A Rare Complication of The Heart Rate Strap Use in A Marathon Runner: Mondor’s Disease of the Breast
By Tuba Selcuk Can, Turkan Uz IkizceliAffiliations
doi: 10.29271/jcpsp.2022.12.1623ABSTRACT
This is the first case report of Mondor’s disease diagnosed in a marathon runner developed due to tight heart rate strap. A 41-year-old female marathon runner was admitted to the hospital with a cord-like soft tissue swelling under her breast, which was confirmed by physical examination. She had a history of severe exercise; during which, she used a sports watch with a heart rate strap that she tightened under her bra. Doppler ultrasonography revealed a superficial non-compressible thrombosed vein compatible with Mondor’s disease.
Key Words: Mondor's disease, Ultrasonography, Heart rate strap.
INTRODUCTION
Mondor’s disease (MD) is a rare benign condition, characterised by self-limiting thrombophlebitis of the superficial veins. Although Charles Fagge first described it in Guy's Hospital Reports in 1870, the disease was named after Henri Mondor, who first reported the clinical series. It usually occurs in the thoracoabdominal superficial veins but can also occur in extremities, the inguinal region, and the penis.1 Trauma, physical stress, surgery, and tight clothing are reported as predisposing factors for MD.2 Recent immunochemical indicators have shown that MD mainly results from thrombophlebitis of superficial veins in many patients. In some cases, lymphangitis plays an essential role in the pathogenesis of the disease. A “cord-like” lesion occurs as a result of the connective tissue accumulation on the vessel wall right after the affected vein is occluded by the inflammatory cells and fibrin.3
We present a case of MD in a marathon athlete, which developed due to a tight heart rate strap. To our knowledge, such aetiology has never been reported before.
CASE REPORT
A 41-year-old female patient presented to the clinic with the complaint of a stiff and painful cord-like lesion under the right breast that began a few days ago. She had no other symptoms.
Her body mass index (BMI) was 19.6, and she was a non-smoker. She did not have any history of thrombophlebitis, breast surgery, or trauma. She did not take any medications (including oral contraceptives) other than antihistamines (desloratadine-montelukast) prescribed for allergic rhinitis. She reported a steady history of jogging for three days a week and had completed two long-distance races (38 km and 42.19 km-marathons) in the past 2 weeks. She reported regular use of a sports watch with a heart rate strap (Figure 1) that she tightened under her bra in order to prevent it from sliding due to sweating.
 Figure 1: The heart rate monitor chest band.
Figure 1: The heart rate monitor chest band.
On physical examination, a cord-like lesion starting at the right areola and extending down was noted. The lesion tended to be more apparent when she raised her arm (Figure 2a). No change in skin colour was present. It was painful during palpation. Laboratory results, including whole blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and D-dimer, were within normal range. Mammography (IMS Giotto MD digital mammography and Tomosynthesis, Bologna, Italy) and simultaneous sonography (Hitachi Medco’s Digital Ultra Sound Examination Device, HI VISION Avius, Tokyo, Japan) have been performed since the age of 41 years. Dense breast tissue was detected in mammography, and there were no pathological results. A long non-compressible surface vein was detected in the breast and surface tissue by ultrasound. Vascularisation was not present in the Color Doppler Ultrasonography (CDUS) (Figure 2b). The clinical and physical examination and imaging findings were compatible with MD. Conservative treatment with nonsteroidal anti-inflammatory drugs (NSAID) was started, and the fibrosed, cord-like, superficial vein that was visible and palpable, regressed completely in three weeks. Revascularisation was observed in the follow-up CDUS 6 weeks later.
