Analysis of Risk Factors for Coronary Artery Lesion in Children with Kawasaki Disease
By Bing Bai, Jin-liang Ya, Chao YanAffiliations
doi: 10.29271/jcpsp.2022.08.1037ABSTRACT
Objective: To determine the frequency of coronary artery lesion (CAL) in children with Kawasaki disease (KD) and to analyse the related risk factors of CAL and the predictive value of risk factors for CAL.
Study Design: A descriptive study.
Place and Duration of Study: Department of Pediatrics, People's Hospital of Linquan County, Anhui Province, China, from January 2019 to January 2022.
Methodology: Clinical data of 71 children with KD were retrospectively analysed, including 31 in the CAL group and 40 in the non-CAL group. The age, gender, days of fever, blood routine, plasma N-terminal B-type natriuretic peptide (NT-proBNP), and Kobayashi score were registered as independent variables of all the children, and the presence or absence of CAL was used as the dependent variable. All the independent variables were subjected to univariate analysis between the groups, and those with significance in univariate analysis were further subjected to unconditional binary logistic regression analysis. A receiver operating curve (ROC) was drawn to analyse the predictive power and optimal cut-off value of related risk factors for CAL.
Results: On univariate analysis, age, NT-proBNP and Kobayashi's score were closely related to CAL (all p<0.05). Multivariate analysis showed that NT-proBNP and Kobayashi scores were independent risk factors for CAL in children with KD. ROC curve analysis showed that the area under the curve (AUC) of NT-proBNP and Kobayashi scores were 0.771 and 0.732, respectively, at optimal critical values of 543.12 ng/L and 7.50 points, respectively.
Conclusion: The frequency of CAL in children with KD is high. NT-proBNP and Kobayashi scores are independent risk factors for the occurrence of CAL in children with KD, and they have good predictive performance for the diagnosis of CAL.
Key Words: Kawasaki disease, Children, Coronary artery lesion, Risk factors, Kobayashi score, NT-pro BNP.
INTRODUCTION
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is a systemic non-specific vasculitis that occurs in the infants and children, mainly involving small and medium blood vessels. The main clinical symptoms are fever, mucositis, and rash. Coronary artery lesion (CAL) is the most serious complication.1 The incidence of KD has been on the rise, and it is one of the most common causes of childhood-acquired heart disease in the developing countries. It has replaced rheumatic fever as the most common cause of childhood-acquired heart disease in developed countries.2
Although the comprehensive treatment of KD based on high-dose intravenous immunoglobulin (IVIG) has been widely implemented, the incidence of KD, especially CAL, is still high.3
Once CAL occurs, especially the occurrence of coronary artery aneurysm, it often leads to thrombosis and intimal thickening in the coronary artery lumen which leads to severe coronary artery stenosis, severe myocardial ischemia, even infarction, and sudden death, resulting in poor long-term prognosis. An early diagnosis of CAL in KD patients, especially the identification of independent risk factors of CAL in KD patients, and early intervention have important clinical significance. The purpose of this study was to observe the general clinical characteristics of children with KD and to analyse independent risk factors for the onset of CAL.
METHODOLOGY
A retrospective analysis was made of 71 children with KD (45 boys and 26 girls) clinically diagnosed in the Department of Pediatrics, People's Hospital of Linquan County, Anhui Province, China, from January 2019 to January 2022, ranging in age from 3 months to 11 years with an average of (22.73±7.05) months. Inclusion criteria were all the patients who met the diagnostic criteria of the 6th revision of Kawasaki disease diagnostic guidelines4 issued by the Scientific Committee of the Japanese Circulatory Society, age ≤14 years.
