A Statistical Model for Early Recognition of Patients Requiring Transfer to Palliative Care (ERPAC)
By Cihangir Dogu1, Ayse Muge Karcioglu2, Isil Ozkocak Turan3, Handan Ankarali4Affiliations
doi: 10.29271/jcpsp.2023.03.261ABSTRACT
Objective: To develop a scoring system to identify patients at an early stage who will need palliative care during intensive care follow-up.
Study Design: Analytical study.
Place and Duration of Study: Ankara City Hospital, Neurology and Orthopaedics Hospital, General Intensive Care Unit, Ankara, Turkiye, from June 2019 to March 2020.
Methodology: Intensive care patients were enrolled and divided into palliative care transfer (p1) and nontransfer groups (p2). The predicted logit value / probality score was calculated and a scoring system was developed, using the formula value, [logit= -3.275 + 0.194 (days of hospitalisation) - 0.345 (SOFAmax) +1.659 (ward admission) + 2.08 (cancer)].
Results: One hundred and thirty five patients were analysed. Sixty-eight (50.4%) were males. The mean age was 67.2 ± 17.2 years. Length of hospital stay (p<0.001), highest sequential organ failure score (SOFAmax, p<0.001), previous hospitalisation (p=0.015), and cancer history (p=0.009) affect the need for palliative care significantly.
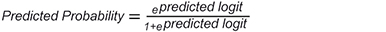
Predicted probability = epredicted togit / 1+epredicted logit
If predicted probabilty >0.5, patient was candidate for palliative care transfer.
Conclusion: Every intensive care unit can calculate its own logit value and represent ERPAC score. ERPAC scores can predict which patients will be transferred to palliative care. Predictedlogit value will help to recognise which patients will need palliative care at an early stage.
Key Words: Palliative care, Scoring, Intensive care.
INTRODUCTION
Palliative care is patient- and family-centred care designed to prevent pain and optimise quality of life through comprehensive assessment of incurable patients, regardless of their age, diagnosis or prognosis.1 In one study, stressful symptoms were observed in 27-75% of intensive care patients. Delirium was observed in approximately one-third of these patients.2
Similarly, in addition to physical and emotional symptoms, 57% of younger relatives of patients had traumatic stress and 70-80% had symptoms of anxiety and depression.3
Palliative care assessment should be initiated as early as possible to minimise the suffering and to allow for solution-oriented interventions. In a study evaluating patients with stage IV non-small cell lung cancer, patients receiving palliative care were shown to have easier symptom management and longer survival.4 Between 14-20% of intensive care patients are estimated to be ready for palliative care processes.5
In the past four decades, despite the fact that advanced organ support systems in intensive care units have ensured the survival of critically ill patients,6 mortality rates did not fall below 20%. The occupancy rates of intensive care beds did not decrease as they become more valuable with the ageing of the population.7 The fact that there are patients who will not benefit from treatment in these beds despite advanced support negatively affects the length of hospitalisation, related costs and the number of patients who could otherwise use these beds.8 If patients to be transferred to palliative care can be recognised early, there will be a rapid turnover of these beds. A scoring system that can help identify palliative care transfers has not been previously reported in the literature. Villa et al. studied a scoring system for patients who would benefit from palliation, but the transfer of these patients from intensive care was not considered in that study.9
This study aimed to develop a scoring system that can identify patients who will need palliative care after intensive care treatment at an early stage, organise appropriate palliative care for these patients and utilise intensive care beds with maximum efficiency.
METHODOLOGY
This single-centred analytical study was conducted in the general intensive care unit of the Orthopaedics- and Neurology Tower of Ankara City, Hospital between June 2019 and March 2020 after obtaining ethics committee approval (number 28/3/2019-2636).
Adult patients of either gender who received treatment in intensive care for more than 48 hours were included in the study. Intoxications, postoperative patients, patients younger than 18 years, and patients transferred from palliative care to intensive care were excluded from the study.
