Anatomical Morphology and Related Angles of Foramen Ovale: A Three-dimensional Computed Tomography Reconstruction
By Zhe Cheng1, Yuan Liang Hu1, Yu Xi Sun1, Li Zhi Liang1, Di Di Pan2, Da Wei Wang1Affiliations
doi: 10.29271/jcpsp.2023.01.113ABSTRACT
This study aimed to report the three-dimensional reconstruction of the foramen ovale (FO) based on computed tomography angiography and describe its shape and related angles. A retrospective analysis of 199 adult patients who were hospitalised at the Department of Neurosurgery, The Second Affiliated Hospital of Bengbu Medical College, Bengbu, China, from January to December 2020 was conducted. The original DICOM files of patients' computed tomography scans were processed by 3D Slicer software to reconstruct the three-dimensional skull. The morphological characteristics of the FO on both sides were analysed. Their size, related angles and volumes, and the differences between the two sides and gender were compared. A total of 398 FO from 199 patients were studied. The most frequent shape of the FO was oval, accounting for 54.27%. The mean lengths of the right and the left sides were 5.40±1.51 and 5.10±1.18mm, respectively. The mean width on the right and left sides was 3.23±1.16 and 3.33±1.19 mm, respectively. The FO is most commonly oval in shape. Clinicians may use the anatomical characteristics regarding the size and shape of the FO for diagnosis and treatment.
Key Words: Foramen ovale, Computed tomographic angiography, 3-Dimensional anatomy.
The foramen ovale (FO) is an important anatomical landmark of the skull; it is located on the greater sphenoid wing on both sides of the sella in the middle cranial fossa, with the foramen spinosum and foramen rotundum located posterolaterally and anteromedially, respectively.1 The FO plays an important role in clinical diagnosis and surgery because of its anatomical characteristics. In particular, the FO is involved in percutaneous micro-balloon compression (PBC) of the Gasserian ganglion and percutaneous radiofrequency thermocoagulation to alleviate symptoms of trigeminal neuralgia, induce mandibular nerve block anaesthesia, and perform a biopsy.
The FO exhibits several typical shapes such as oval, D-shape, almond shape, round, and irregular, of which the oval shape is the most common.2 Ray et al. reported that the mean length of the FO was 7.46 ± 1.41 and 7.01 ± 1.41 mm, and the mean width was 3.21 ± 1.02 and 3.29 ± 0.85 mm on the right and left sides, respectively.3 However, the difference was not significant.
By analysing a large amount of imaging data, the present study aimed to describe the morphometric and anatomical variations of the FO and calculate its size and related angles. The findings were also compared with previous studies on adult dry skulls. The findings of the present research could serve as an important reference for clinicians to perform surgical and diagnostic procedures.
A retrospective analysis of 199 adult patients who were hospitalised in the Department of Neurosurgery, The Second Affiliated Hospital of Bengbu Medical College, Bengbu, China, from January to October 2020 was conducted. The patients included 115 males and 84 females, with an average age of 65.25±12.42 years. The study was approved by the Ethics board of hospital. Cranial CTA was performed with a Philips Aquilion 64-slice spiral CT machine (Amsterdam, Netherlands). The original images were obtained in DICOM format and then imported directly into 3D Slicer software for processing. The first step was to reconstruct the three-dimensional model of the skull. Next, the morphology of the FO was classified into oval, D-shaped, almond-shaped, round, and irregular. The maximum length (L) and width (W) of the FO of both sides were recorded, and the distance (D) between the inner and outer walls of the FO was measured. The FO is a tubular columnar structure with internal and external openings. The volume (V) of the tubular structure of the FO was also calculated.