Table I: Univariate analysis affecting the occurrence of CAL [(x±s), cases (%)].
|
Parameter |
CAL group (n=31) |
Non-CAL group (n=40) |
t/χ2 |
p |
|
Gender (male / female) n (%) |
18(58.06)/13(41.94) |
27(67.50)/13(32.50) |
0.670 |
0.413 |
|
Age (m) |
30.65±7.15 |
18.60±5.15 |
8.255 |
<0.001 |
|
WBC (109·L-1) |
18.55±5.30 |
17.00±4.88 |
1.278 |
0.205 |
|
PLT (109·L-1) |
315.50±95.65 |
355.65±125.55 |
1.478 |
0.144 |
|
HB (g·L-1) |
110.55±12.65 |
109.80±10.55 |
0.272 |
0.786 |
|
CPR (mg·L-1) |
77.65±26.55 |
66.50±21.35 |
1.962 |
0.054 |
|
ESR (mm·h-1) |
75.56±23.50 |
73.25±29.80 |
0.354 |
0.724 |
|
NT-proBNP (ng·L-1) |
950.33±135.66 |
355.85±87.50 |
22.370 |
<0.001 |
|
Kobayashi score (points) |
7.66±1.50 |
6.25±1.05 |
4.656 |
<0.001 |
|
p: χ2 test was used for gender,and Student's t-test was used for other parameters. |
||||
Table II: Multivariate logistic regression analysis of CAL in patients with KD.
|
Parameter |
β |
SE |
Wald |
OR |
95%CI |
p |
|
Age (m) |
0.072 |
0.053 |
1.826 |
1.075 |
0.968~1.193 |
0.177 |
|
NT-proBNP (ng·L-1) |
0.011 |
0.003 |
11.403 |
1.011 |
1.004~1.017 |
0.001 |
|
Kobayashi score (points) |
0.854 |
0.280 |
9.267 |
2.348 |
1.355~4.068 |
0.002 |
All the patients were diagnosed with KD for the first time and were admitted within 10 days of onset. Exclusion criteria were patients with a history of IVIG and adrenocortical hormone treatment 3 months before admission, any infectious diseases in the past month, other immune diseases, incomplete data, and those who did not cooperate or agree to participate in this study.
Philips EPIQ5 ultrasonic diagnostic instrument with a probe frequency of 3.5 to 8.0 MHz was used for echocardiography. The children were taken from the left side, and the echocardiography was performed in a quiet or sleeping state. The internal diameter of each heart chamber, the flow velocity of each valve, and the cardiac function were routinely detected, and the coronary artery was mainly observed. Coronary arteries were evaluated using the Z-score recommended in the guidelines for the diagnosis and management of cardiovascular sequelae of Kawasaki disease (JCS/JSCS2020) issued by the Japanese Society of Circulation and the Japanese Society of Cardiac Surgery in July 2020.5 These diagnostic criteria are no lesions = Z value <2, coronary artery dilatation = 2≤Z value <2.5, or Z value <2, Z value decreased by more than 1 during follow-up; small coronary aneurysm = 2.5≤Z value <5; medium coronary aneurysm: 5≤Z value <10; and Giant coronary aneurysm: Z value ≥10. Where Z value ≥2.5 it was defined as CAL.
KD combined with CAL was evaluated according to the Kobayashi score system proposed by Kobayashi in 2006.6 The components are aspartate aminotransferase (AST) >100U/L (2 points); serum sodium ≤133mmol/L (2 points); blood neutrophil percentage ≥80% (2 points); IVIG treatment started within 4 days of the course of the disease (2 points); age <12 months (1 point); C-reactive protein ≥100 mg/L (1 point); and platelets ≤300×109/L (1 point). The total score is 11 points and ≥7 points are considered as high-risk for CAL.
The patient-related clinical data were accessed through the electronic case system, and the patient's age, gender, days of fever, plasma NT-proBNP, CPR, and other laboratory test results on admission as well as Kobayashi's score results were entered into the Excel table and double-entered for error correction. The patients were divided into a CAL group and a non-CAL group according to whether CAL occurred or not and the differences in the related indicators between the two groups were compared, and those with statistically significant differences were further analysed by unconditional binary logistic regression.
The IBM-SPSS 26.0 software package was used for data analysis. Measurement data were expressed as x±s and statistically analysed by the Student's t-test of two independent samples. Categorical data were described by the counts and percentages and analysed by the χ2 test. Unconditional binary logistic regression analysis was used for multivariate analysis. The diagnostic value of NT-proBNP, CPR, and Kobayashi score were analysed by the ROC curve. p<0.05 was considered the test level.