Both surgical and medical intensive care patients were treated in that unit. Upon admission, demographic characteristics, intensive care unit admission diagnosis, acute physiology and chronic health evaluation II (APACHE II) score, sequential organ failure assessment (SOFA) scores, co-morbidities, previous ward admission, previous intensive care unit admission, tracheostomy, and nursing home admission status of the patients were recorded. Daily SOFA scores, sedation time, intubation time, mechanical ventilation time, respiratory failure, heart failure, renal dysfunction, hepatic dysfunction, coagulation disorder, vasoactive support, renal replacement therapy periods, platelet, fresh frozen plasma, erythrocyte replacements, number of days with sepsis, and days during which antibiotherapy was received and antibiotherapy changes were recorded by the investigators every day during the intensive care stay. Patients treated in the intensive care unit and who were not suitable for transfer to the ward or rehabilitation were included in the palliative group. Patients were divided into two groups as (n=47) patients, who were transferred to palliative care (P1) and (n=88) patients who were not transferred to palliative care (P2). Patients who were to be transferred to palliative care but could not be transferred due to the lack of consent of the patient's relatives or lack of space in palliative care were also included in the palliative care group.
The endpoint of the study was to predict the transfer of patients whose intensive care treatment ended to palliative care by using a scoring system.
When the data obtained at the end of the study were analysed, 47 patients were found to have been transferred to palliative care, 62 patients were transferred to the ward, and 26 patients had died. Since there were more than 25 subjects in each group, minimum sample size was reached. In addition, when the patients were categorised as those who died, who received palliative care and who were taken to the ward and these were compared for SOFA and APACHE scores,the patients who received palliative care were in the middleand significantly better than the patients who died. This result shows that the study was conducted with a sufficient sample size that can distinguish patients receiving palliative care from deceased patients and patients admitted to the ward.
The normality assumption of numerical variables was checked with the Shapiro-Wilk test and it did not show normal distribution. Descriptive statistics of the data were given as mean, standard deviation (SD), median (25th and 75th quartiles), and frequencies as count and percentage according to the types of variables. First of all, the relationships between the groups and the variables were evaluated with univariate tests. To this end, the relationships between categorical variables and groups were investigated by Pearson chi-square test or Fisher Exact test. The differences between groups with regard to numerical variables was evaluated by Mann-Whitney U test. In the second step, all variables influencing palliative care transfer were investigated by the multiple binary logistic regression model with the forward variable selection method.The predicted logit values of the patients were calculated from the coefficients in the final model and these values were converted into predicted probability values (*). These values are between 0 and 1. The cut-off value is accepted as 0.5. For patients with a probability value of above 0.5, a recommendation was provided to be sent to palliative care. However, if the sample sizes in the groups differ from each other, the cut-off value may differ from 0.5. For this reason, the cut-off value that discriminates the groups in the best way should be examined with the ROC curve. In this study, the sample size ratio (non-candidate/candidate for palliative care) is 1.9. Predicted probability values named as ERPAC. The level of statistical significance was accepted as lower than 0.05 and IBM Corp. Released 2013. IBM SPSS for Windows, Version 22.0 (Armonk, NY:IBM Corp, USA) was used for data analysis.
RESULTS
The primary outcome of study was to predict patients to be transferred to palliative care during intensive care follow-up. While 299 patients were treated in the intensive care unit, 135 patients met the inclusion criteria. Sixty-eight (50.4%) of these patients were males and sixty-seven (49.6) were females. The mean age was 67.2 ± 17.2 years, the mean APACHE II score was 17.9 ± 7.9, and the average length of stay was 18.41 ± 18.42 days. Forty-seven (34.8%) patients were in the group with palliative care indication (P1), and 88 (65.2%) in the group without palliative care indication (P2, Figure 1).
