Hypersensitivity Pneumonitis in a Pediatric Patient
By Madiha Naz, Shazia Parveen, Afsheen Asghar Khan, Fauzia ZafarAffiliations
doi: 10.29271/jcpsp.2021.06.735ABSTRACT
Hypersensitivity pneumonitis (HP) is a rarely diagnosed interstitial lung disease with variable manifestations. It results from repeated inhalation of certain antigens, e.g. mold, avian antigen, etc. in susceptible patients. The diagnosis is made by exposure history, relevant clinical presentation, and specific radiologic features. It is treated by avoidance of triggers and use of corticosteroids. We report a 7.5-year girl with HP. She was admitted for cough and severe respiratory distress.
Key Words: Hypersensitivity pneumonitis, Antigen, Allergy, Child.
INTRODUCTION
Hypersensitivity pneumonitis (HP), or extrinsic allergic alveolitis, is described as a complex syndrome with variable severity, diverse presentation, and disease course.1 It is an interstitial lung disease that results from repeated inhalation of certain organic or inorganic antigens, in susceptible patients. In most reported pediatric cases, common provocation agents include bird antigens, fungal aerosols and certain drugs.2 HP has been classified into acute, sub-acute, and chronic forms;3 but these are ill defined and there are no definite criteria. The diagnosis is established by documented exposure, relevant clinical signs and symptoms, and specific radiologic features. If high-resolution CT (HRCT) is inconclusive, then broncho-alveolar lavage (BAL) or lung biopsy is indicated.4 Treatment options include avoidance of triggering agent in all cases, and corticosteroids in some patients.5 The prognosis is excellent when if diagnosed and treated early. However, deaths from HP have been reported in children as well as adults.
CASE REPORT
A 7.5-year girl, presented with complaints of fever and severe respiratory distress. There was history of fever, gradual in onset, high grade, continuous, and associated with cough and respiratory distress. Cough was productive with white sputum, and there was history of similar complaints for the last 9 months. She also took anti-tuberculous treatment (ATT) for 7 months without being properly investigated. History of exposure to pigeon’s droppings for long time was positive.
 Figure 1: Chest X-ray showing fine reticulation and diffuse opacities in both lung fields.
Figure 1: Chest X-ray showing fine reticulation and diffuse opacities in both lung fields.
She was taking treatment from local doctors due to on/off respiratory distress; but did not improve, and was referred to us for further workup and management. She was febrile, having obvious respiratory distress, with subcostal and intercostal recessions. The vitals were: respiratory rate (RR) 80/min, heart rate (HR) 140/min, temperature 990 F, and blood pressure 100/60 mmHg, SPO2 was 55% in ambient air and raised to 92% with oxygen at 6 liter with nasal prongs. The weight and height were 11 kgs and 103 cm, respectively (both under 5th SD). Chest examination revealed bilateral coarse crepitations and reduced air entry on bases of lungs. Cardiovascular examination was normal. There was no visceromegaly. Other systems were normal. Laboratory investigations showed hemoglobin (Hb) of 13.0 g/dl, total leucocyte count (TLC) of 14,900/mm3 with neutrophils 90% and lymphocytes 9%. Routine biochemical investigations were normal. Erythrocyte sedimentation rate (ESR) was 6 mm/1st hr. IgE level was raised at 499.9 IU/ml. Chest X-ray (CXR) revealed fine reticulation and diffuse opacities throughout the lung. HRCT chest done initially revealed bilateral diffuse ground glass opacities with septal thickening involving both lung fields, mainly in centre with some areas of bronchial thickening and cavitation. Later, it repeated after 40 days and revealed bilateral diffusely scattered ground glass haze in lung fields almost in symmetrical pattern, suggestive of acute HP. The child was treated with oxygen, and antibiotics, which were later stopped and pulse therapy of methyl prednisolone, which was given initially, and later oral corticosteroids were started. Patient improved and was discharged with home advice of avoidance of pigeons, which is mandatory; and regular follow-ups were scheduled on weekly basis.