RESULTS
The differences in general clinical data, laboratory tests, and Kobayashi scores were compared between the CAL group and the non-CAL group. The results showed that age, NT-proBNP, and Kobayashi scores were closely related to CAL (all p<0.05, Table I).
The meaningful variables of the above univariate analysis (age, NT-proBNP, and Kobayashi score) were taken as independent variables, and then the occurrence of cal events (occurrence was 1, non-occurrence was 0) was taken as dependent variables for unconditional binary logistic regression analysis. The stepwise backward method was used to fit the optimisation model for analysis. The results showed that NT-proBNP (OR=1.011, 95% CI: 1.004 ~ 1.017, p=0.001) and Kobayashi score (OR=2.348, 95% CI: 1.355 ~ 4.068, p=0.002) were independent risk factors for CAL in children with KD (OR >1, p<0.05). The results are shown in Table II.
Draw the ROC curve of NT-proBNP and Kobayashi's diagnostic score showing that the AUC areas of NT-proBNP and Kobayashi's score are 0.771 and 0.732, respectively. PNT-proBNP <0.001 and PKobayashi's score = 0.001, as shown in Figure 1. According to the Youden index, the optimal critical values were 543.12 ng / L and 7.50 points, respectively. The sensitivity was 51.6% and 45.2% respectively, and the specificity was 92.5% and 87.5%, respectively.
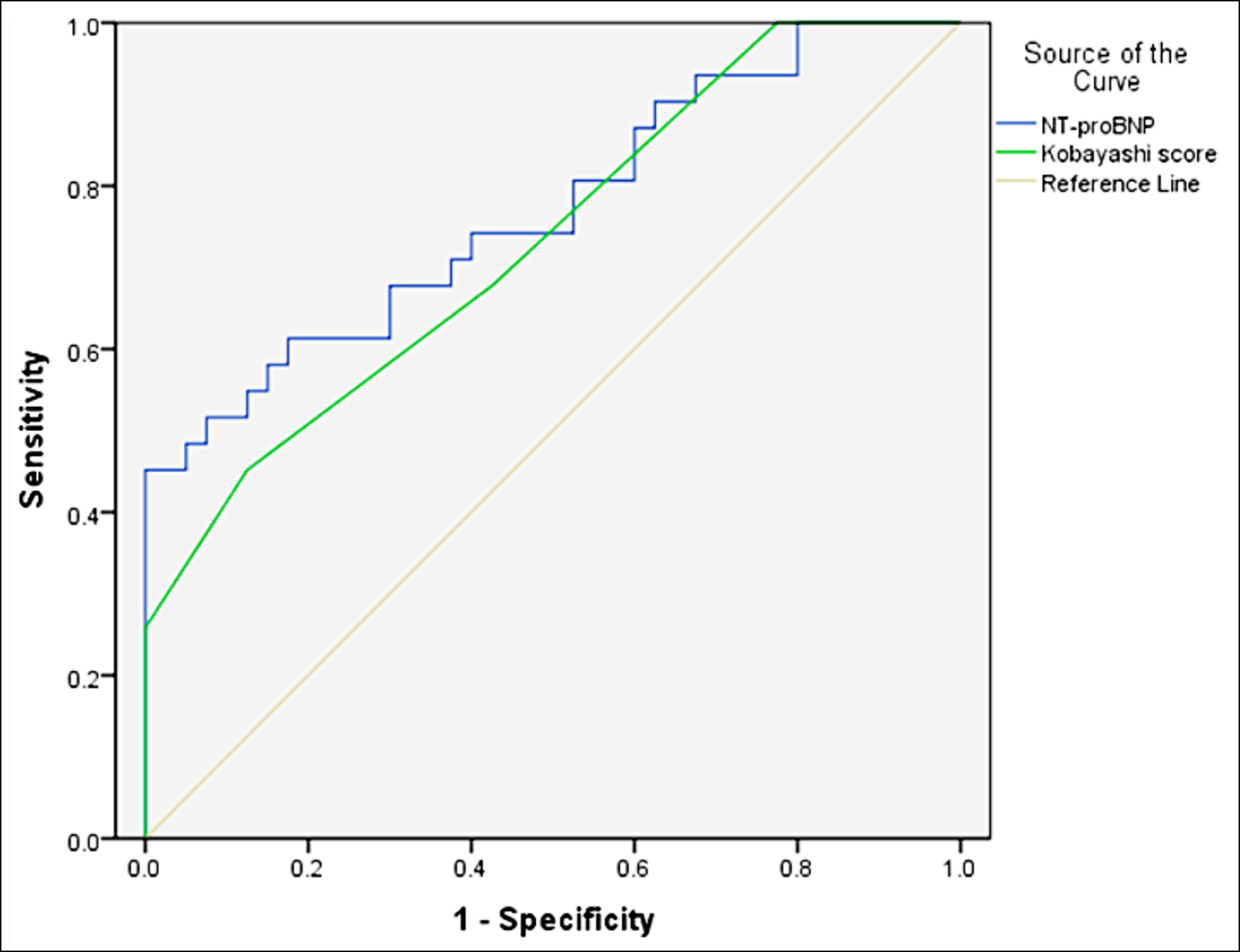 Figure 1: ROC curve of NT-proBNP and Kobayashi score in the diagnosis of children with KD complicated with CAL.