Table I: The related measurement values of the morphology of the foramen ovale.|
Parameters |
Right |
|
Left |
p-value |
|||
|
Mean±SD |
Maximum |
Minimum |
Mean±SD |
Maximum |
Minimum |
||
|
L |
5.40±1.51 |
10.53 |
2.83 |
5.10±1.18 |
8.97 |
2.43 |
0.025 |
|
W |
3.23±1.16 |
8.73 |
1.27 |
3.33±1.19 |
11.60 |
1.37 |
0.374 |
|
D |
4.10±1.53 |
8.83 |
1.27 |
4.59±1.41 |
9.30 |
1.57 |
0.001 |
|
V |
51.98±31.23 |
169.65 |
4.33 |
58.54±31.51 |
159.34 |
2.63 |
0.035 |
|
∠Α ∠Β ∠C |
65.59±10.79 65.99±9.31 30.44±10.07 |
101.83 87.50 58.27 |
31.70 6.27 9.83 |
65.81±11.57 62.65±10.13 31.43±11.02 |
112.00 87.97 69.30 |
34.23 6.17 10.10 |
0.845 0.001 0.417 |
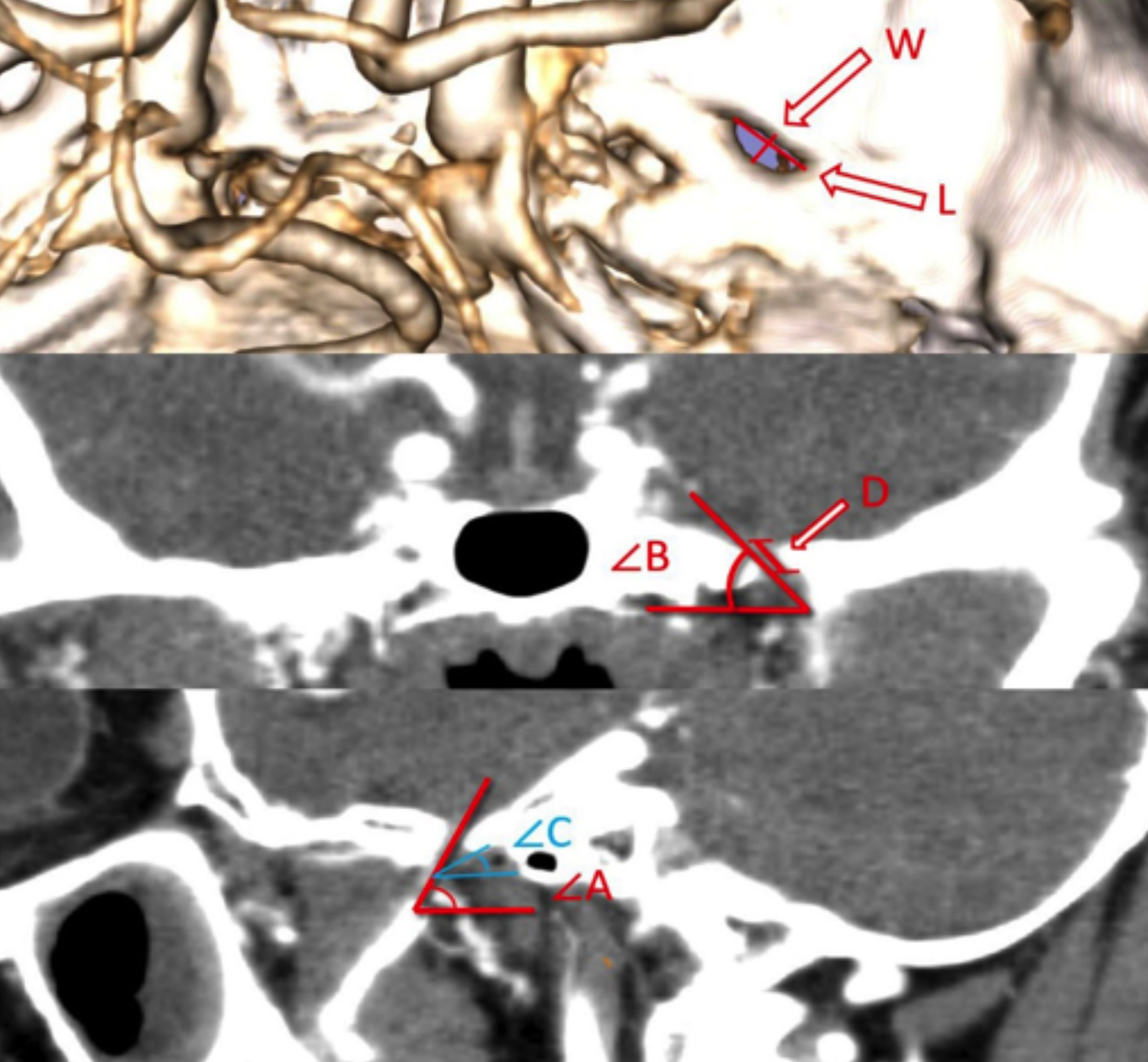 Figure 1: The relevant anatomical values and angles of the foramen ovale (FO).
Figure 1: The relevant anatomical values and angles of the foramen ovale (FO).
L: Length of the FO; W: Width of the FO; D: Distance between the inner and outer walls of the FO; V: Volume of the tubular structure of the FO; ∠Α: The backward inclination angle between the long axis of the FO and the horizontal line in the sagittal position; ∠Β: The angle between the inward inclination of the FO and the horizontal line in the coronal position; ∠C: The angle between the line connecting the anterior and posterior walls of the FO and the horizontal line in the sagittal position.
The backward inclination angle between the long axis of the FO and the horizontal line in the sagittal position was measured and designated as ∠Α. The angle between the inward inclination of the FO and the horizontal line in the coronal position was measured and designated as ∠Β. The angle between the line connecting the anterior and posterior walls of the FO and the horizontal line in the sagittal position was measured and designated as ∠C (Figure 1). All values were calculated by two professional doctors, and each value was measured thrice. The data were statistically analysed using Chi-square test and Student’s t-test, respectively. SPSS Version 16 and GraphPad Prism 8.0.2 were used for analysis, and a p-value of < 0.05 was considered significant.