Among the study parameters, median mechanical ventilation period (p<0.001),intubation period (p=0.008), parenteral nutrition period (p=0.006), antibiotherapy period (p<0.001), and oxygen supplementation period (p<0.001) were significantly higher in group P1. When the study groups were compared for comorbidities, gastrostomy (p=0.001), cancer (p=0.013), and previous intensive care admission (p=0.032) were significantly higher in group P1.
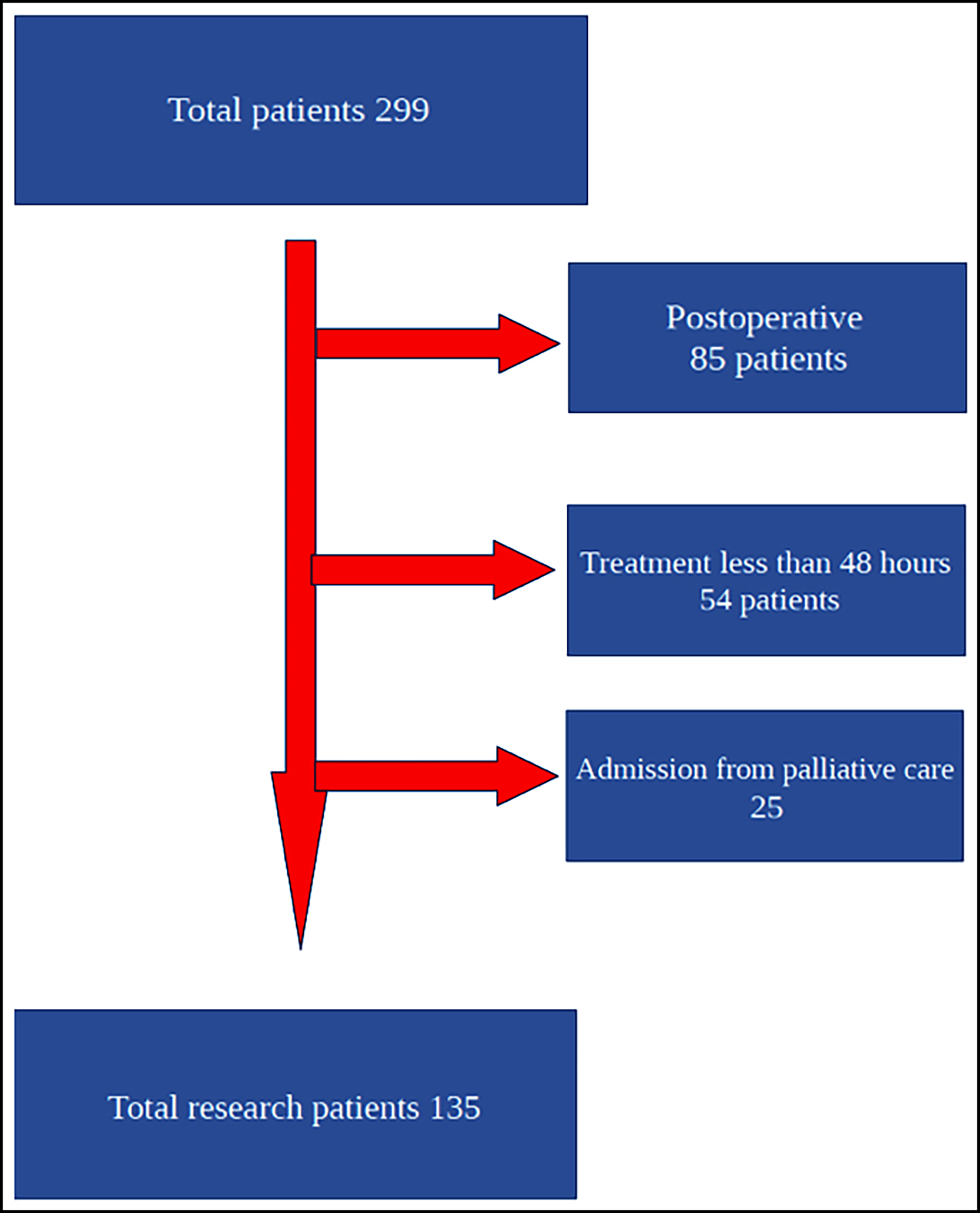 Figure 1: Flowchart.
