Challenges in the Management of Multiple Splenic Abscesses caused by Extensively Drug-resistant (XDR) Salmonella Typhi
By Ch. Muhammad Zubair1, Muhammad Musa Haider2, Muhammad Ameer Musa1, Zulfiqar Ali Khosa3Affiliations
doi: 10.29271/jcpsp.2021.07.855ABSTRACT
Extensively drug-resistant (XDR) typhoid emerged in Hyderabad, Pakistan in 2016. It spread regionally and globally due to fast travelling. An immuno-competent young male referred by general practitioner, was diagnosed and managed as XDR salmonella typhi with multiple splenic abscesses. We faced challenges in its management, like little suspicion of potentially lethal disease; non-availability of evidence-based medicine and further delay in diagnosis as he was already on antibiotics therapy. Patient was diagnosed by radiology and blood cultures. In our case, option of conservative treatment with sensitive antibiotics (azithromycin and meropenem) was successful, though with increased hospital stay. There is no data on treatment duration and choice between two sensitive antibiotics or both in combination. In the present situation, sensitisation of clinicians to salmonella drug resistance, rational use of antibiotics and prompt public health awareness is the need of the day, especially in endemic areas.
KEY WORDS: Extensively drug-resistant (XDR) typhoid,Splenic abscesses, Azithromycin, Meropenem.
INTRODUCTION
Typhoid splenic abscess is a life-threatening condition with high morbidity and mortality, even if appropriately managed. It became a global health issue due to extensively drug-resistant (XDR) salmonella typhi. XDR salmonella was first observed in Hyderabad, Pakistan in 2016. In a span of two and half years duration in ten hospitals of Karachi, 9,591 typhoid positive cases were recorded; out of which, 6,107 were reported as XDR typhoid.1
XDR typhoid with splenic abscesses is clinically lethal entity with narrow therapeutic range. Our patient of XDR positive typhoid fever with multiple splenic abscesses was previously healthy. Self-medication and excessive use of antibiotics by general practitioners resulted in his potentially lethal condition.
The goal of this presentation is to increase awareness of the health stakeholders and practising physicians about the XDR positive typhoid, and compel them for appropriate and judicious use of antibiotics, especially in our country, where antibiotics are sold over-the-counter.
CASE REPORT
An 18-year previously healthy, immunocompetent, non-addicted, non-diabetic male with no significant travel history, was referred by a general practitioner, with one month history of fever with rigors, anorexia and pain in left upper quadrant of abdomen. He was on medication for the last one week and clinically not responding to the treatment. On physical examination, he looked toxic with pulse of 84/min (relative bradycardia), febrile (102oF), blood pressure of 110/80 mm of Hg, respiratory rate, 18 breaths/min and no lymphadenopathy. Systemic examination revealed mild tenderness on deep palpation in left hypochondrium, otherwise abdomeninal examination was normal. Provisional diagnosis of ‘pyrexia of unknown origin’ was made. Preliminary investigations like complete blood count (CBC), malaria parasite, urinalysis and chest X-Ray revealed no abnormality.
Widal test was positive (O titer 1:160, H titer 1:40). Ultrasonography showed evidence of mild splenomegaly, multiple hypo-echoic areas in spleen, mild ascites and mesenteric lymphadenopathy. The findings were corroborated by computed tomography (CT) of the abdomen (Figures 1 and 2). C-reactive protein (CRP) was 43 mg/dl. Blood culture and sensitivity were not sent for the reason, because he was already on antibiotic treatment. Echocardiography was performed to rule out infective endocarditis for possible infective emboli to spleen.
