A Rare Case of Primary Paratesticular Adult Ganglioneuroma
By Yavuz Burak Kara1, Ekrem Akdeniz2Affiliations
doi: 10.29271/jcpsp.2021.07.875Sir,
A 25-year man presented with painless left scrotal swelling of three years’ duration. Physical examination revealed a left paratesticular mass. Alpha-fetoprotein (AFP) and beta human chorionic gonadotropin (β-HCG) were within normal ranges. Scrotal ultrasonography revealed a 40×30×30 mm left-sided paratesticular lesion (Figure 1a). Chest radiography was normal. Scrotal exploration was undertaken, and the paratesticular mass was excised while preserving the testis (Figure 1b). An encapsulated lesion was identified during gross examination. Histopathologically, this consisted of spindle cell lesion containing nodules of ganglion cells with abundant eosinophilic cytoplasm and eccentric, round to oval, vesicular nuclei embedded in the stroma (Figure 2a and 2b). Postoperative abdominal-pelvic magnetic resonance imaging was negative, and the final diagnosis was maturing type primary paratesticular adult ganglioneuroma (PPAG). No clinical, laboratory or radiological pathologies were observed at follow-up visits in the postoperative second year.
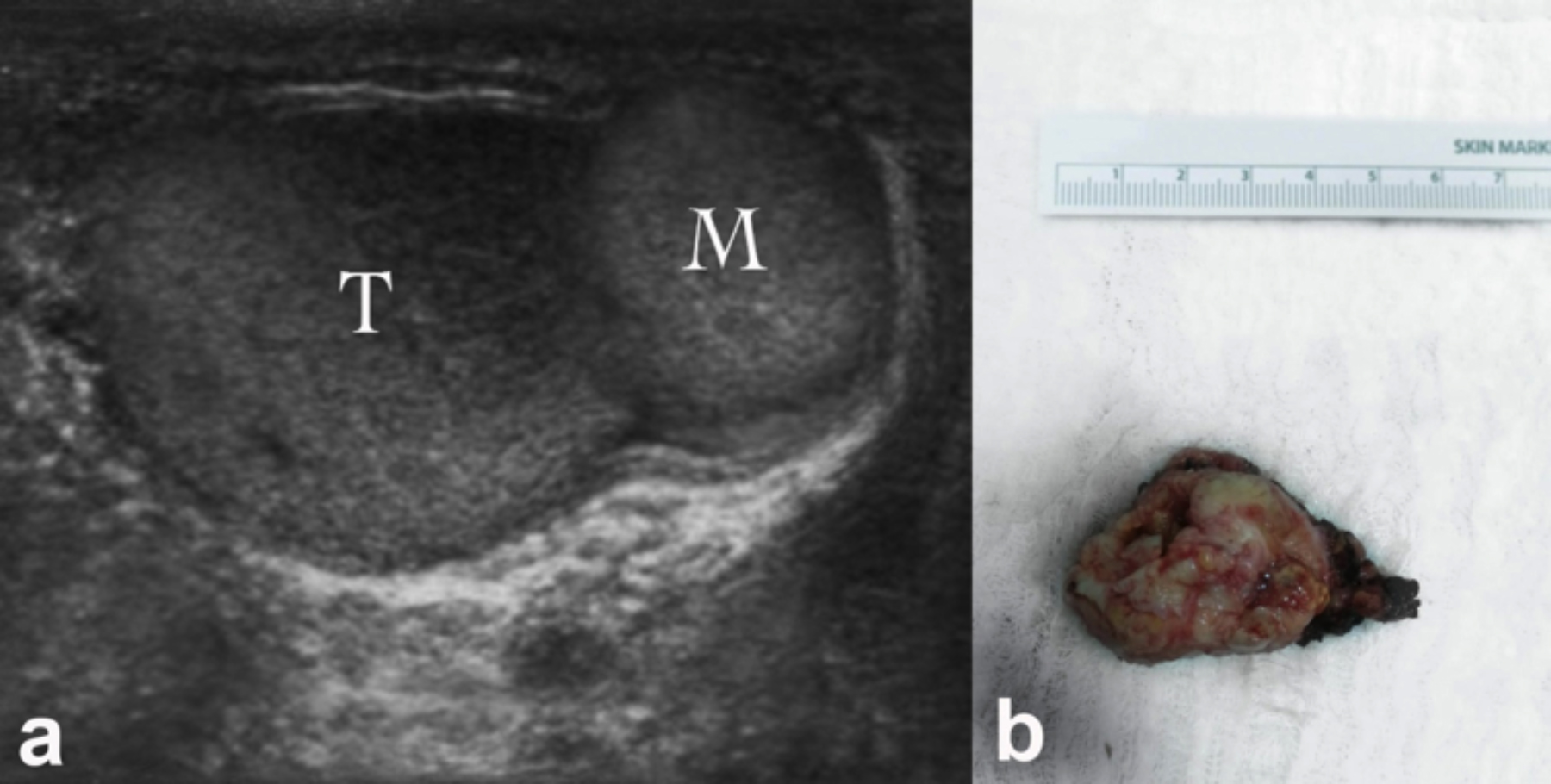 Figure 1: Ultrasonographic (a) and postoperative (b) view of the paratesticular mass (M: Mass, T: Testis).
