted ciliary clearance, and lymphopenia due to severe respiratory viral infection may contribute to the development of invasive pulmonary aspergillosis in critically ill patients with COVID-19.4
Aspergillosis and mucormycosis have a high prevalence in the covid-19 positive population. A study done on 184,500,000 people has revealed that 1.78% have been shown to have serious fungal infections.5 The present study aimed to identify the comorbidities and case fatality of aspergillosis or mucormycosis in COVID-19 cases. This study will also identify the incidence of aspergillosis in critically sick persons that will including both ICU patients and mechanically ventilated cases. Knowledge generated from this systematic review will highlight the importance of preventing and early screening in critically sick persons of COVID-19 as this disease has high morbidity and mortality.
METHODOLOGY
The systematic review was done according to PRISMA guidelines 2020 for an extensive literature search. Articles on aspergillosis or mucormycosis in COVID-19 patients from 1st January 2020 to 15th June 2021 were searched. Databases used were Google scholar, Pakmedinet, PUBMED and MEDLINE. The date of my search was 15th June 2021. PRISMA flowchart is shown in Figure 1. In each database Boolean operators and keywords used were [(Aspergillosis or Mucormycosis) and COVID-19].
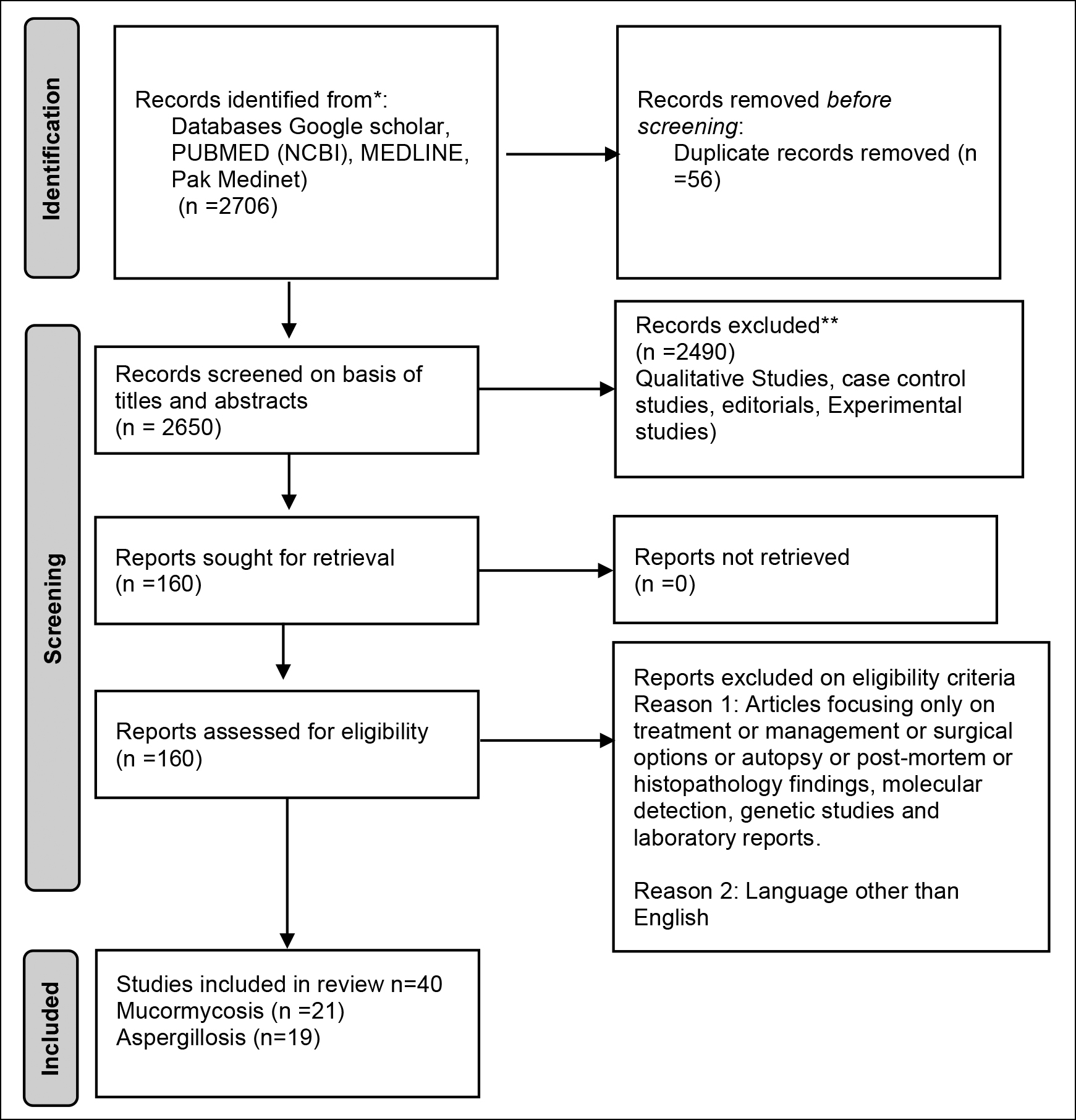 Figure 1: Identification of studies via databases and registers.