Figure 1: Flowchart.
Table I: Model results and coefficients to predict patients to be transferred to palliative care.
|
|
B |
S.E. |
Wald |
df |
P |
OR |
|
Length of stay |
0.194 |
0.037 |
27.511 |
1 |
<0.001 |
1.214 |
|
Maximum SOFA |
-0.345 |
0.098 |
12.500 |
1 |
<0.001 |
0.708 |
|
Previous ward admission |
1.659 |
0.681 |
5.934 |
1 |
0.015 |
5.255 |
|
Cancer (yes/no) |
2.080 |
0.795 |
6.838 |
1 |
0.009 |
8.003 |
|
Constant Term |
-3.275 |
0.819 |
15.997 |
1 |
<0.001 |
0.038 |
The final model established to predict patients to be transferred to palliative care is given below, details of the model are presented in Table I.
It was determined that the effect of four variables was significant in determining the patients who would receive palliative care.
Predicted Logit = -3.275 + 0.194 (Hospitalisation Day) - 0.345 (SOFAmax) +1.659 (Hospital Admission) + 2.08 (Cancer)
Predicted logit values were converted to predicted probabilities by using the formula:

If the probability value is between 0 and 1 and this value is greater than 0.5 (50%), it would be appropriate to transfer the patient to palliative care. When the compatibility of the actual results with this classification based on the model was examined, the model performance criteria were obtained (Table II).