Figure 1: ROC curve of NT-proBNP and Kobayashi score in the diagnosis of children with KD complicated with CAL.
DISCUSSION
KD is one of the common causes of acquired heart disease in infants and young children. It can occur in both boys and girls. The incidence rate is about 1.3 to 1.5:1, and 80% to 85% of the children are younger than 5 years old.7 The ratio of males to females in this study was 1.73:1 of which 95.77% (68/71) of the children occurred within the age of 5 which is basically consistent with the epidemiological survey at home and abroad.8,9 Severe coronary artery inflammation sometimes causes dilation or aneurysm of the heart's arteries in the acute phase. In the early stage of the disease, CAL with KD is mainly coronary artery dilatation which is mainly manifested as coronary artery aneurysm. If the inner diameter of the aneurysm is excessively enlarged, it may lead to rupture or thromboembolism, leading to acute myocardial infarction and even sudden death. After the acute phase of KD, the CAL gradually narrows, and the intimal thickening results in luminal stenosis. However, progressive intimal thickening can lead to stenotic lesions and if clinically apparent, can lead to peripheral myocardial ischemia. CAL has typically complex hemodynamics due to the presence of mixed or dilated lesions and stenotic lesions. Endothelial dysfunction, decreased vascular elasticity, elevated levels of high-sensitivity C-reactive protein, oxidative stress, and elevated levels of inflammatory factors have been reported in late KD.10
The results showed that the increase of serum NT-proBNP expression level and Kobayashi score were independent risk factors for CAL in children with KD. Further ROC scoring showed that the diagnostic efficacy of serum NT-proBNP expression level and Kobayashi score for CAL in children with KD were 0.771 and 0.732, respectively. At that time, the best critical values of the two were 543.12 ng / L and 7.50, respectively. Although the sensitivity was general (51.6% and 45.2% respectively), it had high specificity (92.5% and 87.5%).
This study examined the relationship between early serum NT-proBNP and CAL in children with KD. It showed that the patients with elevated NT-proBNP may be at an increased risk for coronary artery disease if NT-proBNP levels are significantly elevated. The mechanism by which serum NT-proBNP levels are elevated in KD patients is unclear, but two possibilities have been proposed. One possibility is local myocardial inflammation or an area of ischemia. During the acute phase of KD, the pericardium, myocardium, endocardium, and coronary arteries may be involved.11 Another possibility is the involvement of cytokines that stimulate BNP secretion. It is known that tumor necrosis factor α, interleukin (IL)-1α, IL-1β, and interferon-γ exist in the acute phase of KD,12-14 and the involvement of cytokines often leads to coronary endothelial cell dysfunction.15 However, the relevant mechanisms of CAD and NT-proBNP have not been clearly defined. Kaneko et al. reported that when the serum NT-proBNP expression level was 1000 ng/L, the sensitivity and specificity of diagnosing KD with CAL were 83% and 68%.16 In the present study, the value of NT-proBNP was relatively low, probably because we detected it early in KD. Jung et al. detected the serum NT-proBNP expression level in hyperacute KD patients and showed that the cut-off value was 515.4 pg/ml, and the sensitivity and specificity were 78.26% and 61.63%, respectively.11
The Kobayashi score combines the patient's age, serum transaminases, neutrophil levels, CPR, and IVIG treatment. Kobayashi score to evaluate KD patients, who started IVIG treatment, showing the sensitivity and specificity for diagnosing CAL as 86% and 67%, respectively.6 The risk of developing CAL in KD patients is associated with IVIG resistance and high-risk patients, as determined by the scoring system, are generally considered to also have a higher risk of CAL.17 This difference in score performance can be attributed to the low incidence of coronary artery abnormalities in high-risk patients.18 Friedman et al. reported that the patients receiving IVIG plus anti-inflammatory drugs such as corticosteroids or infliximab had a higher rate of abnormal coronary regression than patients receiving other treatments.19 Previous studies have shown that a longer interval from onset to treatment is one of the important independent risk factors associated with abnormal coronary development.20 In this study, the median disease days at diagnosis were 4.5 days and early therapeutic intervention may account for the lower incidence of coronary abnormalities.