Figure 1: Identification of studies via databases and registers.
The participants were hospitalised for COVID-19 cases having fungal infections aspergillosis or mucormycosis. There was no intervention and comparison group. The outcome was noted in terms of case fatality.
The inclusion criteria was articles on mucormycosis and aspergillosis in COVID-19 patients which have mentioned co-morbidities and case fatality. For mucormycosis in COVID-19 cases; case reports and cases series were included in this study. For aspergillosis in COVID-19 cases; original articles and abstracts were included. Case reports and case series were excluded for aspergillosis and COVID-19 patients. Articles focusing on treatment, management, surgical options, autopsy, postmortem, histopathology findings, molecular detection, genetic studies, and laboratory reports were excluded. Articles with languages other than English were also excluded.
For the selection of articles, 2 researchers independently screened the articles on basis of title and abstract during the first phase. The articles meeting the eligibility criteria entered phase 2 of screening in which the full text of the articles was read by both reviewers independently. Articles were included according to standard PRISMA guidelines.
Two reviewers independently extracted data from the included studies. Data were extracted from eligible studies which included authors' name, age, gender, site of disease, co-morbidities, and case fatality. Incidence of aspergillosis in COVID-19 was also extracted. These were entered in Microsoft Excel. For calculating comorbidities and case fatality of mucormycosis in COVID-19; the quality of case reports and case series of mucormycosis for bias assessment was not accessed due to the limited number of case reports and case series.
Articles used for calculating the combined incidence of aspergillosis were published in peer-reviewed journals, and were either prospective or retrospective cohort studies on hospitalized patients of COVID-19 (either mechanically ventilated or not mechanically ventilated). The articles with the confirmed diagnosis on culture, galactomannan, and PCR for aspergillosis were included. For quality assessment of articles used for calculating incidence The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews (Checklist for Cohort Studies) was used.6 Data was extracted and entered in Microsoft Excel.
RESULTS
As mentioned in Figure 1, databases (Google scholar, PUBMED (NCBI), MEDLINE, Pak Medinet) yielded 2706 articles. Fifty-six duplicates were removed. Screening on basis of titles and abstracts yielded 160 papers. The full text of these 160 papers were read by both reviewers thoroughly. Articles focusing only on treatment or management or surgical options or autopsy or post-mortem or histopathology findings, molecular detection, genetic studies, and laboratory reports. Articles other than English were also excluded. As a result of which 40 articles were included in the study.
Twenty-one case reports and case series of mucormycosis in COVID-19 patients were identified.7-27 The total number of cases was 48 patients. The mean age was found to be 56.312 years with a standard deviation of 15.55 years. There were 36 men and 12 women. The most common comorbidity was diabetes (35 out of 48 cases). Other risk factors included chronic kidney disease, ischemic heart disease, transplant, decompensated liver disease, and hypertension (Table I). History of steroid use was present in 45.83% of COVID cases developing mucormycosis as shown in Figure 2. The most common site was Rhino orbital mucormycosis. However cutaneous, gastrointestinal, and pulmonary mucormycosis were also reported. Twenty-five cases died and 23 were discharged (Table I). The chi-square test did not show a significant difference in outcome between men and women (p = 0.133). The combined case fatality of 48 cases was calculated to be 52%.7-27
For Aspergillosis, ninteen articles meeting the inclusion criteria were included. Diabetes was the most common comorbidity in cases. Other risk factors include hypertension, steroid use, hypertension, heart disease, chronic obstructive pulmonary disease, malignancies, and chronic kidney disease. The incidence of aspergillosis in critically sick COVID-19 patients was calculated by including 9 studies as shown in Table II.28-36 Forest plot shows the incidence of aspergillosis in critically sick COVID-19 patients using a 95% confidence interval (Figure 3).
Table I: Case Reports and Case Series of Mucormycosis.
