A Case of Lung Abscess Mimicking Lung Cancer
By Nevhiz GundogduAffiliations
doi: 10.29271/jcpsp.2021.11.1366ABSTRACT
The radiological appearance of lung abscess is nonspecific and can masquerade as a mass lesion during the early phase. The treatment is primarily medical, but surgical treatment is necessary when the size is larger than 6 cm and when patients show any indications of massive hemoptysis, empyema, bronchial obstruction, and risk of cancer or when the medical treatment fails.
A 55-year male patient presented with complaints of back pain over a period of two years with additional complaints such as fatigue and coughing up of blood. On physical examination, crackles in the right upper zone of his lungs were observed. Chest x-ray revealed a cavitary lesion in the right upper zone. The patient was taken to the hospital with preliminary diagnosis of lung cancer. A fiberoptic bronchoscopy (FOB) was performed resulting in a preliminary diagnosis of malignancy. No endobronchial lesion was detected in FOB. The bronchoalveolar lavage (BAL) culture was negative. The BAL cytology was also benign. As a result, oral levofloxacin treatment was started. During follow-up examination, a partial reduction in the size of cavity was observed. As a result of this observation, PET-CT was ordered. According to the results, 18F-fluorodeoxyglucose (FDG) uptake of the level (maximum standardised uptake value [SUVmax]: 10.9) suspicious for malignancy was noted in the right hilar lymph node associated with irregular lobulated mass, which was considered to be associated with the pleura in the posterior segment of the right upper lobe. The patient was taken for surgery in light of these findings. The pathological results were consistent with abscess. The patient has no complaints six months after the surgical operation.
Key Words: Lung abscess, Cavitary lesion, Lung cancer, PET scan.
INTRODUCTION
The pulmonary abscess typically produces a cavitary lung lesion and is at limited area of necrosis containing purulent material, usually larger than 2 cm in diameter and formed within the lung parenchyma by pulmonary infection. The cavity often shows air-fluid level.1 Despite the advances in antibiotic treatment and other treatment options and a decrease in terms of incidence and mortality rates, it still has a mortality rate of 15-20%.2 The radiological appearance is nonspecific and may mimic a mass lesion during the early period, and followed by a cavitary appearance with air-fluid level as necrosis of the lung parenchyma develops. Lung abscesses are usually seen in the posterior segments of right upper lobe or superior segments of lower lobes of both the lungs. The treatment is primarily medical but surgical treatment is considered to be necessary when the size is larger than 6 cm and when patients show any indications of massive hemoptysis, empyema, bronchial obstruction, and clinical suspicion of cancer or when the medical treatment fails.3
CASE REPORT
A 55-year male patient presented to our hospital with complaints of back pain, fatigue, and coughing up of blood. He had been smoking for 15 years. The patient was a professional baker. On physical examination, crackles in the upper zone of his right lung were observed. The oxygen saturation on room air was 95%. His pulse was 75 beats/min; whereas, his blood pressure was 130 / 70 mmHg. His body temperature was 36.7°C. His chest X-ray showed cavitary lesion in the upper zone of right lung (Figure 1). The laboratory results indicated white blood cell count of 11,000 /uL and his C-reactive protein (CRP) was 33 mg/l. The patient was brought to the hospital with a preliminary diagnosis of lung cancer. Clarithromycin 500 mg, b.i.d. was started considering the possibility of tuberculosis due to the presence of cavitary lesion. His sputum was sent for culture and acid-fast bacillus (AFB) smear. His sputum AFB returned negative three times. There was no growth in his sputum culture. The patient also had no fever during the follow-up examinations; therefore, fiberoptic bronchoscopy (FOB) was performed with the preliminary diagnosis of malignancy. No endobronchial lesion was detected in his FOB. Meanwhile, bronchoalveolar lavage (BAL) was performed and the culture of the lavage was negative. BAL cytology was benign. The patient was followed up with oral levofloxacin treatment; and afterwards, the observed cavity became smaller, but it was still present. During this period, a consolidated area of irregular air densities with an approximate dimension of 43×35×40 mm was observed in the posterior segment of right upper lobe following thoracic CT (Figure 2). The patient also underwent PET-CT. The PET results suggested increased FDG uptake in the right hilar lymph node, indicating malignancy associated with an irregular mass-like lesion in the right upper lobe. It was considered to be associated with the pleura in the posterior segment of the right upper lobe and the lobulated contours were found to be related to the hilum medially. The observed maximum standardised uptake value (SUVmax) was 10.9. In the light of these results, the patient was taken to surgery. During the surgical operation, right upper lobectomy was performed and right hilar lymph node was removed. Following the pathological examination, diffuse chronic active inflammation together with large areas of suppurative inflammation as well as dense fibrosis and focal anthracosis were encountered (Figure 3). The patient has no ongoing complaints during the postoperative follow-up examinations even after six months.