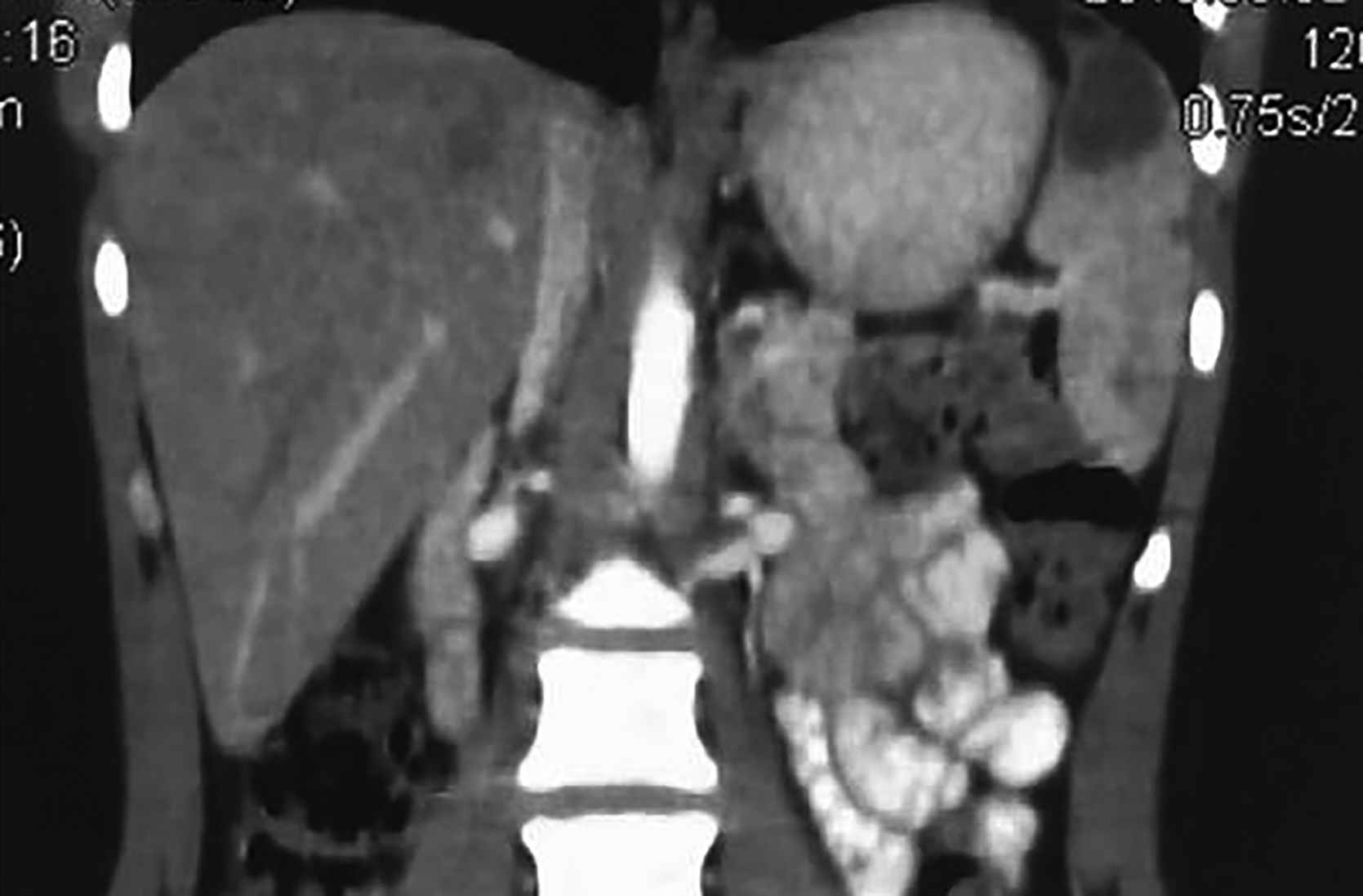 Figure 1. Coronal view of CT scan showing multiple hypodense areas in the spleen, largest one measuring 3.0×2.7 cm. Mild ascites is seen.
Figure 1. Coronal view of CT scan showing multiple hypodense areas in the spleen, largest one measuring 3.0×2.7 cm. Mild ascites is seen.