Figure 1: Ultrasonographic (a) and postoperative (b) view of the paratesticular mass (M: Mass, T: Testis).
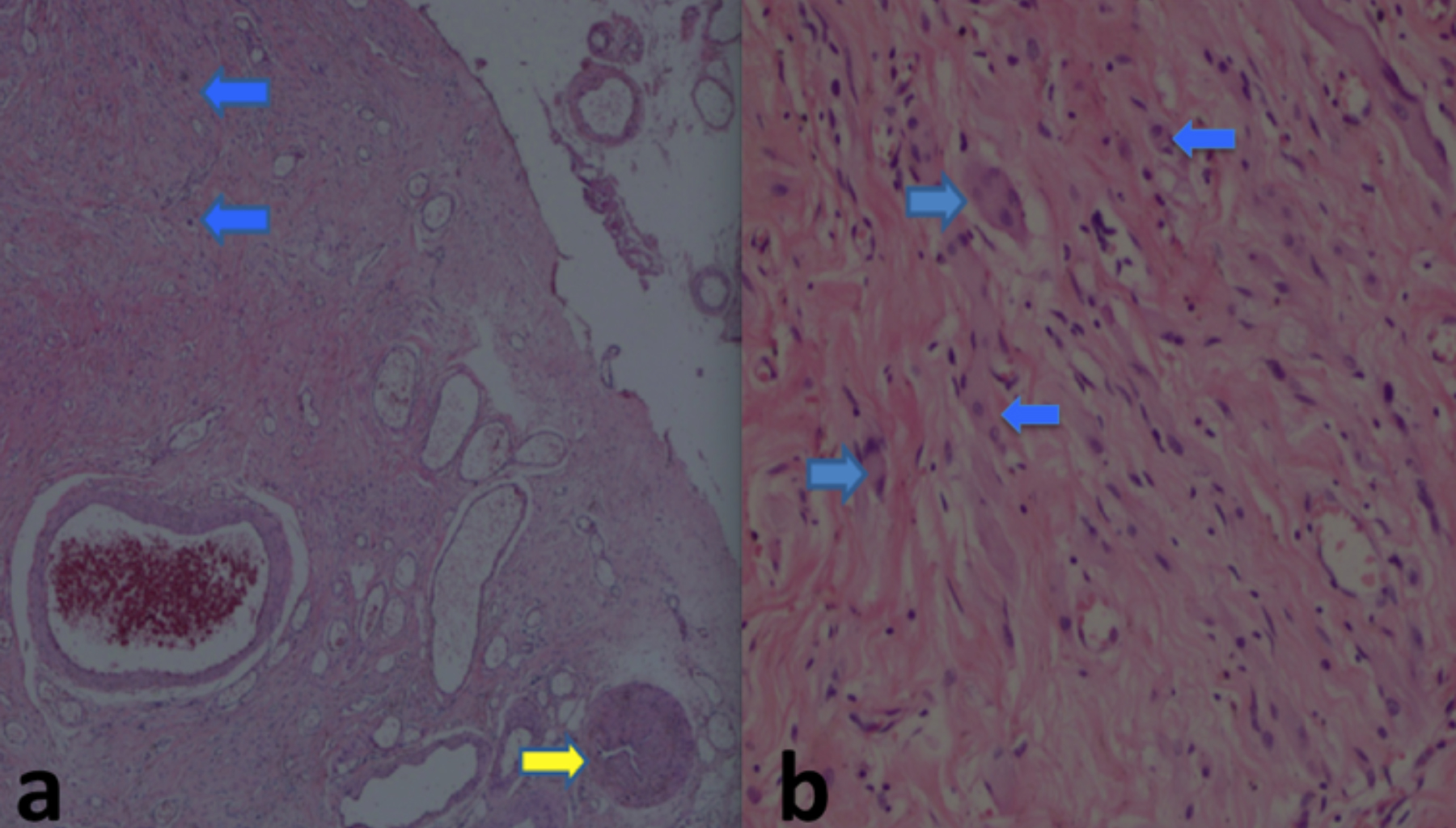 Figure 2: Ductus deferens and tumoral formations in the paratesticular area [a: Ductus deferens (yellow arrow) and ganglion cell nodules (blue arrows) (HE, ×40)]. b: Ganglion cells with eosinophilic cytoplasm, and eccentric ovoid nuclei (blue arrows) (HE, ×200).