|
Study Name |
Age in years |
Gender |
Site of mucormycosis |
Comorbidities |
Outcome |
|
Fouad YA et al. 20217 |
55
63
54
67
41
42
|
Male
Female
Male
Male
Female
Male
|
Rhino-orbital Cerebral
|
Diabetes
Diabetes
Diabetes, CKD, IHD
Diabetes, CKD
Diabetes
Diabetes |
Death
Discharged
Death
Death
Discharged
Discharged
|
|
Paul SS et al. 20218 |
62
70
53
38
37
32
48
60
34 |
Male
Male
Male
Male
Male
Male
Male
Male
Female |
Rhino-orbital Cerebral Sino-nasal
Rhino-orbital Cerebral Rhino-Sino Orbital Sino nasal
Rhino orbital Cerebral Rhino orbital Cerebral Pulmonary
Sino nasal
|
Diabetes
Diabetes
Diabetes, CKD Renal transplant, Diabetes DCLD, Diabetes Chronic Granulomatous Disease
Diabetes
Diabetes, Tuberculosis
End Stage Kidney Disease
- |
Death
Discharged
Death
Discharged
Discharged
Discharged
Discharged
Death
Death |
|
Tabarsi P, et al 20219 |
50 |
Female |
Sino nasal |
Diabetes, Hypertension |
Discharged |
|
Bayram N, et al. 202110 |
Mean age 73.1 |
Male
Male
Male
Male
Male
Male
Male
Male
Male
Female
Female |
Rhino orbital |
CKD
CKD, Diabetes
CKD, Diabetes
AKF, Diabetes
AKF
Myelodysplastic Syndrome Diabetes Diabetes
Diabetes
Diabetes
Diabetes
- |
Death
Death
Death
Death
Death
Death
Death
Discharged
Discharged
Discharged
Discharged
|
|
Shah D, et al. 202111 |
45
50
60
65
|
Male
Male
Female
Male |
Rhino orbital
Orbital
Sinuses
Sinuses |
Diabetes
-
Diabetes
- |
Discharged
Discharged
Discharged
Discharged |
|
Waizel-Haiat S, et al. 202112
|
24 |
Female |
Sino Orbital |
- |
Discharged |
|
Alekseyev K, et al. 202113 |
41 |
Male |
Cutaneous |
Diabetes |
Death |
|
Khatri A, et al. 202114 |
68 |
Male |
Naso orbital |
Heart transplantation, CHD, Diabetes, Hypertension |
Discharged |
|
Maini A, et al. 202115 |
38 |
Male |
Gastrointestinal |
- |
Died |
|
do Monte Junior ES, et al. 202016 |
86 |
Male |
Rhino Orbital |
Hypertension |
Death |
|
Mehta S, et al. 202017 |
60 |
Male |
Pulmonary |
Diabetes |
Died |
|
Khan N, et al. 202018 |
44 |
Female |
Rhino Orbital Cerebral |
Diabetes |
Discharged |
|
Revannavar SM, et al. 202119 |
50 |
Female |
Rhino Cerebral |
Diabetes |
Died |
|
Farid HA, et al. 202120 |
53 |
Male |
Sino Orbital |
Diabetes, hypertension |
Discharged |
|
Meshram HS, et al. 202121 |
47
25 |
Male
Male |
Rhino orbital
Pulmonary
|
Hypertension, Diabetes, Kidney Transplant
Hypertension, Diabetes, Kidney Transplant |
Died
Died |
|
Mekonnen ZK, et al. 202122 |
60 |
Male |
Rhino orbital |
Hypertension, Diabetes, Asthma, Hyperlipidemia |
Died |
|
Johnson AK, et al. 202123 |
79 |
Male |
Pulmonary |
Diabetes, Hypertension |
Discharged |
|
Chowdhary S, et al. 202124 |
45 |
Female |
Rhino orbital |
Diabetes |
Death |
|
Saldanha M, et al. 202125 |
32 |
Female |
Paranasal |
Diabetes |
Discharged |
|
Pasero D, et al. 202126 |
66 |
Male |
Pulmonary |
Hypertension |
Death |
|
Garg D, et al. 202127 |
55 |
Male |
Pulmonary |
Diabetes, Hypertension, IHD, End Stage Kidney Disease |
Discharged |
The combined incidence was 9.3% with a confidence interval of 3.93% to 14.67%. Case fatality was calculated to be 51.2% as shown in Table III.37-44 The number of male cases was more than females.33, 37
DISCUSSION
This study aimed to assess the risk factors and case fatality of aspergillosis and mucormycosis in COVID-19 patients. Incidence of aspergillosis in critically sick patients that included both intensive care unit patients and mechanically ventilated patients of COVID-19 has also been calculated. This study highlighted the importance of prevention and early screening of fungal infections in severe cases of COVID-19 as this lethal disease has high morbidity and mortality. Repeated surgical interventions are required to remove infected tissue which causes disfigurement and mental trauma.
The mean age of cases with mucormycosis was 56 years. This result is similar to other studies.45 The number of males is more than females. This finding is consistent with previous studies but the exact cause of this gender disparity is unknown.46,47A retrospective study in Mexico has shown more male patients with mucormycosis. There are more males in this study as severe COVID-19 and mucormycosis are generally more common in males.48
Diabetes was the most common risk factor found in other systematic reviews of mucormycosis.47-49 Diabetes is an immunocompromised state and its prevalence is high across the globe.