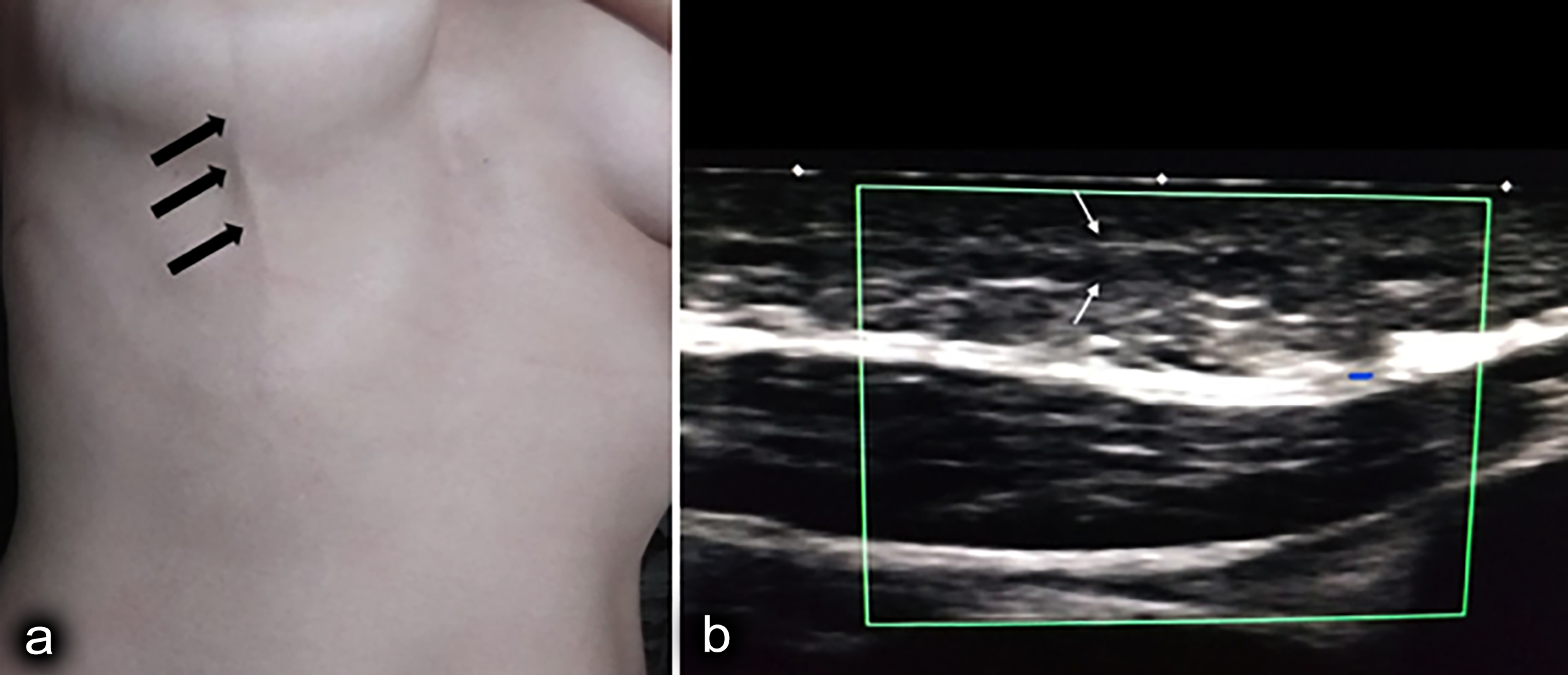 Figure 2: (a) The lesion became more apparent when she lifted her arm. (b) No vascularisation was detected in the Color Doppler Ultrasonography (CDUS).
Figure 2: (a) The lesion became more apparent when she lifted her arm. (b) No vascularisation was detected in the Color Doppler Ultrasonography (CDUS).