When the cut-off value of the predicted probabilities was accepted as 0.5, 81 of 88 patients in the P2 group were correctly estimated with the model (specificity = 92%), and 35 of 47 patients in the P1 group were correctly estimated with the model (sensitivity = 74.5%). In addition, the positive predictive value of the model was calculated as 83.3% and overall accuracy value as (35 + 81) / 135 = 85.9%.
The results of the model's success in palliative care transfer estimation with ROC curve are shown in Figure 2.
When the cut-off value for predicted probabilities was examined with ROC analysis, values between 0.35 and 0.5 were found suitable. When the cut-off was taken as 0.35, the sensitivity was higher (increased up to 85%), but the specificity was lower (decreased to 87.5%) compared to the cut-off 0.50. AUC=0.932, SE for AUC = 0.021.
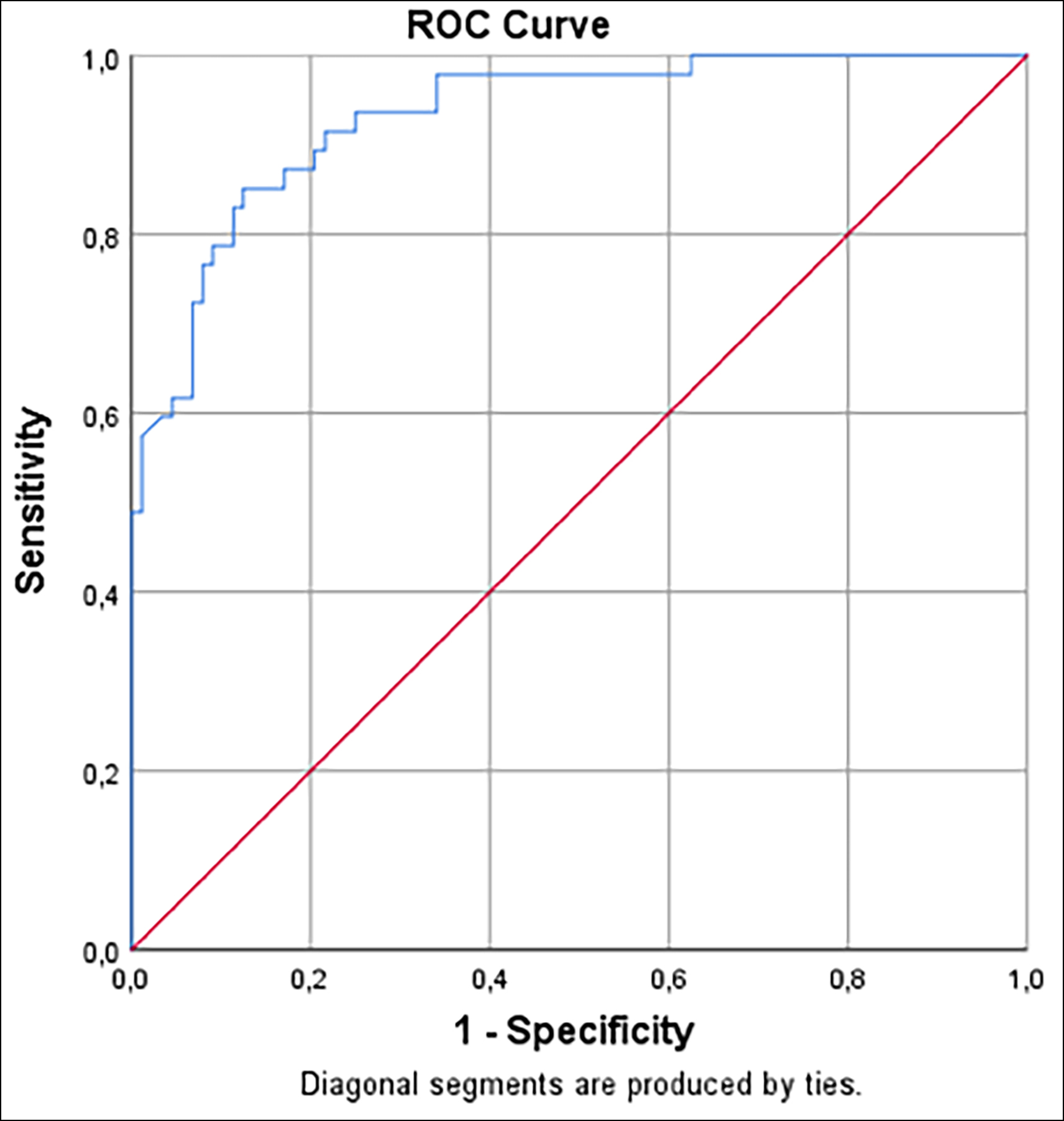 Figure 2: The power of the model created to predict the P1 group.
Figure 2: The power of the model created to predict the P1 group.
DISCUSSION
In this study, the Predicted Logit developed as = -3.275 + 0.194 (days of hospitalisation) - 0.345 (SOFAmax) +1.659 (ward admission) + 2.08 (cancer) to predict patients candidates for palliative care. The logit values calculated from the model were converted into probabilities using the equation "Logit = log (p/(1-p))" and a standard score was obtained. Those with a probability value of 0.5 and above should be referred to palliative care. The specificity and sensitivity of the method were found as 92% and 74%, respectively. Its effectiveness was also demonstrated in the ROC analysis performed for the unit.