Table II: Incidence of aspergillosis in critically sick patients of COVID-19.
|
Study Name |
Study design |
Sample size (n) |
Incidence (n) % |
|
Dellière S, et al. 202128 |
Retrospective Cohort |
366 |
21 (5.7%) |
|
Versyck M, et al. 202129 |
Cohort |
54 |
2 (3.7%) |
|
Gouzien L, et al. 202130 |
Retrospective Cohort |
53 |
1 (1.8%) |
|
Bedini A, et al. 202131 |
Retrospective Cohort |
53 |
5 (9.4%) |
|
Lahmer T, et al. 202132 |
Cohort |
32 |
11 (34%) |
|
Pintado MV, et al. 202133 |
Cohort |
83 |
16 (19.2%) |
|
van Arkel A , et al. 202134 |
Cohort |
31 |
8 (25.8%) |
|
Bartoletti M, et al. 202035 |
Cohort |
185 |
30 (16.2%) |
|
Machado M, et al. 202136 |
Prospective Study |
239 |
8 (3.3%) |
|
Total |
|
1096 |
102 (9.3%) |
Table III: Number of cases who died due to aspergillosis in COVID-19.
|
Study |
Total number of cases n |
Number of cases who died n (%) |
|
Nasir N, et al. 202137 |
9 |
4 (44.4%) |
|
Lai CC, et al. 202138 |
34 |
22 (64.7%) |
|
Kariyawasam RM, et al. 202139 |
182 |
91 (50%) |
|
Chong WH, et al. 202140 |
192 |
94 (48.9%) |
|
Pintado MV, et al. 202133 |
16 |
5 (31.2%) |
|
Apostolopoulou A, et al. 202141 |
85 |
46 (54.1%) |
|
Salmanton-Garcia J, et al. 202142 |
186 |
97 (52.1%) |
|
Abdalla S, et al. 202143 |
2 |
2 (100%) |
|
Alobaid K, et al. 202144 |
2 |
2 (100%) |
|
Total |
708 |
363 (51.2%) |
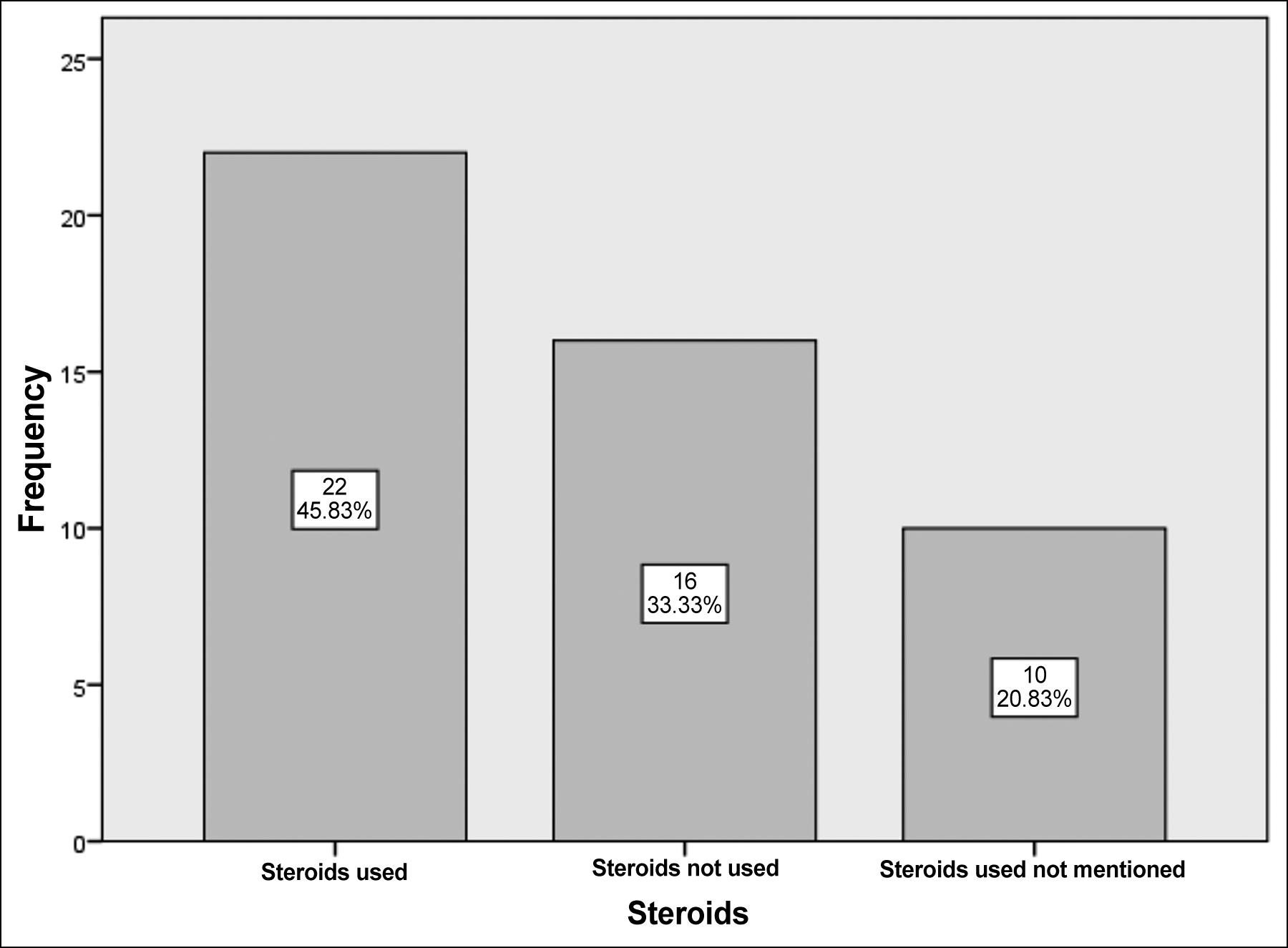 Figure 2: Steroid use among cases of COVID-19 with mucomycosis.