 Figure 1: Chest X-ray showing cavitary lesion in the upper zone of right lung with air-fluid level.
Figure 1: Chest X-ray showing cavitary lesion in the upper zone of right lung with air-fluid level.
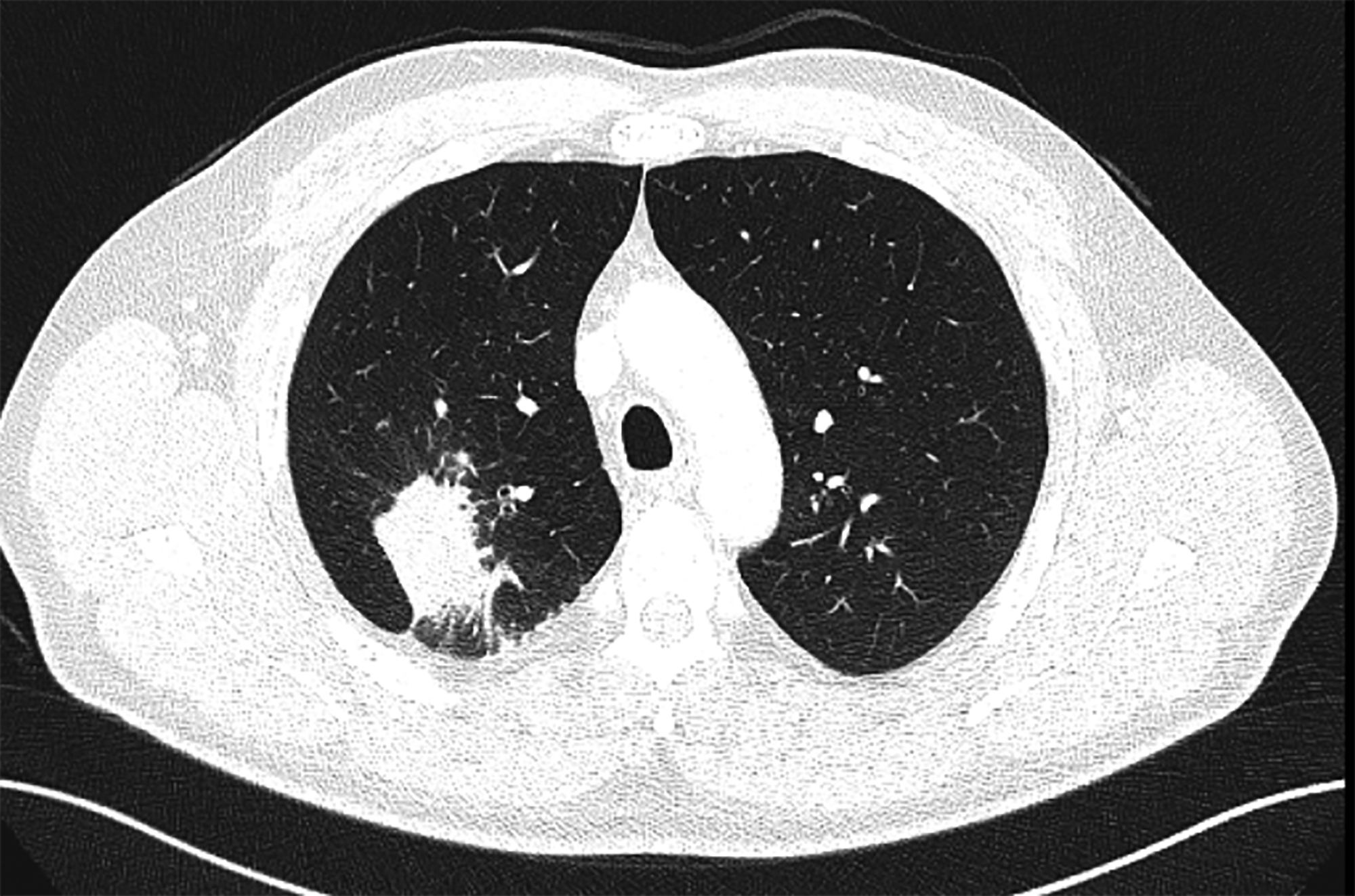 Figure 2: Axial image of thoracic CT scan showing an area of consolidation in the posterior segment of right upper lobe of lung.