Table II: The success of the model, which was established by significant effects among all variables.|
|
True result |
Total |
||||||
|
P1 |
P2 |
|||||||
|
n |
% within Row |
% within Column |
n |
% within Row |
% within Column |
n |
||
|
Results of final model |
P1 |
35 |
83.3 |
74.5 |
7 |
16.7 |
8.0 |
42 |
|
P2 |
12 |
12.9 |
25.5 |
81 |
87.1 |
92.0 |
93 |
|
|
Total |
47 |
34.8 |
100.0 |
88 |
65.2 |
100.0 |
135 |
|
The available literature presents no scoring system that predicts the need for palliative care transfer in patients treated in intensive care. In the study by Villa et al., the aim was to predict patients who could not be treated and to provide palliation.9 In that study, the researchers did not aim to predict the patients who would need long-term care, but rather to identify the patients who would not benefit from intensive care treatment and who would die and to provide them palliation. In addition, the logit value of the model was given as the score value in that study. However, the logit value is influenced by the type, unit of measurement and data structure of the variables and changes greatly. The logit values suggested as scores in the study may take values in completely different ranges in different data even with the same variables. Therefore, the cut-off value is only valid in its own patient group and cannot be applied to other cases. In this study, logit values were converted into probabilities and 0.5 was taken as the cut-off value. When the variables proposed in this study are used in future studies on the same subject, it is expected to yield similar results.
The mean age of the study population was 66 years. With the ageing of the society, the geriatric population in adult intensive care units is on the rise. In a previous study in which evaluated patients who underwent orthopaedic surgery, the mean age was found to be 68 years.10 In the study by Zimmerman et al., the mean age was 60 years.11 The fact that their study was conducted on cancer patients receiving palliation decreased their mean age. In this study, the mean age increased due to the lower number of oncological patients.
In this study, the length of intensive care stay, the SOFAmax value, previous ward admission and the presence of neoplasia were statistically effective in calculating the logit value. The need for palliative care increases by 1.21-folds with prolonged hospitalisation. In a retrospective study by Digwood et al., the length of stay in intensive care shortened after the opening of palliative care services.12 When there were available beds in palliative care wards and the reluctance of patients' relatives could be overcome, the average length of stay in intensive care could also be shortened. Palliative care consultations may reduce long intensive care stays and ensure more effective use of intensive care.
In a meta-analysis by Kyeremanteng et al. palliative care consultation was found to reduce intensive care unit length of stay and related costs.13
SOFA is a scoring system that shows deterioration in organ systems with six different parameters and is calculated daily in intensive care units. Serial SOFA follow-up has previously been reported to indicate intensive care unit mortality.14 Patients with high SOFA scores have high mortality rates and their transfer to palliative care would not be appropriate. In the study, increasing SOFAmax scores increased the transfer to palliative care by 0.70 times.
Being previously treated in the ward increases the likelihood of being transferred to palliative care 5.22 times compared to never being hospitalised. The fact that the patients were previously hospitalised due to chronic diseases causes an increase in the need for palliative care.
In the study, the presence of neoplasia increased the need for palliative care 8.33 times. In the study conducted by Arcanjo et al. in a geriatric unit, malignancy increased the need for palliative care 3.8 times.15
Postoperative and intoxication-related intensive care patients were not included in the study, which enabled the evaluation of the patient group that may need palliative care. Each intensive care unit can calculate its own evaluation score separately according to the logit calculation that was first proposed by analysing important variables in this patient group. In centres where neurology, geriatrics, orthopaedics and orthogeriatrics patients are treated more often, risk calculation can be made using the same logit value.
The biggest limitation of the study was terminating it earlier than it was planned due to the COVID-19 pandemic. If the planned period could have been adhered to, the study could have been conducted with a larger number of patients. Another limitation was that the tower, where the study was conducted was the hospital where orthopaedics, neurology, and infectious diseases clinics were located. The patient population followed up in oncology, haematology, and cancer surgery hospitals participated less in the study possibly causing longer hospitalisation.
CONCLUSION
Palliative care transfers can be estimated by logit calculation in intensive care units. By the help of ERPAC, the need for palliative care can be estimated. Intensive care occupancy rates can be reduced with such an approach.
The study was registered with the number of NCT04864613 in clinicaltrials.gov.
ETHICAL APPROVAL:
This study was approved by the Ankara Numune Research and Training Hospital ethics committee. Date: 28/3/2019, Number: 2636.
PATIENTS’ CONSENT:
Written informed consents were obtained from all patients.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
CD, IOT, AMK: Conceived and designed the study; wrote the manuscript.