There are still some limitations in this study. On the one hand, as it’ s a single centre study, the incidence rate of CAL and its influencing factors among KD children in different regions are unknown. On the other hand, as a retrospective study, selective bias could not be completely avoided. The sample size of this study is relatively small; therefore, the future multi-centre and large sample survey may be more beneficial to the research results of CAL in KD patients.
CONCLUSION
Even with early and standard application of IVIG in the treatment of KD, the occurrence of CAL is not uncommon, especially for the patients with increased expression of serum NT-proBNP and high Kobayashi score in the early stage. CAL surveillance should be as highly vigilant as possible in these children.
PATIENTS’ CONSENT:
Written informed consents were obtained from all the patients.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
BB: Funds management, research design, statistical analysis, and article writing.
JLY: Treatment, personnel coordination, and postoperative follow-up.
CY: Funds management, research design, and article writing.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Stijn DV, Korbee JM, Netea SA, Winter VCD, Winderman KAH, Kuipers IM, et al. Treatment and coronary artery aneurysm formation in kawasaki disease: A per-day risk analysis. J Pediatr 2021; S0022-3476(21)01261-0. doi: 10.1016/j.jpeds.2021.12.054.
- Shi H, Weng FF, li C, Jin ZY, Hu JY, Chu MP, et al. Overweight, obesity and coronary artery lesions among Kawasaki disease patients. Nutr Metab Cardiovasc Dis 2021; 31(5):1604-12. doi: 10.1016/j.numecd.2021.01.015.
- Lee ZM, Chu CL, Chu CH, Chang LS, Kuo HC. Multiple intravenous antibiotics usage is associated with intravenous immunoglobulin resistance in Kawasaki disease. Pediatr Neonatol 2021; 63(2):S1875-9572(21) 00180-7. doi: 10.1016/j.pedneo.2021.06.020.
- Kobayashi T, Ayusawa M, Suzuki H, Abe J, Ito S, Kato T, et al. Revision of diagnosticguidelines for Kawasaki disease (6th revised edition). Pediatr Int 2020: 62(10):1135-8. doi: 10.1111/ped.14326.
- Fukazawa R, Kobayashi J, Ayusawa M, Hamada H, Miura M, Mitani Y, et al. JCS/JSCS 2020 guideline on diagnosis and management of cardiovascular sequelae in Kawasaki disease. Circ J 2020; 84(8):1348-407.doi: 10.1253/circj. CJ-19-1094.
- Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, et al. Prediction of intravenous immuno-globulin unresponsiveness in patients with Kawasaki disease. Circulation 2006; 1(22):2606-12. doi: 10.1161/ CIRCULATIONAHA.105.592865.
- Tsuda E, Hamaoka K, Suzuki H, Sakazaki H, Murakami Y, Nakagawa M, et al. A survey of the 3-decade outcome for patients with giant aneurysms caused by Kawasaki disease. Am Heart J 2014; 167(2):249-58. doi: 10.1016/j.ahj.2013. 10.025.
- Kuwabara M, Yashiro M, Kotani K, Tsuboi S, Ae R, Nakamura Y, et al. Cardiac lesions and initial laboratory data in Kawasaki disease: A nationwide survey in Japan. J Epidemio 2015; 25(3):189-93. doi: 10.2188/jea.JE20140128.