Figure 2: Steroid use among cases of COVID-19 with mucomycosis.
History of steroid use was fairly common among respondents of this study. Glucocorticoid-induced immunosuppression may be responsible for increased fungal infections.50 Rhino orbital mucormycosis was the most common site in cases.51 The combined case fatality in this study was found to be 52%. The mortality of pulmonary mucormycosis is slightly higher. A study done has demonstrated mortality of 57%. Another systematic review on mucormycosis has shown 67% survival with antifungal medications and surgery.40 This study has reported higher mortality (52%). This may be because cases of mucormycosis have COVID-19 infection as well which has resulted in higher case fatality.
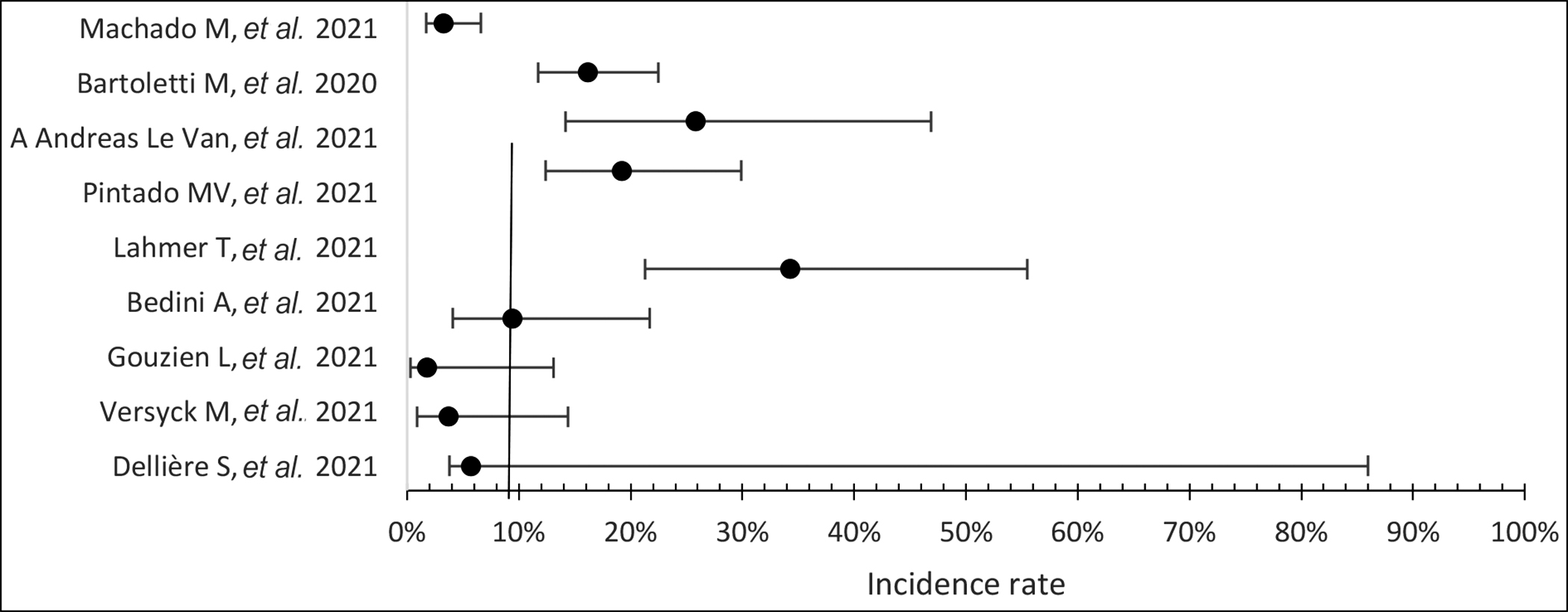 Figure 3: Incidence of aspergillosis in critically sick COVID-19 Patients.
Figure 3: Incidence of aspergillosis in critically sick COVID-19 Patients.
Aspergillosis has a higher incidence in critically sick COVID-19 patients. That demands early screening. The combined incidence was found to be 9.3% with a range of 1.88% to 25%.