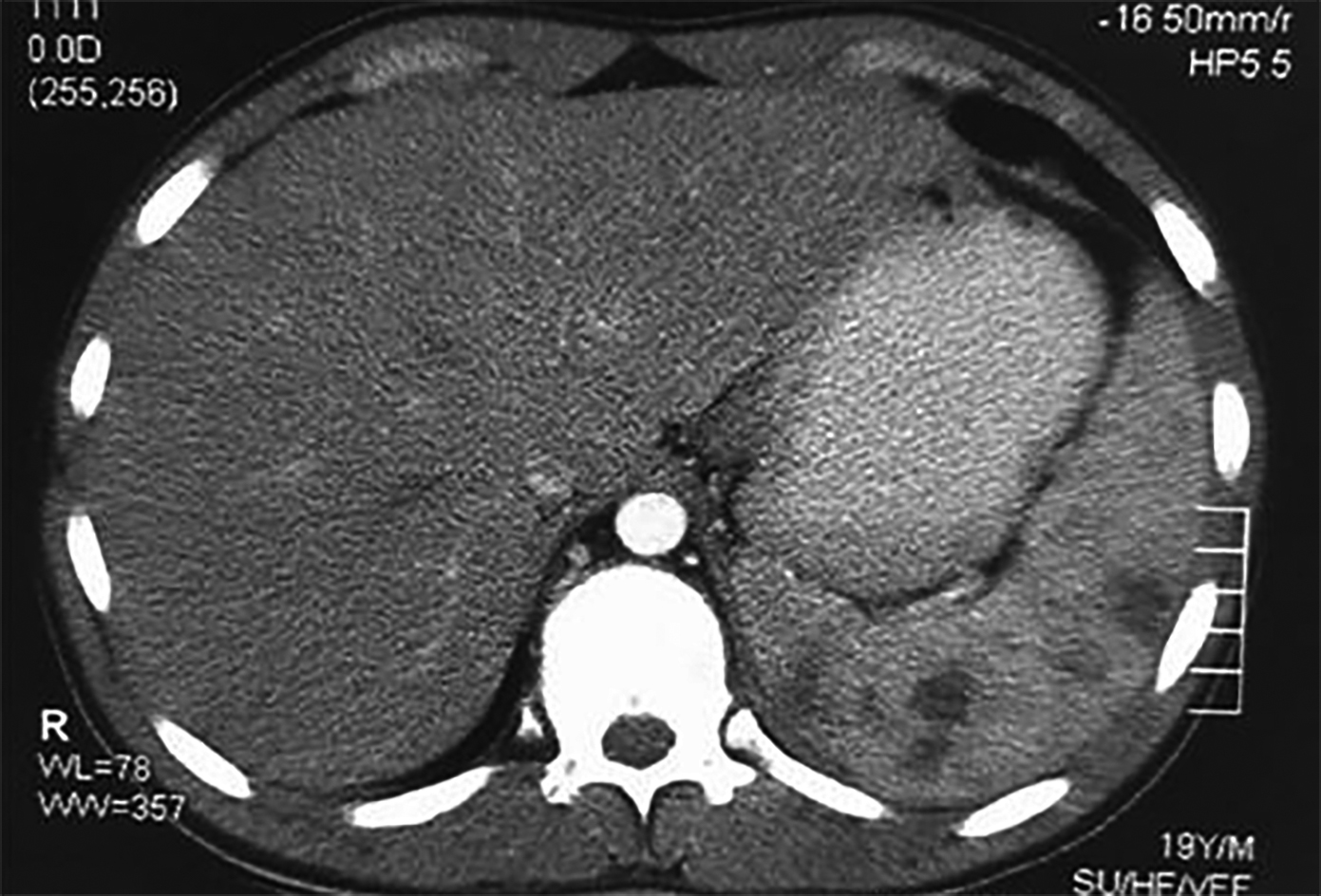 Figure 2. Axial view of CT scan showing multiple hypodense areas in the spleen, largest one measuring 3.0×2.7 cm. Mild ascites is seen.
Figure 2. Axial view of CT scan showing multiple hypodense areas in the spleen, largest one measuring 3.0×2.7 cm. Mild ascites is seen.
