Improving the Prognosis for Phthisis Bulbi Patients
By Neeti Solanki, Saumyendra Vikram Singh, Deeksha AryaAffiliations
doi: 10.29271/jcpsp.2021.10.1257
Sir,
Prosthetic rehabilitation of patients with phthisis bulbi is challenging, primarily due to reduced prosthetic space and corneal sensitivity. Sensitivity can cause difficulty in prosthesis fabrication; and inability of the patient to wear the prosthesis1 (Figure 1a). Surgical techniques to minimise sensitivity have their own complications.2,3 Therefore, a prosthetic technique, aimed at gradual desensitisation, and improving the esthetic outcome in cases of phthisis bulbi has been being discussed.
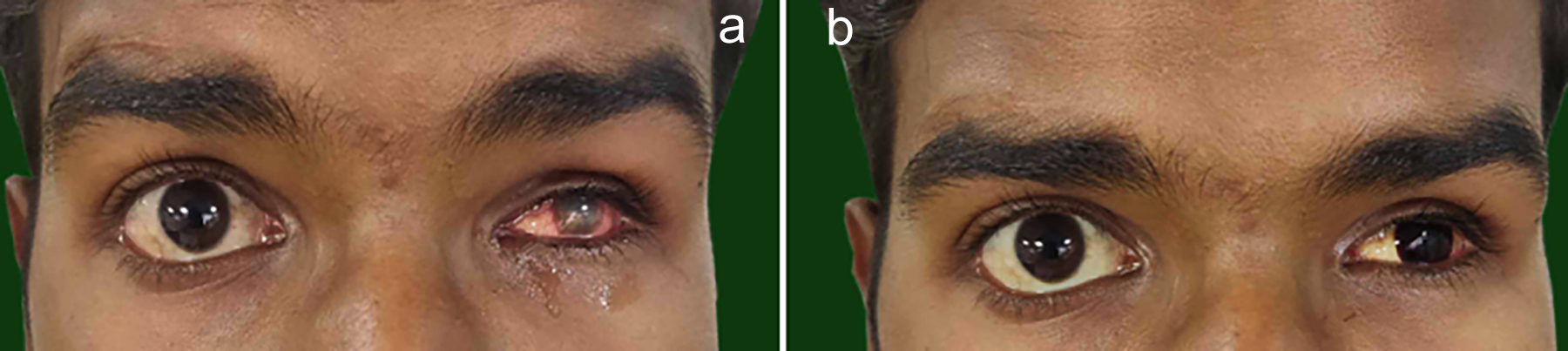 Figure 1: (a) Excessive corneal sensitivity associated with the phthisical eye. (b) Contact lens given to the patient for gradual desensitisation.
Figure 1: (a) Excessive corneal sensitivity associated with the phthisical eye. (b) Contact lens given to the patient for gradual desensitisation.
A 24-year male patient was referred for left prosthetic eye fabrication, who had presented with a history of trauma resulting in phthisis bulbi. Testing with a cotton wisp showed that the patient had sensitivity in this eye. To start with, a coloured rigid glass permeable (RGP) contact lens (Elite, Everclear) matching patient’s contralateral iris colour (Figure 1b) was selected. Patient was told to wear the contact lens for brief time periods initially. The time of wear was increased gradually until two weeks.
After this, patient’s affected eye was examined again for sensitivity. As the tolerance had improved, an ocular impression was made after anaesthetising the affected eye. Had excessive sensitivity been persistent, patient would have been instructed to increase lens wearing time for another two weeks. Impression was poured in type III dental stone (Kalabhai Kalstone, Karson Pvt. Ltd., Mumbai), to create a two-half mold, then wax was poured in this mold to fabricate a wax pattern for the prosthesis. Carving and contouring of the wax pattern was done to simulate the lost eye. After this, try-in was done to assess for fit, contour, comfort, size, support and movement. Acrylisation of the wax pattern was done in heat-cured tooth coloured acrylic resin (Heat Cure, Pyrax Polymars, India), matching the shade with the sclera of unaffected eye.
Margins were ascertained to be thin to avoid an over-bulging prosthesis. Prosthesis was checked for fit and contour, following which it was relined with permanent heat-cured soft reliner (Molloplast B, Detax, Germany) after reducing 1 mm circumferentially to improve retention and reduce discomfort (Figure 2a). Iris position was determined on scleral shell according to conventional techniques (Figure 2b). This portion of the prosthesis was formed with the initially used contact lens, which was adhered with cyanoacrylate to the shell, in previously determined position. Monopoly syrup was used to protect the surface and contact lens. After this, the final prosthesis was delivered (Figure 2c).
 Figure 2: (a) Margins of the prosthesis trimmed and relined with a permanent soft liner. (b) Iris positioning. (c) Final prosthesis with contact lens as the iris.
Figure 2: (a) Margins of the prosthesis trimmed and relined with a permanent soft liner. (b) Iris positioning. (c) Final prosthesis with contact lens as the iris.
Use of contact lens introduced an inceptive stimulus to gradually desensitise the patient. Using same contact lens as iris in the prosthesis, provided superior esthetics by minimising risk of a bulging over-contoured prosthesis, pre-empting excessive thinning of scleral shell, which can lead to fragility and show through. Use of permanent soft liner at the margins of the prosthesis, reduced discomfort and aided retention. However, this approach is technique-sensitive and time-consuming, with additional cost of the lens.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
NS: Conceptualisation, investigation, writing the original draft.
SVS: Formal analysis, methodology, writing, reviewing and editing.
DA: Supervision, validation, and visualisation.
REFERENCES
- Ding J, Chen T, Hou Z, Qin Y, Hao L, Li D. Cosmetic shell fitting over a sensitive cornea in mild phthisis bulbi using total conjunctival flap. Aesthetic Plast Surg 2013; 37(2): 398-401. doi: 10.1007/s00266-012-0003-2.
- Alino AM, Perry HD, Kanellopoulos AJ, Donnenfeld ED, Rahn EK. Conjunctival flaps. Ophthalmol 1998; 105(6):1120-3. doi: 10.1016/S0161-6420(98)96017-1.
- Gundersen T, Pearlson HR. Conjunctival flaps for corneal disease: Their usefulness and complications. Trans Am Ophthalmol 1969; 67:78-95. PMID:5381310.