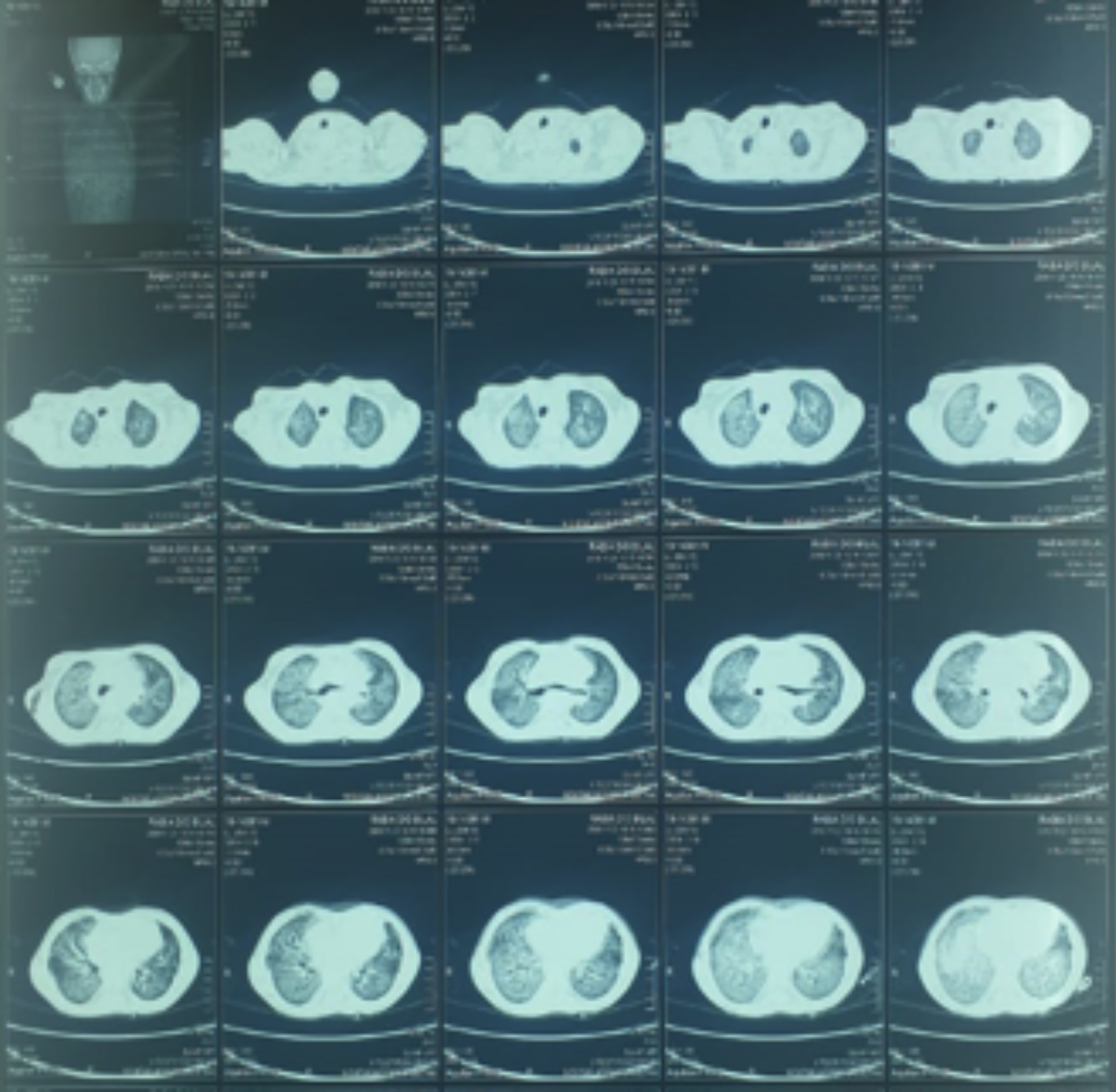 Figure 2: High-resolution CT showing bilateral diffuse ground glass haze in lung fields.
Figure 2: High-resolution CT showing bilateral diffuse ground glass haze in lung fields.
DISCUSSION
HP is an interstitial lung disorder recognised and reported rarely by pediatricians. It is recognised clinically by definite history of exposure to specific antigens with respiratory findings. Pediatric cases are rarely diagnosed or reported, so limited data is available and is largely based on few case reports and small series of patients. Till 2005, only 95 cases were reported.6 Although we report a female patient, slight male predominance was noted by Fink et al.6 In our patient, history of inhalation of avian antigen was evident. Many reported cases among children also had birds exposure.2,5Although cases reported include exposure to fungal aerosols. Nakshima et al. reported HP as a result of inhalation of isocyanates.7 Family history was negative in our case; although Fink et al. reported that many pediatric cases had positive family history.6 Pediatric patients are least suspected of having HP, and thus are under-reported and misdiagnosed. So any patient having favourable history should be investigated and managed appropriately. All the cases must be reported to increase knowledge regarding HP.
CONFLICT OF INTEREST:
All authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
MN: Conception and writing the article.
SP: Bibliography collection.
AAK: Critical revision of the article.
FZ: Final approval of the article.
REFERENCES
- Spagnolo P, Rossi G, Cavazza A, Bonifazi M, Paladini I, Bonella F, et al. Hypersensitivity pneumonitis: A comprehensive review. J Investig Allergol Clin Immunol 2015; 25(4):237-50; quiz follow 250.
- Nogueira R, Melo N, Novais E, Bastos H, Martins N, Delgado L, et al. Hypersensitivity pneumonitis: Antigen diversity and disease implications. Pulmonology 2019; 25(2):97-108. doi: 10.1016/j.pulmoe.2018.07.003.
- Riario Sforza GG, Marinou A. Hypersensitivity pneumonitis: A complex lung disease. Clin Mol Allergy 2017; 15:6.
- Federico MJ, Baker CD, Deboer EM, Halbower AC, Kupfer O, Martiniano SL, et al. Respiratory tract & mediastinum. In: Hay Jr William W, Levin MJ, Deterding RR, Abzug MJ, editors. Current Pent: Pediatrics. 24th ed. New York, NY: McGraw-Hill Education; 2018 cited 2020 Jan 10. Available from: accessmedicine.mhmedical.com/content.aspx?aid=1153308493
- Jędrych ME, Szturmowicz M, Bestry I, Kuś J. Hypersensitivity pneumonitis: Diagnostic criteria, treatment, prognosis and prevention. Med Pr 2016; 67(4):517-27. doi: 10.13075/ mp.5893.00406.
- Fink JN, Ortega HG, Reynolds HY, Cormier YF, Fan LL, Franks TJ, et al. Needs and opportunities for research in hypersensitivity pneumonitis. Am J Respir Crit Care Med 2005; 171(7):792-8. doi: 10.1164/rccm.200409-1205WS.
- Nakashima K, Takeshita T, Morimoto K. Occupational hypersensitivity pneumonitis due to isocyanates: Mechanisms of action and case reports in Japan. Industrial Health 2001; 39(3):269-79. doi: 10.2486/indhealth.39.269.