Figure 2: Axial image of thoracic CT scan showing an area of consolidation in the posterior segment of right upper lobe of lung.
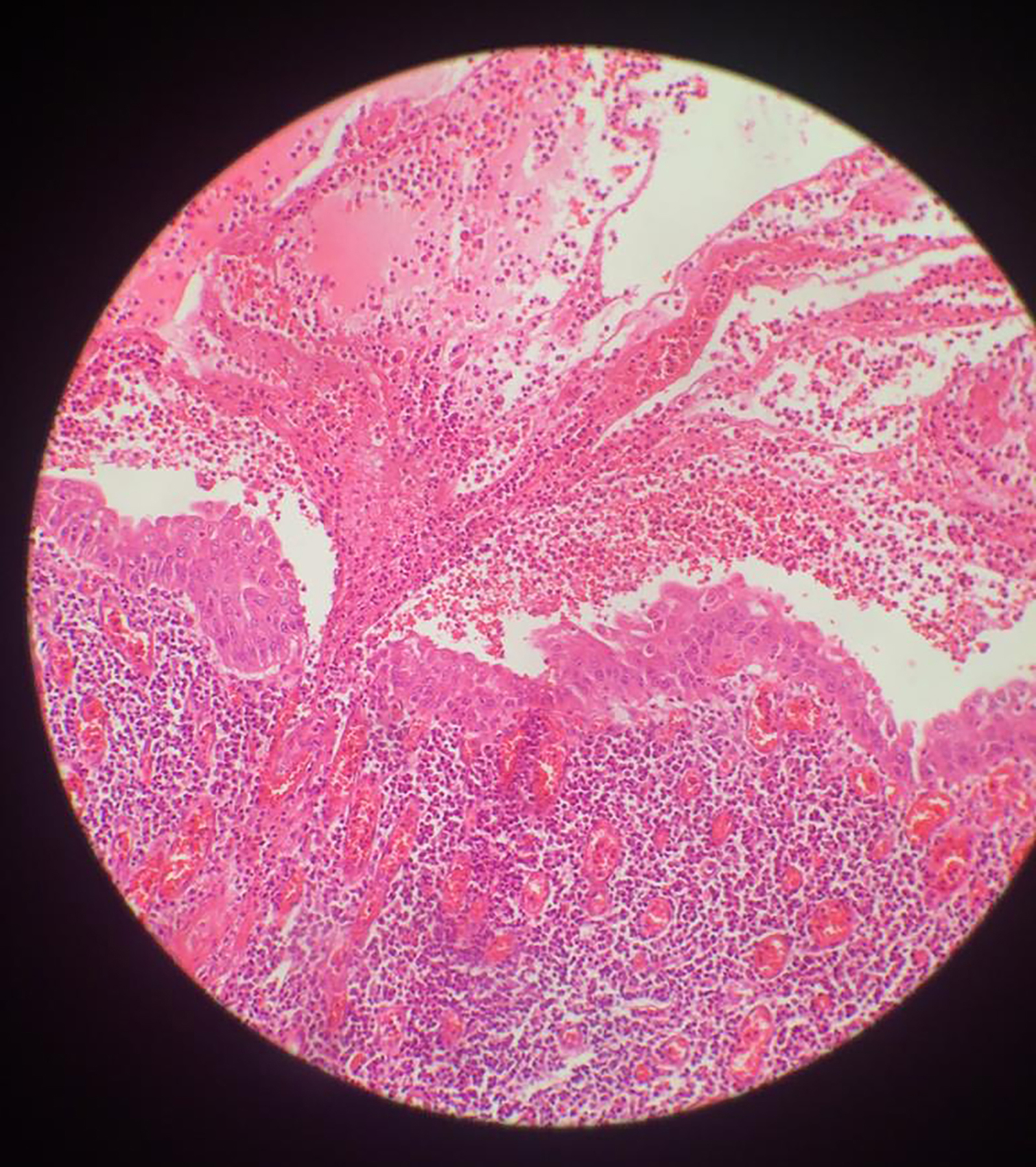 Figure 3: Histopathology shows dense mixed inflammatory cell infiltration in the wall and lumen of small bronchi. No evidence of dysplasia or malignancy is seen. (H&E, ×200).
Figure 3: Histopathology shows dense mixed inflammatory cell infiltration in the wall and lumen of small bronchi. No evidence of dysplasia or malignancy is seen. (H&E, ×200).