The three-dimensional model of the skull was successfully reconstructed by 3D Slicer. The shape of all the FO observed in this study was classified into oval, almond-shaped, round, and irregular. The most common morphology observed was oval 54.27% (n=216), followed by almond-shaped 18.34% (n=73), round 14.82% (n=59), and irregular 12.56% (n=50). Significant differences in FO morphology were observed between the two sides (p <0.001) and between the genders (p = 0.005) by Chi-square test. The mean lengths on the right and left sides were 5.40 ± 1.51 and 5.10 ± 1.18 mm, respectively, whereas the observed maximum and minimum lengths were 10.53 and 2.83 mm, and 8.97 and 2.43 mm on the right and left sides, respectively. The mean widths on the right and left sides were 3.23±1.16 and 3.33±1.19 mm, respectively. The mean volume of the tubular structure of the FO was 51.98 ± 31.23 and 68.54 ± 31.51 mm3 on the right and left sides, respectively. The average value of ∠Α was 65.59 ± 10.79° and 58.54 ± 31.51° on the right and left sides, respectively. The mean value of ∠Β was 65.99 ± 9.31° and 62.65 ± 10.13° on the right and left sides, respectively. The mean value of ∠C was 30.44 ± 10.07° and 31.43 ± 11.02° on the right and left sides, respectively (Table I). Student’s t-test was used to compare the various measured anatomical values of the left and right foramen ovale. P-value are presented in Table I.
The FO is located on the small wing of the sphenoid bone in the middle cranial fossa.4 Neurosurgeons often use the natural anatomical characteristics of the foramen ovale to assist in the diagnosis and treatment of related diseases.5
Therefore, it is very important to understand and analyse the morphological characteristics and anatomy of the FO. By reviewing the relevant anatomical literature on the FO, the authors found that previous anatomical studies on the foramen ovale were mainly based on the measurement of adult dry skulls. Because of ligament loss, ossification, and fibroplasia in adult dry skulls, the anatomical measurement of the FO might not be accurate only by measuring adult dry skulls. There are, however, few reports on the anatomical morphology of the FO based on imaging. Therefore, as a new approach, the authors propose to use 3D Slicer software to analyse the thin CTA images of adult skulls to simulate and measure the size and related angles of the FO as much as possible.
In the present study, 3D Slicer software was used to analyse and measure the morphological and anatomical characteristics of the bilateral FO on thin CT images of 199 adult skulls. The FO is the anatomical marker of the middle cranial fossa, which connects the intracranial and extracranial pathways. Clinicians often use the anatomical characteristics of the FO to conduct diagnosis and treatment. Therefore, neurosurgeons, pain surgeons, radiologists, and anatomists need to learn and understand the anatomical characteristics of the FO.
Some limitations of this study should be acknowledged. The number of FO is not large. This study failed to correlate the morphological characteristics of FO with the disease. There are statistical differences in the morphological distribution of FO on both sides and between genders, however, it may not have special value in clinical practice. In the future, it may be necessary to enlarge the number of foramen ovale and use multiple softwares for fusion and measurement.
In this study, 3D Slicer software was used to analyse a large number of adult thin skull CTA images to study the anatomical morphology of the foramen ovale. The most common shape of the FO is oval, and its length and width are slightly smaller than those based on adult dry skulls. The FO is an oblique tubular columnar structure with internal and external openings, and the lateral opening is located in the anterolateral side of the medial opening.
FUNDING:
This work was supported by the Open Project of the Key Laboratory of Computational Medicine and Intelligent Health of Anhui Higher Education Institutes, Bengbu Medical College (AHCM2022W001).
ETHICAL APPROVAL:
This study protocol was reviewed and approved by the Ethics Committee of The Second Affiliated Hospital of Bengbu Medical College (BYEFY2022.9A).
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
ZC, YLH: Funding acquisition, conceptualisation, formal analysis, and writing the original draft.
YXS, YLH: Data curation and investigation.
DDP, LZL: Image analysis, writing review, and editing.
WDW: Data analysis, interpretation, and critical revision.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Das S, Bhattacharjee S, Pal S. A morphometric study of foramen ovale. Indian J Clinical Anatomy Physiology 2019; 6:359-62.
- Patil GV, Shishirkumar, Apoorva D. Morphometry of the foramen ovale of sphenoid bone in human dry skulls in Kerala. International J Health SciencesResearch 2014.
- Ray B, Gupta N, Ghose S. Anatomic variations of foramen ovale. Kathmandu University Medical J (KUMJ) 2005; 3(1): 64-8.
- Edwards B, Wang JM, Iwanaga J, Loukas M, Tubbs RS. Cranial nerve foramina Part I: A review of the anatomy and pathology of cranial nerve foramina of the anterior and middle fossa. Cureus 2018; 10(2):e2172. doi: 10.7759/ cureus.2172.
- Arishima H, Sindou M. Benefits and pitfalls of percutaneous biopsy for cavernous sinus tumors through the foramen ovale: Two case reports. Minimally Invasive Neurosurgery MIN 2010; 53(4):194-7. doi: 10.1055/s-0030-1263114.