CD, HA: Contributed to the analysis and interpretation of data.
CD, IOT, HA: Revised the manuscript.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Mercadante S. Gregoretti C. Cortegiani A. Palliative care in intensive care units: why, where, what, who, when, how. BMC Anesthesiol 2018; 18(1):106. doi: 10.1186/s12871- 018-0574-9.
- Puntillo KA, Arai S, Cohen NH, Gropper MA, Neuhaus J, Paul SM, et al. Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med 2010; 38(11):2155-60. doi: 10.1097/CCM.0b013e3181f267ee.
- McAdam JL, Dracup KA, White DB, Fontaine DK, Puntillo KA. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med 2010; 38(4):107885. doi: 10.1097/CCM.0b013e3181cf 6d94.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Eng J Med 2010; 363(8):733-42. doi:10.1056/NEJMoa1000678
- Hua MS, Li G, Blinderman CD, Wunsch H. Estimates of the need for palliative care consultation across united states ıntensive care units using a trigger-based model. Am J Respir and Crit Care Med 2014; 189(4):428–36. doi: 10.1164/rccm.201307-1229OC.
- Bertolini G, Boffelli S, Malacarne P, Peta M, Marchesi M, Barbisan C, et al. End-of-life decision-making and quality of ICU performance: An observational study in 84 Italian units. Intensive Care Med 2010; 36(9):1495–504. doi: 10.1007/ s00134-010-1910-9.
- Hartog CS, Peschel I, Schwarzkopf D, Curtis JR, Westermann I, Kabisch B, et al. Are written advance directives helpful to guide end-of-life therapy in the intensive care unit? A retrospective matched-cohort study. J Crit Care 2014; 29(1): 128-33. doi: 10.1016/j.jcrc.2013. 08.024.
- Ward N, Chong D. Critical care beds and resource utilization: Current trends and controversies. Semin Respir Crit Care Med 2015; 36(06):914-20. doi: 10.1055/s-0035- 1564876.
- Villa G, De Gaudio AR, Falsini S, Lanini I, Curtis JR. Development of END-of-Life ScorING-System to identify critically ill patients after initial critical care who are highly likely to die: A pilot study. Minerva Anestesiologica 2015; 81(12): 1318-28. doi: 10.1055/s-0035-1564876.
- Dogu C, Mehmet Mutlu N, Turan S, Karaca O, Kayir S, Ozkocak Turan I. Evaluation of risk factors and comorbidies of the orthopedic patients treated in intensive care unit. Acta Medica Mediterranea 2019; 35:2583-9. doi: 10.19193/ 0393-6384_2019_5_405.
- Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet 2014; 383(9930):1721-30. doi: 10.1016/S0140- 6736(13)62416-2.
- Digwood G, Lustbader D, Pekmezaris R, Lesser ML, Walia R, Frankenthaler M, et al. The impact of a palliative care unit on mortality rate and length of stay for medical intensive care unit patients. Palliative Supportive Care 2011; 9(4):387-92. doi: 10.1017/S147895151100040X.
- Kyeremanteng K, Gagnon LP, Thavorn K, Heyland D, D’Egidio G. The ımpact of palliative care consultation in the ICU on length of stay: A systematic review and cost evaluation. J Intensive Care Med 2018; 33(6):346-53. doi: 10.1177/ 0885066616664329.
- Ferreira FL. Serial evaluation of the sofa score to predict outcome in critically Ill patients. JAMA 2001; 286(14):1754. doi: 10.1001/jama.286.14.1754.
- Arcanjo SP, Saporetti LA, Curiati JAE, Jacob-Filho W, Avelino-Silva TJ. Clinical and laboratory characteristics associated with referral of hospitalised elderly to palliative care. Einstein (Sao Paulo) 2018; 16(1):eAO4092. doi: 10.1590/ s1679-45082018ao4092.