In another systematic review, the incidence was found to be 13.5%.40 This may be because in this study both mechanically ventilated and not mechanically ventilated Intensive Care Unit (ICU) patients were included. The average case fatality was found to be 51.2%. Another systematic review has calculated the case fatality of aspergillosis to be 58%.52 The risk factors of aspergillosis were diabetes, hypertension, steroid use, hypertension, heart disease, chronic obstructive pulmonary disease, malignancies, and chronic kidney disease.
The limitations of this study are that it has covered comorbidities and case fatalities. Treatment, management, and diagnosis options were beyond the scope of this article. Quality assessment of articles (case reports and case series) on mucormycosis in COVD-19 cases was not accessed due to their limited number. The strengths of this study are that it is a systematic review with a thorough data search. It has covered two lethal fungal infections which have shown increased prevalence since the COVID pandemic. The most common risk factor was diabetes. Health education and lifestyle modifications should be promoted to halt the rise in diabetes.
CONCLUSION
Case fatality from aspergillosis and mucormycosis in Covid-19 cases is quite high. Diabetes is the most common comorbidity in the cases of COVID-19 developing mucormycosis or aspergillosis. The incidence of aspergillosis in critically sick COVID cases is around 9.3%. Early screening and prophylactic antifungals can improve the prognosis of this disease.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
SA: Carried out the conception and design of the research, Screening of articles and data extraction, analysis, and interpretation.
MN: drafted the manuscript and screening of articles was done with data extraction and analysis.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Mucormycosis. Centers for Disease Control and Prevention. https://www.cdc.gov/fungal/diseases/mucormycosis/index.html. (Accessed 22/06/2021).
- Aspergillosis. Centers for Disease Control and Prevention. https://www.cdc.gov/fungal/diseases/aspergillosis/index.html. (Accessed 22/06/2021).
- Schauwvlieghe AF, Rijnders BJ, Philips N, Verwijs R, Vanderbeke L, Van Tienen C, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: A retrospective cohort study. Lancet Respir Med 2018; 6(10):782-92. doi: 10.1016/S2213-2600(18)30274-1.
- Jabeen K, Farooqi J, Mirza S, Denning D, Zafar A. Serious fungal infections in Pakistan. Eur J Clin Microbiol Infect Dis 2017; 36(6):949-56. doi: 10.1007/s10096-017-2919-6.
- Koehler P, Bassetti M, Chakrabarti A, Chen SC, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: The 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis 2020; 21(6):e149-e162. doi: 10.1016/S1473- 3099(20)30847-1.
- The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews Checklist for Cohort Studies. Available at: https://jbi. global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Cohort_Studies2017_0.pdf (Accessed 22/06/2021).
- Fouad YA, Abdelaziz TT, Askoura A, Saleh MI, Mahmoud MS, Ashour MM. Spike in rhino-orbital-cerebral mucormycosis cases presenting to a tertiary care center during the COVID-19 pandemic. Front Med 2021; 8:645270. doi: 10.3389/fmed.2021.645270.
- Paul SS, Kumar R, Meena VP, Ramprasad A, Garg P, Keri VC. Clinical characteristics and outcomes of 16 cases with COVID19 and mucormycosis: Experience from a tertiary care center. In India Review Literature 2021. doi:10. 21203/rs.3.rs-533347/v1.
- Tabarsi P, Khalili N, Pourabdollah M, Sharifynia S, Naeini AS, Ghorbani J, et al. Case report: Coronavirus disease 2019-associated rhinosinusitis mucormycosis caused by rhizopus arrhizus: A rare but potentially fatal infection occurring after treatment with corticosteroids. Am J Trop Med Hyg 2021; 105(2):449-53. doi: 10.4269/ajtmh.21-0359.
- Bayram N, Ozsaygılı C, Sav H, Tekin Y, Gundogan M, Pangal E, et al. Susceptibility of severe COVID-19 patients to rhino-orbital mucormycosis fungal infection in different clinical manifestations. Jpn J Ophthalmol 2021; 31:1-1. doi: 10. 1007/s10384-021-00845-5.
- Shah D, Talwar D, Kumar S, Acharya S, Dubey A. Mucormycosis as a complication of LONG COVID: A case series. J Med Sci 2021; 25(112):1331-7.
- Waizel-Haiat S, Guerrero-Paz JA, Sanchez-Hurtado L, Calleja-Alarcon S, Romero-Gutierrez L. A case of fatal rhino-orbital mucormycosis associated with new onset diabetic ketoacidosis and COVID-19. Cureus 2021; 13(2). doi: 10.7759/cureus.13163.
- Alekseyev K, Didenko L, Chaudhry B. Rhinocerebral mucormycosis and COVID-19 pneumonia. J Med Case Rep 2021; 12(3):85. doi: 10.14740/jmc3637.
- Khatri A, Chang KM, Berlinrut I, Wallach F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient–case report and review of literature. Med Mycol 2021; 31(2):101125. doi: 10.1016/j.mycmed.2021. 101125.