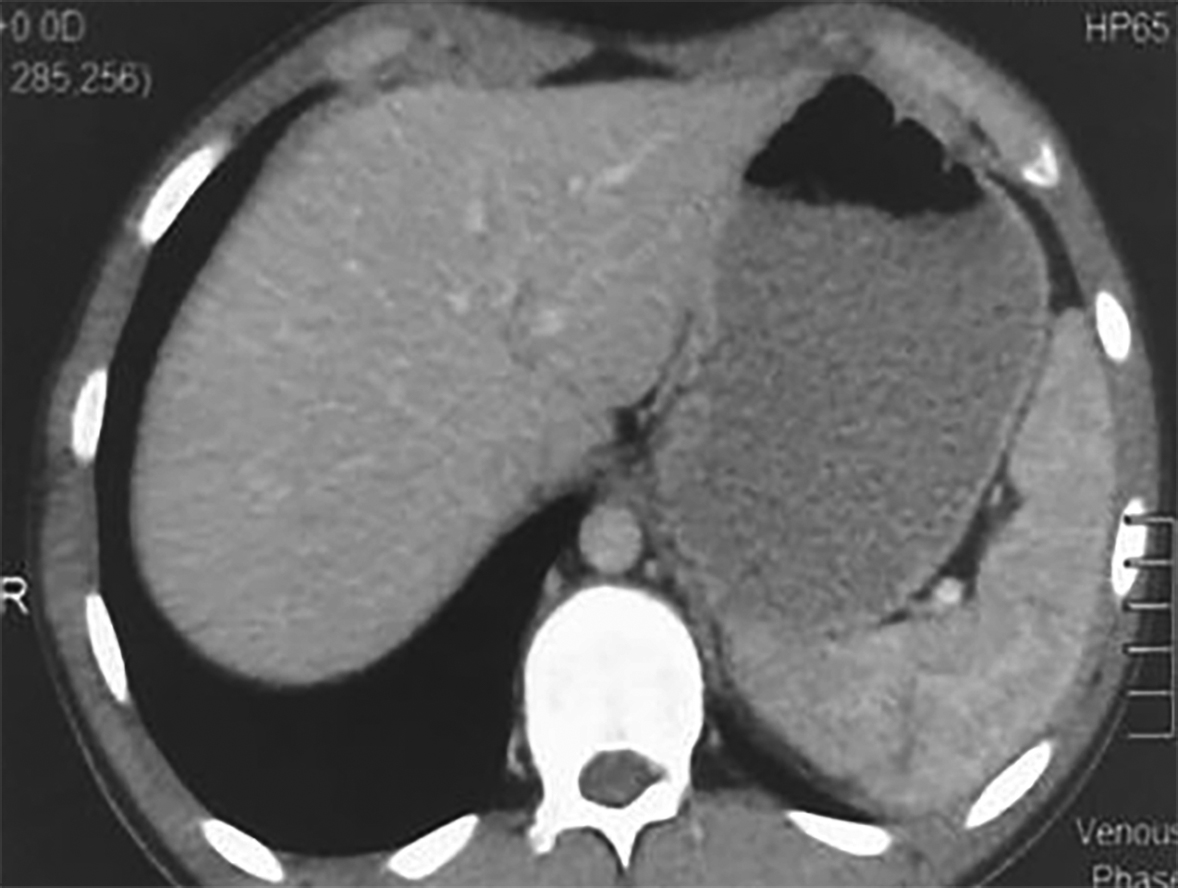 Figure 3. Axial view of CT scan after treatment showing tiny hypodense areas in the spleen, suggestive of healing. No ascites or lymphadenopathy is seen.
Figure 3. Axial view of CT scan after treatment showing tiny hypodense areas in the spleen, suggestive of healing. No ascites or lymphadenopathy is seen.
After 72 hours without antibiotics, blood was sent for culture and drug sensitivity testing. The findings showed XDR salmonella typhi, sensitive to azithromycin and meropenem. Multidisciplinary approach by involving surgeon, infectious disease specialist, and radiologist was adopted. The plan for medication was made after preliminary antibiotic test dose. After five days of treatment, patient became afebrile and general well being improved. Repeated ultrasound with one week treatment of both antibiotics (azithromycin and meropenem) revealed improvement in the size of splenic abscesses, disappearance of mild ascites and normalisation of mesenteric lymph nodes. The same treatment was continued for one more week and azithromycin alone for further two weeks. Sonography and CT findings of spleen became normal (Figure 3). Patient improved and was discharged with advice to remain in follow-up for at least six months. At five months of regular follow-up, patient remained asymptomatic.