DISCUSSION
MD of the breast is a benign condition that is characterised by superficial thrombophlebitis of the breast veins. Affected veins include lateral, thoracoepigastric, and superior epigastric thoracic veins. In this case, the thoracoepigastric vein was affected. In accordance with this case, MD is three times more common in women compared to men. The pathophysiology of MD is still not fully understood. Although the aetiology is typically idiopathic, thromboembolic events, surgery, and trauma are reported as predisposing factors.4
Thromboembolic events due to severe exercise have been reported in the literature. Venous thrombosis of the lower extremities in several marathoners and deep venous thrombosis in a soccer player were reported.5 Rare axillary and anterior thoracoabdominal thrombophlebitis have been reported among bodybuilders.6 Similar pathophysiological mechanisms are responsible for these various exercise-related conditions. Temporary inflammatory condition is known to occur following severe exercise.7 These inflammatory processes trigger clotting and fibrinogenesis.8
Similarly, this case had a severe exercise history. This case has reported continued use of the heart rate strap in addition to lengthening his routine exercise schedule. Heart rate straps have adjustable bands. These bands are attached around the thorax to monitor the heart rate. Since the strap is made of rubber, these bands may become loose and slide down during jogging, which can cause false measurements and discomfort for the runner. This case also reported fastening the band and tightening it under her bra to prevent sliding. Deterioration of venous return and resultant venous stasis due to compression as well as severe exercise seemed to be the underlying mechanisms in this case.
The diagnosis of MD is usually made on clinical evaluation. Ultrasound and/or Doppler Ultrasound can be used for verification of diagnosis. The mammogram results of our case were normal, as stated in the literature.9
There is no consensus on the treatment of MD. Drug/hormone use should be stopped, and any underlying diseases should be treated. The presence of an underlying disease is reported to be rare in a recently published review.10 It usually heals and resolves spontaneously. NSAID use is recommended in case of pain and sensitivity, which was the case in the present report.5 Local heat application and loose bra use during the treatment period can be recommended.4
Diagnosis of MD can usually be made clinically. In order to prevent unnecessary clinical evaluations, a detailed history should be obtained, and it should be kept in mind that severe exercise can lead to this condition. With the recent developments in technology, monitoring equipments are widely used by athletes. This report suggests that the use of these types of equipment during severe exercises, such as marathons, can create a cumulative effect for the development of MD of the breast.
PATIENT’S CONSENT:
An informed consent was obtained from the patient for the publication of this case report.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
TUI: Conception, supervision, resources, literature search, and manuscript writing.
TSC: Design, analysis and/or ınterpretation, and manuscript writing.
All the authors have approved the final version of the manuscript to be published.
REFERENCES
- Godoy JM, Godoy MF, Batigalia F, Braile DM. The association of Mondor’s disease with protein S deficiency: A case report and review of literature. J Thromb Thrombolysis 2002; 13(3):187-9. doi: 10.1023/a:1020487225611.
- Amano M, Shimizu T. Mondor's disease: A review of the literature. Intern Med 2018; 57(18):2607-12. doi: 10.2169/ internalmedicine.0495-17.
- Alvarez-Garrido H, Garrido-Ríos AA, Sanz-Muñoz C, Miranda-Romero A. Mondor’s disease. Clin Exp Dermatol 2009; 34(7):753-6. doi: 10.1111/j.1365-2230.2009. 03430.x.
- Agus G. COVID-19 ERA: Mondor’s disease and rembrandt. What ties? Veins Lymphatics 2020; 9:23-4.
- Fleming A, Frey D. Extensive venous thrombosis in a runner. Phys Sportsmed 2005; 33(1):34-6. doi: 10.3810/ psm.2005.01.35.
- Talhari C, Mang R, Megahed M, Ruzicka T, Stege H. Mondor’s disease associated with physical strain: Report of 2 cases. Arch Dermatol 2005; 141(6):800-1. doi: 10.1001/ archderm.141.6.800.
- Hemsing AL, Reikvam H. Mondor's disease after extensive training with Nordic walking. Oxf Med Case Reports 2019; 28(8):356-8. doi: 10.1093/omcr/omz075.
- Tröbinger C, Wiedermann CJ. Bodybuilding-induced Mondor’s disease of the chest wall. Phys Ter Sport 2017; 23:133-5. doi: 10.1016/j.ptsp.2016.09.002.
- Welsh P, Gryfe D. Atypical presentation of axillary web syndrome (AWS) in a male squash player: A case report. J Can Chiropr Assoc 2016; 60(4):294-8.
- Chen YW. Exercise-induced changes in inflammatory processes: İmplications for thrombogenesis in cardio-vascular disease. Ann Med 2014; 46(7):439-55. doi: 10. 3109/07853890.2014.927713.