- Maini A, Tomar G, Khanna D, Kini Y, Mehta H, Bhagyasree V. Sino-orbital mucormycosis in a COVID-19 patient: A case report. Int J Surg Case Rep 2021; 82:105957. doi: 10. 1016/j.ijscr.2021.105957.
- do Monte Junior ES, Dos Santos ME, Ribeiro IB, de Oliveira Luz G, Baba ER, Hirsch BS, et al. Rare and fatal gastrointestinal mucormycosis (zygomycosis) in a COVID-19 patient: A case report. Clin Endosc 2020; 53(6):746. doi: 10. 5946/ce.2020.180.
- Mehta S, Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus 2020; 12(9). doi: 10.7759/cureus. 10726.
- Khan N, Gutierrez CG, Martinez DV, Proud KC. A case report of COVID-19 associated pulmonary mucormycosis. Arch Clin Cases 2021; 7(3):2020-7. doi: 10.22551/2020.28.0703. 10172.
- Revannavar SM, Supriya PS, Samaga L, Vineeth VK. COVID-19 triggering mucormycosis in a susceptible patient: A new phenomenon in the developing world? BMJ Case Rep 2021; 14(4). doi: 10.1136/bcr-2021-241663.
- Farid HA, Hashim AR, Hasrat NH. Rhinocerebral Mucormycosis as a COVID-19-related complication: A case report from Basra city, Southern Iraq. Int J Glob Sci Res 2021; 6(5):1369-74. doi: 10.1186/s12879-021-06625-3.
- Meshram HS, Kute VB, Chauhan S, Desai S. Mucormycosis in post‐COVID‐19 renal transplant patients: A lethal complication in follow‐up. Transpl Infect Dis 2021; 3. doi: 10.1111/ tid.13663.
- Mekonnen ZK, Ashraf DC, Jankowski T, Grob SR, Vagefi MR, Kersten RC, et al. Acute invasive rhino-orbital mucormycosis in a patient with COVID-19-associated acute respiratory distress syndrome. Ophthalmic Plast Reconstr Surg 2021; 37(2). doi: 10.1097/IOP.0000000000001889.
- Johnson AK, Ghazarian Z, Cendrowski KD, Persichino JG. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Med Mycol Case Rep 2021; 32:64-7. doi: 10.1016/j.mmcr.2021.03.006.
- Chowdhary S. The Face of the COVID-19 Pandemic: Invasive rhino-orbital mucormycosis. Clin Surg J 2021; 4(S7):14-7.
- Saldanha M, Reddy R, Vincent MJ. Paranasal mucormycosis in COVID-19 patient. Indian J Otolaryngol Head Neck Surg 2021; 22:1-4. doi: 10.1007/s12070-021-02574-0.
- Pasero D, Sanna S, Liperi C, Piredda D, Branca GP, Casadio L, et al. A challenging complication following SARS-CoV-2 infection: A case of pulmonary mucormycosis. Infection 2020; 1-6. doi: 10.1007/s15010-020-01561-x.
- Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia 2021; 5:1-0. doi: 10.1007/ s11046-021-00528-2.
- Dellière S, Dudoignon E, Fodil S, Voicu S, Collet M, Oillic PA, et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: A french multicentric retrospective cohort. Clin Microbiol Infect 2021; 27(5):790. doi: 10.1016/j.cmi.2020.12.005.
- Versyck M, Zarrougui W, Lambiotte F, Elbeki N, Saint-Leger P. Invasive pulmonary aspergillosis in COVID-19 critically ill patients: Results of a French monocentric cohort. Med Mycol J 2021; 31(2):101122. doi: 10.1016/j.mycmed.2021. 101122.
- Gouzien L, Cocherie T, Eloy O, Legriel S, Bedos JP, Simon C, et al. Invasive aspergillosis associated with Covid-19: A word of caution. Infectious Diseases Now 2021; 51(4):383-6. doi: 10.1016/j.idnow.2020.12.008.
- Nori P, Cowman K, Chen V, Bartash R, Szymczak W, Madaline T, et al. Bacterial and fungal coinfections in COVID-19 patients hospitalised during the New York city pandemic surge. Infect Control Hosp Epidemiol 2021; 42(1):84-8. doi: 10.1017/ice.2020.368.
- Lahmer T, Kriescher S, Herner A, Rothe K, Spinner CD, Schneider J, et al. Invasive pulmonary aspergillosis in critically ill patients with severe COVID-19 pneumonia: Results from the prospective AspCOVID-19 study. Plos One 2021; 16(3). doi: 10.1371/journal.pone.0238825.
- Pintado MV, Camiro-Zúñiga A, Soto MA, Cuenca D, Mercado M, Crabtree-Ramirez B. COVID-19-associated invasive pulmonary aspergillosis in a tertiary care center in Mexico City. Med Mycol 2021; 59(8):828-33. doi: 10.1093/mmy/ myab009.