DISCUSSION
Reduced susceptibility to major antibiotics in salmonella typhi remains a wide-spread public health problem in Asia, Africa and Oceania. In modern era of fast travelling, global transmission of resistant organism is observed. XDR typhoid was first reported in Sindh province of Pakistan in 2016 and its rapid spread was noticed regionally and internationally. Six international travel-associated cases of XDR typhoid were also reported in 2018; one in the United Kingdom and five in the United States of America.2
The XDRTyphoid is defined as extensive resistance of salmonella typhi to five major groups of antibiotics; first line (chloramphenicol, ampicillin, trimethoprim-sulfamethoxazole), second line fluoroquinolones), and third generation cephalosporin antibiotics, while resistance to all drugs is known as pan-drug resistant. A recent study from southern Pakistan shows incidence of XDR typhoid to be 3.7%.3 It has the potential to spread globally by replacing less resistant strains where they are endemic. The incidence of splenic abscesses in typhoid fever has been reported in between 0.29 to 2%cases. In these patients, certain risk factors like haemoglobinopathies and immunosuppression are usually present.4 Splenic abscesses with XDR-typhoid have not yet been reported in literature.
Our patient of low income class was an immunocompetent young male with no significant past history of any disease or travel. His nonspecific clinical presentation, poor early suspicion by general practitioner, and absence of adequate health facilities led to delay in accurate diagnosis. Lack of knowledge of XDR typhoid organism, resulted in blind treatment with easily available ceftriaxone. Poverty, poor sanitation and unhygienic conditions further augmented the predisposing factors.5
Treatment of XDR typhoid splenic abscesses is difficult as no data is available regarding management of this potentially lethal disease. For typhoid splenic abscess, splenectomy, percutaneous abscess drainage, combined with antibiotics and treatment with antibiotics alone remain choice of many physicians but still are controversial as no randomised control trial has been conducted. In addition, there is no consensus in choice of antibiotics and its duration.6 our patient responded dramatically with sensitive antibiotics treatment with no need of percutaneous drainage or splenectomy. The potentially lethal disease was controlled by antibiotic regimen.
There is a need in present emerging situations of sensitisation of general practitioners and clinicians to the knowledge of antimicrobial drug resistance in typhoid, multidrug resistance (MDR) and XDR, and rationale use of antibiotics is mandatory in areas specially where disease burden is high. Careful, individualised, and rationalised management of patients is essential. A prompt public health response by local government is also needed in endemic regions of disease and even in areas where XDR typhoid is not endemic, with school and community awareness campaign on water and sanitation hygiene (WASH) improvement. Strengthening surveillance of typhoid fever with mass typhoid vaccination, distribution of chlorine tablets, restriction of over-the-counter and easy availability of only sensitive antibiotics along with well-functioning laboratory system (for antibiotic susceptibility testing and possibly whole-genome sequencing) are imperatives for the effective control. Local and international pre-travel vaccination and guidance for travelers to endemic areas are immediately needed. Randomised control trials are the need of hour for the optimal treatment of XDR typhoid and its complications.
Early suspicion, correct diagnosis and appropriate management are the key to successful treatment of XDR typhoid splenic abscesses. Radiology along with blood/pus culture and drug sensitivity testing are major diagnostic tools for diagnosis. Conservative treatment with only sensitive antibiotics may prove to be successful for this potentially deadly disease.
PATIENT’S CONCENT:
Informed consent was obtained from the patient to publish the data concerning his case report.
CONFLICT OF INTEREST:
Authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
CMZ: Conception of work, first draft, acquisition and analysis of data, final approval of version to be published.
MH: Revised and critically analysed the content.
MAM: Evaluation of the case, detailed history taking and investigation and reporting the investigations.
ZAK: Final approval of the version to be published.
REFERENCES
- Extensively Drug-Resistant Typhoid fever in Pakistan. Alert-Level 2, practice enhances precautions. World Health Organization 2018; (https://wwwnc.cdc.gov/travel/notices/ alert/xdr-typhoid-fever-pakistan).
- Emergencies preparedness response. Typhoid fever, Islamic republic of Pakistan.
- Shaikh AA, Shaikh A, Tahir A. Antimicrobial resistance trends of typhoidal salmonellae in southern Pakistan. RMJ 2019; 44(1):7-10.
- Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance and antimicrobial management of invasive salmonella infections. Clin Microbiol Rev 2015; 28:901-7.
- Extremely drug-resistant typhoid in south Asia. www.thelancet.com/infection Vol 18 September 2018. Dated 15th Nov, 2019.
- Khan FY. Typhoid splenic abscess: A case report and literature review, Int J Infect; 6(1):e87136.doi: 10.5812/ iji.87136.