- Zhang X, Zhang Z, Liu SC, Sun JH. Epidemiologic survey of Kawasaki disease in Jilin from 1999 through 2008. Pediatr Cardiol 2012; 33(2):272-9. doi: 10.1007/s00246-011- 0121-7.
- Watanabe M, Fukazawa R, Ogawa S, Ohkubo T, Abe M, Hashimoto K, et al. Virtual histology intravascular ultrasound evaluation of coronary artery lesions within 1 year and more than 10 years after the onset of Kawasaki disease. J Cardiol 2020; 75(2):171-6. doi: 10.1016/j.jjcc. 2019.06.015.
- Jung JY, Ham EM, Kwon H, Kwak YH, Kim DK, Lee JH, et al. N-terminal pro-brain natriuretic peptide and prediction of coronary artery dilatation in hyperacute phase of Kawasaki disease. Am J Emerg Med 2019; 37(3):468-71.doi: 10.1016/j.ajem.2018.06.021.
- Weng HB, Pei QF,Yang ML, Zhang J, Cheng ZL, Yi QJ, et al. Hypomethylation of C1q/tumor necrosis factor-related protein-1 promoter region in whole blood and risks for coronary artery aneurysms in Kawasaki disease. Int J Cardiol 2020; 307:159-63. doi: 10.1016/j.ijcard.2020. 02.002.
- Kone-Paut I, Cimaz R, Herberg J, Bates O, Carbasse A, Saulnier JP, et al. The use of interleukin 1 receptor antagonist (anakinra) in Kawasaki disease: A retrospective cases series. Autoimmun Rev 2018; 17(8):768-74. doi: 10.1016/j. autrev.2018.01.024.
- Hu P, Jiang GM, Wu Y, Huang BY, Liu SY, Zhang DD, et al. TNF-α is superior to conventional inflammatory mediators in forecasting IVIG nonresponse and coronary arteritis in Chinese children with Kawasaki disease. Clin Chim Acta 2017; 471:76-80. doi: 10.1016/j.cca.2017.05.019.
- Xu MG, Qi Q, Men L, Wang SS, Li M, Xiao M, et al. Berberine protects Kawasaki disease-induced human coronary artery endothelial cells dysfunction by inhibiting of oxidative and endoplasmic reticulum stress. Vascul Pharmacol 2020; 127:106660. doi: 10.1016/j.vph.2020.106660.
- Kaneko K, Yoshimura K, Ohashi A, Kimata T, Shimo T, Tsuji S. Prediction of the risk of coronary arterial lesions in Kawasaki disease by brain natriuretic peptide. Pediatr Cardiol 2011; 32(8):1106-9. doi: 10.1007/s00246-011- 9986-8.
- Huang CN, Wu FF, Chang YM, Huang HC, Lin MT, Wang JK, et al. Comparison of risk scores for predicting intravenous immunoglobulin resistance in Taiwanese patients with Kawasaki disease. J Formos Med Assoc 2021; 120(10): 1884-9. doi: 10.1016/j.jfma.2020.12.010.
- Miyata K, Miura M, Kaneko T, Morikawa Y, Matsushima T, Sakakibara H, et al. Evaluation of a Kawasaki disease risk model for predicting coronary artery aneurysms in a Japanese population: An analysis of post raise. J Pediatr 2021; 237:96-101.e3. doi: 10.1016/j.jpeds.
- Friedman KG, Gauvreau K, Hamaoka-Okamoto A, Tang A, Berry E, Tremoulet AH, et al. Coronary artery aneurysms in Kawasaki disease: Risk factors for progressive disease and adverse cardiac events in the US population. J Am Heart Assoc 2016; 5(9):e003289. doi: 10.1161/JAHA.116.003289.
- Downie ML, Manlhiot C, Collins TH, Chahal N, Yeung RSM, McCrindle BW. Factors associated with development of coronary artery aneurysms after Kawasaki disease are similar for those treated promptly and those with delayed or no treatment. Int J Cardiol 2017; 236:157-61.doi: 10.1016/j.ijcard.2017.01.068.