DISCUSSION
There are many differential diagnoses of lung abscess in the literature. Infections include tuberculosis, fungal infections, histoplasmosis, actinomycosis and parasitic infections such as amoebic abscess, and infected lung hydatid cyst, cavitary carcinoma, cystic lung diseases, infected emphysematous blebs, infected bronchogenic cysts, lung sequestrations, and granulomatous diseases such as Wegener's granulomatosis.3 In this particular case, we initially thought of lung cancer because of the persistence of the complaints over a 2-month period and due to the absence of fever. Therefore, bronchoscopy was performed during the early period. His bronchoscopy did not reveal any endobronchial lesions. His bronchial lavage was taken from the right upper lobe. The bronchial lavage culture was found to be negative. Meanwhile, AFB result was also negative. His bronchial lavage cytology was benign. The patient was followed-up with these findings. During the follow-up examinations, the cavitary lesion became smaller but still it did not disappear completely. The absence of growth in sputum and bronchial lavage cultures also compelled us to think about the possibility of malignancy.
When the primary causes of lung abscess are deliberated, in about 80-90% of the cases, it is because of anaerobic bacteria. Peptostreptococcus, microaerophilic streptococcus, bacteroides fragilis, and fusobacterium nucleatum are considered as primary culprits.1 Had an anaerobic culture been taken in our case, we could have reached to the correct diagnosis. Since the patient had no fever during the follow-up examinations and his CRP did not increase considerably, thus the patient underwent PET-CT to exclude the diagnosis of lung cancer. PET results showed increased FDG uptake in the right hilar lymph node and lung lesion with SUVmax of 10.9. The contours of the lung lesion were irregular and the SUVmax was at a level suspicious for malignancy necessitated biopsy of the lesion. Since the patient did not have any endobronchial lesion in his previous bronchoscopy, thoracotomy was planned and right upper lobectomy was performed and right hilar lymph node was also removed. The pathology results were consistent with the diagnosis of lung abscess. Surgical management of uncomplicated lung abscesses is rare; it is done if it is larger than 6 cm, and if there is massive hemoptysis, empyema, bronchial obstruction, clinical suspicion of cancer or failure of medical treatment.3 In this case, history of hemoptysis was present, but after the patient was admitted to the hospital, there was no hemoptysis and the size of the cavity was reduced to less than 2 cm with treatment, but lobectomy was performed due to the suspicion of malignancy, especially on PET CT report.
In 2009, a similar case was presented in Japan and a diagnosis was not reached after bronchoscopy. As a result of this particular presentation, and because of suspicion on PET, thoracotomy was performed for 2.5 cm lesion and the pathological diagnosis was consistent with lung abscess.4
On the contrary, in another published case, a 55-year patient with complaints of cough, hemoptysis and back pain for two months, which were similar to our case, lung, liver, bone and skin abscess lesions were observed. The bronchoscopy performed on this patient also had shown no endobronchial lesion, and bronchial lavage was found to be benign. But, unlike our study, the needle aspiration biopsy was consistent with epidermoid carcinoma.5 Hence, it is always advisable to approach such cases judiciously and meticulously.
In summary, this case study is presented to share our experience with the diagnosis and treatment of a case of lung abscess, which was originally thought to be lung cancer.
PATIENT’S CONSENT:
Informed consent was obtained from the patient before enrollment in the study.
CONFLICT OF INTEREST:
The author declared no conflict of interest.
AUTHOR’S CONTRIBUTION:
NG: Protocol/project development, data analysis, manuscript writing.
REFERENCES
- Yu H. Management of pleural effusion, empyema, and lung abscess. Semin Intervent Radiol 2011; 28(1):75-86. doi: 10.1055/s-0031-1273942.
- Hirshberg B, Sklair-Levi M, Nir-Paz R, Ben-Sira L, Krivoruk V, Kramer MR. Factors predicting mortality of patients with lung abscess. Chest 1999; 115(3):pp.746-50. doi: 10.1378/ chest.115.3.746.
- Çobanoğlu U, Deveci A. Akciğer Absesi. Van Tıp Dergisi 2007; 14(4):120-6.
- Kamiya K, Yoshizu A, Misumi Y, Hida N, Okamoto H, Yoshida S. Lung abscess which needed to be distinguished from lung cancer; report of a case. Kyobu Geka 2011; 64(13):1204-7.
- Dursunoğlu N, Başer S, Evyapan F, Kıter G, Ozkurt S, Polat B, et al. A squamous cell lung carcinoma with abscess-like distant metastasis. Tüberk Toraks 2007; 55(1):99-102.