- van Arkel A, Rijpstra TA, Belderbos H, van Wijngaarden P, Verweij P E, Bentvelsen RG. COVID-19-associated pulmonary aspergillosis. Am J Respir Crit Care Med 2020; 202(1):132-5. doi: 10.1164/rccm.202004-1038LE.
- Bartoletti M, Pascale R, Cricca M, Rinaldi M, Maccaro A, Bussini L, et al. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: A prospective study. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa1065.
- Machado M, Valerio M, Álvarez‐Uría A, Olmedo M, Veintimilla C, Padilla B, et al. Invasive pulmonary aspergillosis in the COVID‐19 era: An expected new entity. Mycoses 2021; 64(2):132-43. doi: 10.1111/myc.13213.
- Nasir N, Farooqi J, Mahmood SF, Jabeen K. COVID‐19‐associated pulmonary aspergillosis (CAPA) in patients admitted with severe COVID‐19 pneumonia: An observational study from Pakistan. Mycoses 2020; 63(8):766-70. doi: 10. 1111/myc.13135.
- Lai CC, Yu WL. COVID-19 associated with pulmonary aspergillosis: A literature review. J Microbiol Immunol Infect 2021; 54(1):46-53. doi: 10.1016/j.jmii.2020.09.004.
- Kariyawasam RM, Dingle TC, Kula BE, Sligl WI, Schwartz IS. COVID-19 Associated pulmonary aspergillosis: Systematic review and patient-level meta-analysis. Medrxiv 2021. doi: 10.1101/2021.05.21.21257626.
- Chong WH, Neu KP. The incidence, diagnosis, and outcomes of COVID-19-associated pulmonary aspergillosis (CAPA): A systematic review. J Hosp Infect 2021; 113:115-29. doi: 10.1016/j.jhin.2021.04.012.
- Apostolopoulou A, Esquer Garrigos Z, Vijayvargiya P, Lerner AH, Farmakiotis D. Invasive pulmonary aspergillosis in patients with SARS-CoV-2 infection: A systematic review of the literature. Diagnostics 2020; 10(10):807. doi: 10.3390/diagnostics10100807.
- Salmanton-Garcia J, Sprute R, Stemler J, Bartoletti M, Dupont D, Valerio M, et al. COVID-19–associated pulmonary aspergillosis, March–August 2020. Emerg Infect Dis 2021; 27(4):1077. doi: 10.3201/eid2704.204895.
- Abdalla S, Almaslamani MA, Hashim SM, Ibrahim AS, Omrani AS. Fatal coronavirus disease 2019-associated pulmonary aspergillosis: A report of two cases and review of the literature. IDCases 2020; 22. doi: 10.1016/j.idcr.2020.e00935.
- Alobaid K, Yousuf B, Al-Qattan E, Muqeem Z, Al-Subaie N. Pulmonary aspergillosis in two COVID-19 patients from Kuwait. Access Microbiol 2021; 3(3). doi: 10.1099/acmi. 0.000201.
- Ravani SA, Agrawal GA, Leuva PA, Modi PH, Amin KD. Rise of the phoenix: Mucormycosis in COVID-19 times. Indian J. Ophthalmol 2021; 69(6):1563-8. doi: 10.4103/ijo.IJO_ 310_21.
- Pakdel F, Ahmadikia K, Salehi M, Tabari A, Jafari R, Mehrparvar G, et al. Mucormycosis in patients with COVID‐19: A cross‐sectional descriptive multicenter study from Iran. Mycoses 2021; 64(10):1238-52. doi: 10.1111/myc.13334.
- Bonifaz A, Tirado‐Sánchez A, Hernández‐Medel ML, Araiza J, Kassack JJ, del Angel‐Arenas T, Moisés‐Hernández JF, et al. Mucormycosis at a tertiary‐care center in Mexico. A 35‐year retrospective study of 214 cases. Mycoses 2021; 64(4): 372-80. doi: 10.1111/myc.13222.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DC, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect 2019; 25(1):26-34. doi: 10.1016/j.cmi.2018.07.011.
- Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. The Lancet 2003; 362(9398):1828-38. doi: 10.1016/S0140-6736(03)14904-5.
- Vaezi A, Moazeni M, Rahimi MT, de Hoog S, Badali H. Mucormycosis in Iran: A systematic review. Mycoses 2016; 59(7):402-15. doi: 10.1111/myc.12474.
- Muthu V, Agarwal R, Dhooria S, Sehgal IS, Prasad KT, Aggarwal AN, et al. Has the mortality from pulmonary mucormycosis changed over time? A systematic review and meta-analysis. Clin Microbiol Infect 2021; 27(4):538-49. doi: 10.1016/j.cmi.2020.12.035.
- Lin SJ, Schranz J, Teutsch SM. Aspergillosis case-fatality rate: Systematic review of the literature. Clin Infect Dis 2001; 32(3):358-66. doi: 10.1086/318483.