Figure 2: Ductus deferens and tumoral formations in the paratesticular area [a: Ductus deferens (yellow arrow) and ganglion cell nodules (blue arrows) (HE, ×40)]. b: Ganglion cells with eosinophilic cytoplasm, and eccentric ovoid nuclei (blue arrows) (HE, ×200).
Ganglioneuroma is a benign tumour of the sympathetic nervous system, composed of gangliocytes, Schwann cells and mature stroma. It is usually observed in children and young adults.1 The most common non-cranial locations are the posterior mediastinum, retroperitoneum, and adrenal glands.2 Ganglioneuromas in the paratesticular region are rare in adults. The English-language medical literature contains only two previous reports of ganglioneuroma, a childhood disease, in the paratesticular region in adult patients.3, 4
Curative treatment of paratesticular ganglioneuroma consists of total surgical excision. A very small number of non-cranial ganglioneuromas have been shown to possess the capacity to metastasise, and this entity is also capable of exhibiting delayed transition to neuroblastoma.1-5 The most important prognostic factor is that the surgical margins should be negative. Surgical excision of ganglioneuroma must be well planned, and care must be taken during clinical follow-ups. If recurrence occurs at follow-up, a wide area of surgical excision must be planned in order to prevent malignancy development.
The behaviour of paratesticular ganglioneuromas may vary in terms of aggressiveness, due to the rich blood and lymphatic drainage in the paratesticular region; and the fact that histologically, these consist of several cell types. A standard follow-up course is required in such cases, and the potential transition of PPAG to malignancy in the long-term must also be kept in mind. However, more reports are needed in order for this evaluation to be possible.
CONFLICT OF INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
BYK, EA: Substantial contributions to the conception or design of the work, the acquisition, analysis, or interpretation of data for the work, drafting the work and revising it critically for important intellectual content, and final approval of the finished version.
REFERENCES
- Hanna SJ, Muneer A, Coghill SB, Miller MA. Ganglio-neuromas in the adult scrotum. J R Soc Med 2005; 98(2): 63‐4. doi: 10.1258/jrsm.98.2.63-a.
- Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglio-neuroma: Radiologic-pathologic correlation. Radiographics 2002; 22(4):911‐34. doi: 10.1148/radiographics.22.4.g02jl 15911.
- Pardalidis NP, Grigoriadis K, Papatsoris AG, Kosmaoglou EV, Horti M. Primary paratesticular adult ganglioneuroma. Urology 2004; 63(3):584-5. doi: 10.1016/j.urology.2003. 10.068.
- Jaiprakash P, Rao AC. Primary paratesticular ganglioneuroma: A rare case in an adult. Turk Patoloji Derg 2012; 28(2):165-7. doi: 10.5146/tjpath.2012.01117.
- Kulkarni AV, Bilbao JM, Cusimano MD, Muller PJ. Malignant transformation of ganglioneuroma into spinal neuroblastoma in an adult. J Neurosurg 1998; 88(2): 324-27. doi: 10.3171/jns.1998.88.2.0324.